| Revision as of 05:26, 5 February 2008 view sourceBackin72 (talk | contribs)5,347 edits Undid revision 189184169 by Mccready (talk) - rv; redundant (See talk)← Previous edit | Revision as of 05:46, 5 February 2008 view source Backin72 (talk | contribs)5,347 edits →Evidence-based medicine: restore a bunch of V RS's that another editor inappropriately removed from this sectionNext edit → | ||
| Line 277: | Line 277: | ||
| For ], a systematic review of the best 5 ] available found mixed results.<ref name="pmid17189243">{{cite journal |author=Mayhew E, Ernst E |title=Acupuncture for fibromyalgia--a systematic review of randomized clinical trials |journal=Rheumatology (Oxford, England) |volume=46 |issue=5 |pages=801-4 |year=2007 |pmid=17189243 |doi=10.1093/rheumatology/kel406}}</ref> Three positive studies, all using electro-acupunture, found short term benefits. The methodological quality of the 5 trials was mixed and frequently low. | For ], a systematic review of the best 5 ] available found mixed results.<ref name="pmid17189243">{{cite journal |author=Mayhew E, Ernst E |title=Acupuncture for fibromyalgia--a systematic review of randomized clinical trials |journal=Rheumatology (Oxford, England) |volume=46 |issue=5 |pages=801-4 |year=2007 |pmid=17189243 |doi=10.1093/rheumatology/kel406}}</ref> Three positive studies, all using electro-acupunture, found short term benefits. The methodological quality of the 5 trials was mixed and frequently low. | ||
| For the following conditions, the ] concluded there is insufficient evidence that acupuncture is beneficial, often because of the paucity and poor quality of the research and that further research would be needed to support claims for efficacy: | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| * | |||
| In practice, EBM does not demand that doctors ignore research outside its "top-tier" criteria <ref></ref>. | In practice, EBM does not demand that doctors ignore research outside its "top-tier" criteria <ref></ref>. | ||
Revision as of 05:46, 5 February 2008
| The neutrality of this article is disputed. Relevant discussion may be found on the talk page. Please do not remove this message until conditions to do so are met. (December 2007) (Learn how and when to remove this message) |
| Acupuncture | |
|---|---|
| Medicine: | CAM |
| NCCAM: | Alternative Medical Systems |
| NCCAM: | Energy Medicine |
| Modality: | Professionalized |
| Culture: | East/West |

Acupuncture (from Lat. acus, "needle", and pungere, "prick") or in Standard Mandarin, zhēn biān (a related word zhēn jiǔ refers to acupuncture together with moxibustion) is a technique of inserting and manipulating filiform needles into points on the body with the aim of restoring health and well-being, and particularly treating pain. Acupuncture is thought to have originated in China and is most commonly associated with Traditional Chinese medicine (TCM). Different types of acupuncture (Classical Chinese, Japanese, Tibetan, and Korean acupuncture) are practiced and taught throughout the world.
Scientists are studying the mechanisms and efficacy of acupuncture. The effectiveness of acupuncture remains controversial in the scientific community, and a review by Edzard Ernst and colleagues in 2007 found that the body of evidence was growing, research is active, and that the "emerging clinical evidence seems to imply that acupuncture is effective for some but not all conditions". Researchers using the protocols of evidence-based medicine have found good evidence that acupuncture is moderately effective in preventing nausea. There is conflicting evidence that it can treat chronic low back pain, and moderate evidence of efficacy for neck pain and headache. For most other conditions reviewers have found either a lack of efficacy (e.g., help in quitting smoking) or have concluded that there is insufficient evidence to determine if acupuncture is effective (e.g., treating shoulder pain). While little is known about the mechanisms by which acupuncture may act, a review of neuroimaging research suggests that specific acupuncture points have distinct effects on cerebral activity in specific areas that are not otherwise predictable anatomically.
The WHO, the National Center for Complementary and Alternative Medicine (NCCAM) of the National Institutes of Health (NIH), the American Medical Association (AMA) and various government reports have also studied and commented on the efficacy of acupuncture. There is also general agreement that acupuncture is safe when administered by well-trained practitioners, and that further research is warranted.
Traditional Chinese medicine's acupuncture theory predates the use of the modern scientific method, and has received various criticisms based on modern scientific thinking. There is no generally-accepted anatomical or histological basis for the existence of acupuncture points or meridians. Acupuncturists tend to perceive TCM concepts in functional rather than structural terms, i.e. as being useful in guiding evaluation and care of patients. As the NIH consensus statement noted: "Despite considerable efforts to understand the anatomy and physiology of the "acupuncture points", the definition and characterization of these points remains controversial. Even more elusive is the basis of some of the key traditional Eastern medical concepts such as the circulation of Qi, the meridian system, and the five phases theory, which are difficult to reconcile with contemporary biomedical information but continue to play an important role in the evaluation of patients and the formulation of treatment in acupuncture."
Traditional theory
Traditional Chinese medicine
Main article: Traditional Chinese medicineChinese medicine is based on a pre-scientific paradigm of medicine that developed over several thousand years. Its theory holds the following explanation of acupuncture:
Health is a condition of balance of yin and yang within the body. Particularly important in acupuncture is the free flow of Qi, a difficult-to-translate concept that pervades Chinese philosophy and is commonly translated as "vital energy"). Qi is immaterial and hence yang; its yin, material counterpart is Blood (capitalized to distinguish it from physiological blood, and very roughly equivalent to it). Acupuncture treatment regulates the flow of Qi and Blood, tonifying where there is deficiency, draining where there is excess, and promoting free flow where there is stagnation. An axiom of the medical literature of acupuncture is "no pain, no blockage; no blockage, no pain."
Many patients claim to experience the sensations of stimulus known in Chinese as de qi ("obtaining the Qi" or "arrival of the Qi"). This kind of sensation was historically considered to be evidence of effectively locating the desired point. (There are some electronic devices now available which will make a noise when what they have been programmed to describe as the "correct" acupuncture point is pressed).
TCM treats the human body as a whole that involves several "systems of function" generally named after anatomical organs but not directly associated with them. The Chinese term for these systems is Zang Fu, where zang is translated as "viscera" or solid organs and fu is translated as ""bowels" or hollow organs. In order to distinguish systems of function from physical organs, Zang Fu are capitalized in English, thus Lung, Heart, Kidney, etc. Disease is understood as a loss of balance of Yin, Yang, Qi and Blood (which bears some resemblance to homeostasis). Treatment of disease is attempted by modifying the activity of one or more systems of function through the activity of needles, pressure, heat, etc. on sensitive parts of the body of small volume traditionally called "acupuncture points" in English, or "xue" (穴, cavities) in Chinese. This is referred to in TCM as treating "patterns of disharmony."
Acupuncture points and meridians
See also: Acupuncture points and Channel (Chinese medicine)
Most acupuncture points are found along the "fourteen channels", which are described in TCM as pathways through which Qi and Blood flow. There also exist "extra points" not belonging to any channel. Other tender points (known as "ashi points") may also be needled as they are believed to be where stagnation has gathered.
Treatment of acupuncture points may be performed along several layers of pathways, most commonly the twelve primary channels, or mai, located throughout the body. The first twelve channels correspond to systems of function: Lung, Large Intestine, Stomach, Spleen, Heart, Small Intestine, Bladder, Kidney, Pericardium, San Jiao (an intangible, also known as Triple Burner), Gall Bladder, and Liver. Other pathways include the Eight Extraordinary Pathways (Qi Jing Ba Mai), the Luo Vessels, the Divergents and the Sinew Channels. Ashi (tender) points are generally used for treatment of local pain.
Of the eight extraordinary pathways, only two have acupuncture points of their own: the Ren Mai and Du Mai, which are situated on the midline of the anterior and posterior aspects of the trunk and head respectively. The other six meridians are "activated" by using a master and couple point technique which involves needling the acupuncture points located on the twelve main meridians that correspond to the particular extraordinary pathway.
The twelve primary pathways run vertically, bilaterally, and symmetrically and every channel corresponds to and connects internally with one of the twelve Zang Fu ("organs"). This means that there are six yin and six yang channels. There are three yin and three yang channels on each arm, and three yin and three yang on each leg.
- The three yin channels of the hand (Lung, Pericardium, and Heart) begin on the chest and travel along the inner surface (mostly the anterior portion) of the arm to the hand.
- The three yang channels of the hand (Large intestine, San Jiao, and Small intestine) begin on the hand and travel along the outer surface (mostly the posterior portion) of the arm to the head.
- The three yin channels of the foot (Spleen, Liver, and Kidney) begin on the foot and travel along the inner surface (mostly posterior and medial portion) of the leg to the chest or flank.
- The three yang channels of the foot (Stomach, Gallbladder, and Urinary Bladder) begin on the face, in the region of the eye, and travel down the body and along the outer surface (mostly the anterior and lateral portion) of the leg to the foot.
The movement of Qi through each of the twelve channels comprises an internal and an external pathway. The external pathway is what is normally shown on an acupuncture chart and is relatively superficial. All of the acupuncture points of a channel lie on its external pathway. The internal pathways are the deep course of the channel where it enters the body cavities and related Zang Fu organs. The superficial pathways of the twelve channels describe three complete circuits of the body, chest to hands, hands to head, head to feet, feet to chest, etc.
The distribution of Qi through the pathways is said to be as follows (the based on the demarcations in TCM's Chinese Clock): Lung channel of hand taiyin to Large Intestine channel of hand yangming to Stomach channel of foot yangming to Spleen channel of foot taiyin to Heart channel of hand shaoyin to Small Intestine channel of hand taiyang to Bladder channel of foot taiyang to Kidney channel of foot shaoyin to Pericardium channel of hand jueyin to San Jiao channel of hand shaoyang to Gallbladder channel of foot shaoyang to Liver channel of foot jueyin then back to the Lung channel of hand taiyin. According to the "Chinese clock", each channel occupies two hours, beginning with the Lung, 3AM-5AM, and coming full circle with the Liver 1AM-3AM.
Traditional diagnosis
The acupuncturist decides which points to treat by observing and questioning the patient in order to make a diagnosis according to the tradition which he or she utilizes. In TCM, there are four diagnostic methods: inspection, auscultation and olfaction, inquiring, and palpation (Cheng, 1987, ch. 12).
- Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge.
- Auscultation and olfaction refer, respectively, to listening for particular sounds (such as wheezing) and attending to body odor.
- Inquiring focuses on the "seven inquiries", which are: chills and fever; perspiration; appetite, thirst and taste; defecation and urination; pain; sleep; and menses and leukorrhea.
- Palpation includes feeling the body for tender "ashi" points, and palpation of the left and right radial pulses at two levels of pressure (superficial and deep) and three positions Cun, Guan, Chi(immediately proximal to the wrist crease, and one and two fingers' breadth proximally, usually palpated with the index, middle and ring fingers).
Other forms of acupuncture employ additional diagnosic techniques. In many forms of classical Chinese acupuncture, as well as Japanese acupuncture, palpation of the muscles and the hara (abdomen) are central to diagnosis.
TCM perspective on treatment of disease
Although TCM is based on the treatment of "patterns of disharmony" rather than biomedical diagnoses, practitioners familiar with both systems have commented on relationships between the two. A given TCM pattern of disharmony may be reflected in a certain range of biomedical diagnoses: thus, the pattern called Deficiency of Spleen Qi could manifest as chronic fatigue, diarrhea or uterine prolapse. Likewise, a population of patients with a given biomedical diagnosis may have varying TCM patterns. These observations are encapsulated in the TCM aphorism "One disease, many patterns; one pattern, many diseases". (Kaptchuk, 1982)
Classically, in clinical practice, acupuncture treatment is typically highly-individualized and based on philosophical constructs, and subjective and intuitive impressions" and not on controlled scientific research.
Criticism of TCM theory
TCM theory predates use of the scientific method and has received various criticisms based on scientific reductionist thinking, since there is no physically verifiable anatomical or histological basis for the existence of acupuncture points or meridians.
Felix Mann, founder and past-president of the Medical Acupuncture Society (1959–1980), the first president of the British Medical Acupuncture Society (1980), and the author of the first comprehensive English language acupuncture textbook Acupuncture: The Ancient Chinese Art of Healing' first published in 1962, has stated in his book Reinventing Acupuncture: A New Concept of Ancient Medicine:
- "The traditional acupuncture points are no more real than the black spots a drunkard sees in front of his eyes." (p. 14)
and…
- "The meridians of acupuncture are no more real than the meridians of geography. If someone were to get a spade and tried to dig up the Greenwich meridian, he might end up in a lunatic asylum. Perhaps the same fate should await those doctors who believe in meridians." (p. 31)
Philosopher Robert Todd Carroll deems acupuncture a pseudoscience because it "confuse(s) metaphysical claims with empirical claims". Carroll states that:
- "...no matter how it is done, scientific research can never demonstrate that unblocking chi by acupuncture or any other means is effective against any disease. Chi is defined as being undetectable by the methods of empirical science."
A report for CSICOP on pseudoscience in China written by Wallace Sampson and Barry L. Beyerstein said:
- "A few Chinese scientists we met maintained that although Qi is merely a metaphor, it is still a useful physiological abstraction (e.g., that the related concepts of Yin and Yang parallel modern scientific notions of endocrinologic and metabolic feedback mechanisms). They see this as a useful way to unite Eastern and Western medicine. Their more hard-nosed colleagues quietly dismissed Qi as only a philosophy, bearing no tangible relationship to modern physiology and medicine."
George A. Ulett, MD, PhD, Clinical Professor of Psychiatry, University of Missouri School of Medicine states: "Devoid of metaphysical thinking, acupuncture becomes a rather simple technique that can be useful as a nondrug method of pain control." He believes that the traditional Chinese variety is primarily a placebo treatment, but electrical stimulation of about 80 acupuncture points has been proven useful for pain control.
Ted J. Kaptchuk, author of The Web That Has No Weaver, refers to acupuncture as "prescientific." Regarding TCM theory, Kaptchuk states:
- "These ideas are cultural and speculative constructs that provide orientation and direction for the practical patient situation. There are few secrets of Oriental wisdom buried here. When presented outside the context of Chinese civilization, or of practical diagnosis and therapeutics, these ideas are fragmented and without great significance. The "truth" of these ideas lies in the way the physician can use them to treat real people with real complaints." (1983, pp. 34-35)
According to the NIH consensus statement on acupuncture:
- "Despite considerable efforts to understand the anatomy and physiology of the "acupuncture points", the definition and characterization of these points remains controversial. Even more elusive is the basis of some of the key traditional Eastern medical concepts such as the circulation of Qi, the meridian system, and the five phases theory, which are difficult to reconcile with contemporary biomedical information but continue to play an important role in the evaluation of patients and the formulation of treatment in acupuncture."
History
In China, the practice of acupuncture can perhaps be traced as far back as the stone age, with the Bian shi, or sharpened stones. Stone acupuncture needles dating back to 3000 B.C. have been found by archeologists in Inner Mongolia. Clearer evidence exists from the 1 millennium BCE, and archeological evidence has been identified with the period of the Han dynasty (202 BC–220 AD). Forms of it are also described in the literature of traditional Korean medicine where it is called chimsul. It is also important in Kampo, the traditional medicine system of Japan.
Recent examinations of Ötzi, a 5,000-year-old mummy found in the Alps, have identified over 50 tattoos on his body, some of which are located on acupuncture points that would today be used to treat ailments Ötzi suffered from. Some scientists believe that this is evidence that practices similar to acupuncture were practised elsewhere in Eurasia during the early bronze age. According to an article published in The Lancet by Dorfer et al., "We hypothesised that there might have been a medical system similar to acupuncture (Chinese Zhenjiu: needling and burning) that was practised in Central Europe 5,200 years ago... A treatment modality similar to acupuncture thus appears to have been in use long before its previously known period of use in the medical tradition of ancient China. This raises the possibility of acupuncture having originated in the Eurasian continent at least 2000 years earlier than previously recognised.", .
Acupuncture's origins in China are uncertain. The earliest Chinese medical text that first describes acupuncture is the Yellow Emperor’s Classic of Internal Medicine (History of Acupuncture) Huangdi Neijing, which was compiled around 305–204 B.C. However, the Chinese medical texts (Ma-wang-tui graves, 68 BC) do not mention acupuncture. Some hieroglyphics have been found dating back to 1000 B.C. that may indicate an early use of acupuncture. Bian stones, sharp pointed rocks used to treat diseases in ancient times, have also been discovered in ruins; some scholars believe that the bloodletting for which these stones were likely used presages certain acupuncture techniques.
According to a tradition that is widely quoted in various versions, acupuncture started in China when some soldiers who were wounded by arrows in battle experienced a relief of pain in other parts of the body, and consequently people started experimenting with arrows (and later needles) as therapy.
R.C. Crozier in the book Traditional medicine in modern China (Harvard University Press, Cambridge, 1968) says the early Chinese Communist Party expressed considerable antipathy towards classical forms of Chinese medicine, ridiculing it as superstitious, irrational and backward, and claiming that it conflicted with the Party’s dedication to science as the way of progress. Acupuncture was included in this criticism. Reversing this position, Communist Party Chairman Mao later said that "Chinese medicine and pharmacology are a great treasure house and efforts should be made to explore them and raise them to a higher level."
Representatives were sent out across China to collect information about the theories and practices of Chinese medicine. Traditional Chinese Medicine is the formalized system of Chinese medicine that was created out of this effort. TCM combines the use of acupuncture, Chinese herbal medicine, tui na, and other modalities. After the Cultural Revolution, TCM instruction was incorporated into university medical curricula under the "Three Roads" policy, wherein TCM, biomedicine, and a synthesis of the two would all be encouraged and permitted to develop. After this time, forms of classical Chinese medicine other than TCM were outlawed, and some practitioners left China.
The first forms of acupuncture to reach the United States were brought by non-TCM practitioners -such as Chinese rail road workers- many employing styles that had been handed down in family lineages, or from master to apprentice (collectively known as "Classical Chinese Acupuncture").
In Vietnam, Dr. Van Nghi and colleagues used the classical Chinese medical texts and applied them in clinical conditions without reference to political screening. They rewrote the modern version: Trung E Hoc. Van Nghi was made the first President of the First World Congress of Chinese Medicine at Bejing in 1988 in recognition of his work.
In the 1970s, acupuncture became vogue in America after American visitors to China brought back firsthand reports of patients undergoing major surgery using acupuncture as their sole form of anesthesia. Since then, tens of thousands of treatments are now performed in this country each year for many types of conditions such as back pain, headaches, infertility, stress, and many other illnesses.
Clinical practice
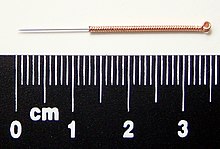
Most modern acupuncturists use disposable stainless steel needles of fine diameter (0.007" to 0.020", 0.18 mm to 0.51 mm), sterilized with ethylene oxide or by autoclave. These needles are far smaller in diameter (and therefore less painful) than the needles used to give shots, since they do not have to be hollow for purposes of injection. The upper third of these needles is wound with a thicker wire (typically bronze), or covered in plastic, to stiffen the needle and provide a handle for the acupuncturist to grasp while inserting. The size and type of needle used, and the depth of insertion, depend on the acupuncture style being practised.
Warming an acupuncture point, typically by moxibustion (the burning of a combination of herbs, primarily mugwort), is a different treatment than acupuncture itself and is often, but not exclusively, used as a supplemental treatment. The Chinese term zhēn jǐu (針灸), commonly used to refer to acupuncture, comes from zhen meaning "needle", and jiu meaning "moxibustion". Moxibustion is still used in the 21 century to varying degrees among the schools of oriental medicine. For example, one well known technique is to insert the needle at the desired acupuncture point, attach dried moxa to the external end of an acupuncture needle, and then ignite it. The moxa will then smolder for several minutes (depending on the amount adhered to the needle) and conduct heat through the needle to the tissue surrounding the needle in the patient's body. Another common technique is to hold a large glowing stick of moxa over the needles. Moxa is also sometimes burned at the skin surface, usually by applying an ointment to the skin to protect from burns, though burning of the skin is general practice in China.
An example of acupuncture treatment
In western medicine, vascular headaches (the kind that are accompanied by throbbing veins in the temples) are typically treated with analgesics such as aspirin and/or by the use of agents such as niacin that dilate the affected blood vessels in the scalp, but in acupuncture a common treatment for such headaches is to stimulate the sensitive points that are located roughly in the center of the webs between the thumbs and the palms of the patient, the hé gǔ points. These points are described by acupuncture theory as "targeting the face and head" and are considered to be the most important point when treating disorders affecting the face and head. The patient reclines, and the points on each hand are first sterilized with alcohol, and then thin, disposable needles are inserted to a depth of approximately 3-5 mm until a characteristic "twinge" is felt by the patient, often accompanied by a slight twitching of the area between the thumb and hand. Most patients report a pleasurable "tingling" sensation and feeling of relaxation while the needles are in place. The needles are retained for 15-20 minutes while the patient rests, and then are removed.
In the clinical practice of acupuncturists, patients frequently report one or more of certain kinds of sensation that are associated with this treatment, sensations that are stronger than those that would be felt by a patient not suffering from a vascular headache:
- Extreme sensitivity to pain at the points in the webs of the thumbs.
- In bad headaches, a feeling of nausea that persists for roughly the same period as the stimulation being administered to the webs of the thumbs.
- Simultaneous relief of the headache. (See Zhen Jiu Xue, p. 177f et passim.)
Indications according to acupuncturists in the West
According to the American Academy of Medical Acupuncture (2004), acupuncture may be considered as a complementary therapy for the conditions in the list below. The conditions labeled with * are also included in the World Health Organization list of acupuncture indications.. These cases, however, are based on clinical experience, and not necessarily on controlled clinical research: furthermore, the inclusion of specific diseases are not meant to indicate the extent of acupuncture's efficacy in treating them.
- Abdominal distention/flatulence*
- Acute and chronic pain control*
- Allergic sinusitis *
- Anesthesia for high-risk patients or patients with previous adverse responses to anesthetics
- Anorexia
- Anxiety, fright, panic*
- Arthritis/arthrosis *
- Atypical chest pain (negative workup)
- Bursitis, tendinitis, carpal tunnel syndrome*
- Certain functional gastrointestinal disorders (nausea and vomiting, esophageal spasm, hyperacidity, irritable bowel) *
- Cervical and lumbar spine syndromes*
- Constipation, diarrhea *
- Cough with contraindications for narcotics
- Drug detoxification *
- Dysmenorrhea, pelvic pain *
- Frozen shoulder *
- Headache (migraine and tension-type), vertigo (Meniere disease), tinnitus *
- Idiopathic palpitations, sinus tachycardia
- In fractures, assisting in pain control, edema, and enhancing healing process
- Muscle spasms, tremors, tics, contractures*
- Neuralgias (trigeminal, herpes zoster, postherpetic pain, other)
- Paresthesias *
- Persistent hiccups*
- Phantom pain
- Plantar fasciitis*
- Post-traumatic and post-operative ileus *
- Premenstrual syndrome
- Selected dermatoses (urticaria, pruritus, eczema, psoriasis)
- Sequelae of stroke syndrome (aphasia, hemiplegia) *
- Seventh nerve palsy
- Severe hyperthermia
- Sleep disorders
- Sprains and contusions
- Temporo-mandibular joint derangement, bruxism *
- Urinary incontinence, retention (neurogenic, spastic, adverse drug effect) *
Additionally, other sources advocate the use of acupuncture for the following conditions:
- Infertility, regarding in vitro fertilization, see Expansions of in vitro fertilization - acupuncture
Scientific theories and mechanisms of action
Main article: Scientific theories regarding acupunctureMany hypotheses have been proposed to address the physiological mechanisms of action of acupuncture. To date, more than 10,000 scientific research studies have been published on acupuncture as cataloged by the National Library of Medicine database.
Neurohormonal theory

Pain transmission can also be modulated at many other levels in the brain along the pain pathways, including the periaqueductal gray, thalamus, and the feedback pathways from the cerebral cortex back to the thalamus. Pain blockade at these brain locations is often mediated by neurohormones, especially those that bind to the opioid receptors (pain-blockade site).
Some studies suggest that the Analgesic (pain-killing) action of acupuncture is associated with the release of natural endorphins in the brain. This effect can be inferred by blocking the action of endorphins (or morphine) using a drug called naloxone. When naloxone is administered to the patient, the analgesic effects of morphine can be reversed, causing the patient to feel pain again. When naloxone is administered to an acupunctured patient, the analgesic effect of acupuncture can also be reversed, causing the patient to report an increased level of pain. It should be noted, however, that studies using similar methodological procedures, including the administration of naloxone, have suggested a role of endogenous opioids in the placebo response, demonstrating that this response is not unique to acupuncture
Such analgesic effect can also be shown to last more than an hour after acupuncture stimulation by recording the neural activity directly in the thalamus of the monkey's brain. Furthermore, there is a large overlap between the nervous system and acupuncture trigger points (points of maximum tenderness) in myofascial pain syndrome.
Evidence suggests that the sites of action of analgesia associated include the thalamus using fMRI (functional magnetic resonance imaging) and PET (positron emission tomography) brain imaging techniques, and via the feedback pathway from the cerebral cortex using electrophysiological recording of the nerve impulses of neurons directly in the cortex, which shows inhibitory action when acupuncture stimulus was applied. Similar effects have been observed in association with the placebo response. One study using fMRI found that placebo analgesia was associated with decreased activity in the thalamus, insula and anterior cingulate cortex .
Recently acupuncture has been shown to increase the nitric oxide levels in treated regions and resulting in increased local blood circulation, an outcome found in other studies. Effects on local inflammation and ischemia have also been previously reported.
Histological studies
In the 1960's, Bonghan Kim (medical scientist, North Korea) proposed that meridians and acupuncture points exist in the form of distinctive anatomical structures in his Bonghan Theory.
In the 2000's, some medical scientists started to take Bonghan Kim's theory seriously. Quite some papers were published by medical scientists in South Korea to follow up on Bonghan Kim's theory.
Issues in study design
One of the major challenges in acupuncture research is in the design of an appropriate placebo control group. In trials of new drugs, double blinding is the accepted standard, but since acupuncture is a procedure rather than a pill, it is difficult to design studies in which both the acupuncturist and patient are blinded as to the treatment being given. The same problem arises in double-blinding procedures used in biomedicine, including virtually all surgical procedures, dentistry, physical therapy, etc.
Blinding of the practitioner in acupuncture remains challenging. One proposed solution to blinding patients has been the development of "sham acupuncture", i.e., needling performed superficially a/o at non-acupuncture sites. Controversy remains over whether, and under what conditions, sham acupuncture may function as as true placebo, particularly in studies in pain in which insertion of needles anywhere near painful regions may elicit a beneficial response.
A study by Ted Kaptchuk et. al. showed that sham acupuncture exerted a stronger effect on pain than an inert pill did, and concluded: "Placebo effects seem to be malleable and depend on the behaviours embedded in medical rituals."
Scientific research into efficacy
Evidence-based medicine
There is scientific agreement that an evidence-based medicine (EBM) framework should be used to assess health outcomes and that systematic reviews with strict protocols are essential. Organisations such as the Cochrane Collaboration and Bandolier publish such reviews.
The development of the evidence base for acupuncture was summarized in a review by researcher Edzard Ernst and colleagues in 2007. They compared systematic reviews conducted (with similar methodology) in 2000 and 2005:
- The effectiveness of acupuncture remains a controversial issue. ... The results indicate that the evidence base has increased for 13 of the 26 conditions included in this comparison. For 7 indications it has become more positive (i.e. favoring acupuncture) and for 6 it had changed in the opposite direction. It is concluded, that acupuncture research is active. The emerging clinical evidence seems to imply that acupuncture is effective for some but not all conditions.
For low back pain, a Cochrane review (2005) stated:
- Thirty-five RCTs covering 2861 patients were included in this systematic review. There is insufficient evidence to make any recommendations about acupuncture or dry-needling for acute low-back pain. For chronic low-back pain, results show that acupuncture is more effective for pain relief than no treatment or sham treatment, in measurements taken up to three months. The results also show that for chronic low-back pain, acupuncture is more effective for improving function than no treatment, in the short-term. Acupuncture is not more effective than other conventional and "alternative" treatments. When acupuncture is added to other conventional therapies, it relieves pain and improves function better than the conventional therapies alone. However, effects are only small. Dry-needling appears to be a useful adjunct to other therapies for chronic low-back pain.
A review by Manheimer et al. in Annals of Internal Medicine (2005) reached conclusions similar to Cochrane's review on low back pain. A review for the American Pain Society/American College of Physicians found fair evidence that acupuncture is effective for chronic low back pain.
For nausea and vomiting: The Cochrane review (Lee and Done, 2006) on the use of the P6 acupoint for the reduction of post-operative nausea and vomiting concluded that the use of P6 acupoint stimulation can reduce the risk of postoperative nausea and vomiting with minimal side effects, albeit with efficacy less than or equal to prophylactic (i.e., preventative) treatment with antiemetic drugs. Cochrane also stated: "Electroacupuncture is effective for first day vomiting after chemotherapy, but trials considering modern antivomiting drugs are needed."
A 2007 Cochrane Review for the use of acupuncture for neck pain stated:
- There is moderate evidence that acupuncture relieves pain better than some sham treatments, measured at the end of the treatment. There is moderate evidence that those who received acupuncture reported less pain at short term follow-up than those on a waiting list. There is also moderate evidence that acupuncture is more effective than inactive treatments for relieving pain post-treatment and this is maintained at short-term follow-up.
For headache, Cochrane concluded (2006) that "(o)verall, the existing evidence supports the value of acupuncture for the treatment of idiopathic headaches. However, the quality and amount of evidence are not fully convincing. There is an urgent need for well-planned, large-scale studies to assess the effectiveness and cost-effectiveness of acupuncture under real-life conditions." .
For osteoarthritis, reviews since 2006 show acupuncture to be more effective than no treatment at all, but approximately as effective as sham acupuncture (wherein needles are inserted in points that, according to acupuncture theory, should not be effective).
For fibromyalgia, a systematic review of the best 5 randomized controlled trials available found mixed results. Three positive studies, all using electro-acupunture, found short term benefits. The methodological quality of the 5 trials was mixed and frequently low.
For the following conditions, the Cochrane Collaboration concluded there is insufficient evidence that acupuncture is beneficial, often because of the paucity and poor quality of the research and that further research would be needed to support claims for efficacy:
- Giving up smoking
- Chronic asthma
- Bell's palsy
- Shoulder pain
- Lateral elbow pain
- Acute stroke
- Rheumatoid arthritis
- Depression
- Induction of labour
In practice, EBM does not demand that doctors ignore research outside its "top-tier" criteria .
Evidence from neuroimaging studies
Acupuncture appears to have effects on cortical activity, as demonstrated by MRI (magnetic resonance imaging) and PET (positron emission tomography). Researchers from the University of Southampton, UK and Purpan Hospital of Toulouse, France, summarize the literature:
- Investigating Acupuncture Using Brain Imaging Techniques: The Current State of Play: George T. Lewith, Peter J. White and Jeremie Pariente. "We have systematically researched and reviewed the literature looking at the effect of acupuncture on brain activation as measured by functional magnetic resonance imaging and positron emission tomography. These studies show that specific and largely predictable areas of brain activation and deactivation occur when considering the traditional Chinese functions attributable to certain specific acupuncture points. For example, points associated with hearing and vision stimulates the visual and auditory cerebral areas respectively. Pain, however, is a complex matrix that is intimately intertwined with expectation. Acupuncture clearly affects this matrix in both specific and non-specific manner that is consistent with its specific clinical effects, as well as the effects of expectation on pain relief. ... It is quite possible that specific acupuncture points for non-painful conditions, such as PC6 in the treatment of nausea, may activate or inhibit very specific neuronal substrates. This may support ... the assumptions inherent within traditional Chinese medicine. The effects of acupuncture in pain and possibly also in addiction may be far less point-specific as has been previously suggested from the available clinical evidence."
NIH consensus statement
According to the National Institutes of Health:
- Preclinical studies have documented acupuncture's effects, but they have not been able to fully explain how acupuncture works within the framework of the Western system of medicine that is commonly practiced in the United States.
In 1997, the National Institutes of Health (NIH) issued a consensus statement on acupuncture that concluded that
- there is sufficient evidence of acupuncture's value to expand its use into conventional medicine and to encourage further studies of its physiology and clinical value.
The statement was not a policy statement of the NIH but rather the assessment of a panel convened by the NIH.
The NIH consensus statement said that
- the data in support of acupuncture are as strong as those for many accepted Western medical therapies
and added that
- there is clear evidence that needle acupuncture is efficacious for adult postoperative and chemotherapy nausea and vomiting and probably for the nausea of pregnancy... There is reasonable evidence of efficacy for postoperative dental pain... reasonable studies (although sometimes only single studies) showing relief of pain with acupuncture on diverse pain conditions such as menstrual cramps, tennis elbow, and fibromyalgia...
The NIH consensus statement summarized and made a prediction:
- Acupuncture as a therapeutic intervention is widely practiced in the United States. While there have been many studies of its potential usefulness, many of these studies provide equivocal results because of design, sample size, and other factors. The issue is further complicated by inherent difficulties in the use of appropriate controls, such as placebos and sham acupuncture groups. However, promising results have emerged, for example, showing efficacy of acupuncture in adult postoperative and chemotherapy nausea and vomiting and in postoperative dental pain. There are other situations such as addiction, stroke rehabilitation, headache, menstrual cramps, tennis elbow, fibromyalgia, myofascial pain, osteoarthritis, low back pain, carpal tunnel syndrome, and asthma, in which acupuncture may be useful as an adjunct treatment or an acceptable alternative or be included in a comprehensive management program. Further research is likely to uncover additional areas where acupuncture interventions will be useful.
The NIH's National Center For Complementary And Alternative Medicine continues to abide by the recommendations of the NIH Consensus Statement .
American Medical Association statement
In 1997, the following statement was adopted as policy of the American Medical Association (AMA), an association of medical doctors and medical students, after a report on a number of alternative therapies including acupuncture:
"There is little evidence to confirm the safety or efficacy of most alternative therapies. Much of the information currently known about these therapies makes it clear that many have not been shown to be efficacious. Well-designed, stringently controlled research should be done to evaluate the efficacy of alternative therapies."
German study
A German study published in the September 2007 issue of the Archives of Internal Medicine found that nearly half of patients treated with acupuncture or a sham treatment felt relief from chronic low back pain over a period of months compared to just nearly a quarter of those receiving a variety of more conventional treatments (drugs, heat, massage, etc.) The greater benefit of the real and sham treatments were not significantly different.
Nonacupuncture points
A controlled study of 300 migraine patients found that both sham and real acupuncture resulted in improvements compared with patients on a waiting list, with no significant difference in benefit between the sham and active treatment groups. The sham treatment involved actual needles piercing the skin, but at nonacupuncture points.
Some researchers have questioned the use of sham acupuncture as a control in this study and others, arguing that sham acupuncture may be too similar to real acupuncture to be a valid control, thereby skewing results toward showing a relative lack of efficacy.
Safety and risks
Because acupuncture needles penetrate the skin, many forms of acupuncture are invasive procedures, and therefore not without risk. Injuries are rare among patients treated by trained practitioners.
Certain forms of acupuncture such as the Japanese Tōyōhari and Shōnishin often use non-invasive techniques, in which specially-designed needles are rubbed or pressed against the skin. These methods are common in Japanese pediatric use.
Common, minor adverse events
A survey by Ernst et al. of over 400 patients receiving over 3500 acupuncture treatments found that the most common adverse effects from acupuncture were:
- Minor bleeding after removal of the needles, seen in roughly 3% of patients. (Holding a cotton ball for about one minute over the site of puncture is usually sufficient to stop the bleeding.)
- Hematoma, seen in about 2% of patients, which manifests as bruises. These usually go away after a few days.
- Dizziness, seen in about 1% of patients. Some patients have a conscious or unconscious fear of needles which can produce dizziness and other symptoms of anxiety. Patients are usually treated lying down in order to reduce likelihood of fainting.
The survey concluded: "Acupuncture has adverse effects, like any therapeutic approach. If it is used according to established safety rules and carefully at appropriate anatomic regions, it is a safe treatment method."
Other injury
Other risks of injury from the insertion of acupuncture needles include:
- Nerve injury, resulting from the accidental puncture of any nerve.
- Brain damage or stroke, which is possible with very deep needling at the base of the skull.
- Pneumothorax from deep needling into the lung.
- Kidney damage from deep needling in the low back.
- Haemopericardium, or puncture of the protective membrane surrounding the heart, which may occur with needling over a sternal foramen (a hole in the breastbone that occurs as the result of a congenital defect.)
- Risk of terminating pregnancy with the use of certain acupuncture points that have been shown to stimulate the production of adrenocorticotropic hormone (ACTH) and oxytocin.
These risks are slight and can all be avoided through proper training of acupuncturists. For correct perspective, their risk should be compared to the level of side effects of common drugs and biomedical treatment - see below. Graduates of medical schools and (in the US) accredited acupuncture schools receive thorough instruction in proper technique so as to avoid these events. (Cf. Cheng, 1987)
Risks from omitting orthodox medical care
Some doctors believe that receiving any form of alternative medical care without also receiving orthodox western medical care is inherently risky, since undiagnosed disease may go untreated and could worsen. For this reason many acupuncturists and doctors prefer to consider acupuncture a complementary therapy rather than an alternative therapy.
Critics also express concern that unethical or naive practitioners may induce patients to exhaust financial resources by pursuing ineffective treatment. However, many recent public health departments in modern countries have acknowledged the benefits of acupuncture by instituting regulations, ultimately raising the level of medicine practiced in these jurisdictions.
Safety compared to other treatments
Commenting on the relative safety of acupuncture compared to other treatments, the NIH consensus panel stated that "(a)dverse side effects of acupuncture are extremely low and often lower than conventional treatments." They also stated:
- "the incidence of adverse effects is substantially lower than that of many drugs or other accepted medical procedures used for the same condition. For example, musculoskeletal conditions, such as fibromyalgia, myofascial pain, and tennis elbow... are conditions for which acupuncture may be beneficial. These painful conditions are often treated with, among other things, anti-inflammatory medications (aspirin, ibuprofen, etc.) or with steroid injections. Both medical interventions have a potential for deleterious side effects but are still widely used and are considered acceptable treatments."
In a Japanese survey of 55,291 acupuncture treatments given over five years by 73 acupuncturists, 99.8% of them were performed with no significant minor adverse effects and zero major adverse incidents (Hitoshi Yamashita, Bac, Hiroshi Tsukayama, BA, Yasuo Tanno, MD, PhD. Kazushi Nishijo, PhD, JAMA). Two combined studies in the UK of 66,229 acupuncture treatments yielded only 134 minor adverse events. (British Medical Journal 2001 Sep 1). The total of 121,520 treatments with acupuncture therapy were given with no major adverse incidents (for comparison, a single such event would have indicated a 0.0008% incidence).
Legal and political status
Acupuncturists may also practice herbal medicine or tui na, or may be medical acupuncturists, who are trained in allopathic medicine but also practice acupuncture in a simplified form. License is regulated by the state or province in many countries, and often requires passage of a board exam.
United States
In the US, acupuncture is practiced by a variety of healthcare providers. Those who specialize in Acupuncture and Oriental Medicine are usually referred to as "licensed acupuncturists", or L.Ac.'s. Other healthcare providers such as physicians, dentists and chiropractors sometimes also practice acupuncture, though they may often receive less training than L.Ac.'s. L.Ac.'s generally receive from 2500 to 4000 hours of training in Chinese medical theory, acupuncture, and basic biosciences. Some also receive training in Chinese herbology and/or bodywork. The amount of training required for healthcare providers who are not L.Ac.'s varies from none to a few hundred hours, and in Hawaii the practice of acupuncture requires full training as a licensed acupuncturist. The National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) tests practitioners to ensure they are knowledgeable about Chinese medicine and appropriate sterile technique. Many states require this test for licensing, but each state has its own laws and requirements. Some states use titles besides L.Ac. for licensed practitioners specializing in acupuncture: "D.O.M." (Doctor of Oriental Medicine) in New Mexico, "D.Ac." (Doctor of Acupuncture) in Rhode Island, and "A.P." (Acupuncture Physician) in Florida. Some states, such as California and Florida, legally treat acupuncturists as primary care providers. Most states allow acupuncturists to practice without a referral from another medical practitioner.
The abbreviation "Dipl. Ac." stands for "Diplomate of Acupuncture" and signifies that the holder is board-certified by the NCCAOM. Professional degrees are usually at the level of a Master's degree and include "M.Ac." (Master's in Acupuncture), "M.S.Ac." (Master's of Science in Acupuncture), "M.S.O.M" (Master's of Science in Oriental Medicine), and "M.A.O.M." (Master's of Acupuncture and Oriental Medicine). As of 2007, the Accreditation Commission for Acupuncture and Oriental Medicine (ACAOM) is beginning the process of accrediting the "Doctor of Acupuncture and Oriental Medicine" (DAOM) degree, and this new degree will represent the terminal degree in the field. The Oregon College of Oriental Medicine and Bastyr University were the first two institutions in the United States to offer the DAOM. The titles "O.M.D." (Doctor of Oriental Medicine) and "C.M.D." (Doctor of Chinese Medicine) are sometimes used by graduates of Chinese medical schools who have received the Bachelor of Medicine and Surgery degree. "O.M.D." may also signify a degree, granted by certain American schools, indicating a year or two of study beyond the Master's level. The O.M.D. and C.M.D. are not recognized by the ACAOM.
Acupuncturists are required to obtain continuing education credit to retain their licenses. There are three bodies that approve continuing education courses for re-licensure: the California Acupuncture Board, the Florida Board of Acupuncture, and the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM). The NCCAOM awards PDA points towards re-licensure for approved courses and requires Diplomates (licensed acupuncturists with NCCAOM certification) to obtain 60 PDA points every four years to re-certify. The California Acupuncture Board governs the re-licensure of all California licensed acupuncturists and requires fifty continuing education units (CEU’s) every two years. The Florida Board of Acupuncture governs all licensed acupuncturists in Florida and requires acupuncturists to complete 30 continuing education credit hours (CE’s) every two years. The NCCAOM and Florida Acupuncture Board calculate continuing education credit hours based on the calculation that sixty minutes of course time equals one continuing education point or unit. The California Acupuncture Board calculates that one continuing education unit is awarded for fifty minutes of course time and limits distance education to fifty percent of total CEU’s.
Acupuncture is becoming accepted by the general public and by doctors. Over fifteen million Americans tried acupuncture in 1994. A poll of American doctors in 2005 showed that 59% believe acupuncture was at least somewhat effective, with the percentage increasing to 75% if acupuncture is considered as a complement to conventional treatment.
In 1996, the Food and Drug Administration changed the status of acupuncture needles from Class III to Class II medical devices, meaning that needles are regarded as safe and effective when used appropriately by licensed practitioners .
Canada
In the province of British Columbia the TCM practitioners and Acupuncturists Bylaws were approved by the provincial government on April 12, 2001. The governing body, College of Traditional Chinese Medicine Practitioners and Acupuncturists of British Columbia provides professional licensing. Acupuncturists began lobbying the B.C. government in the 1970s for regulation of the profession which was achieved in 2003.
In Ontario, the practice of acupuncture is now regulated by the Traditional Chinese Medicine Act, 2006, S.o. 2006, chapter 27. The government is in the process of establishing a College whose mandate will be to oversee the implementation of policies and regulations relating to the profession. Practitioners of Traditional Chinese medicine will be permitted to use the title 'Doctor of Traditional Chinese medicine'. In addition, they will be permitted to communicate a diagnosis to patients based on Traditional Chinese medicine techniques for diagnosis. Other regulated Health Care Professionals, such as naturopaths, physicians, physiotherapists, chiropractors, dentists, or massage therapists can perform acupuncture treatments when they fulfill educational requirements set up by their regulatory colleges. It is noteworthy, however, that the school (philosophy and approach) and style of acupuncture differs depending on the training of the practitioner.
United Kingdom
In the United Kingdom, British Acupuncture Council (BAcC) members observe the Code of Safe Practice with standards of hygiene and sterilisation of equipment. Members use single-use pre-sterilised disposable needles. Similar standards apply in most jurisdictions in the United States and Australia.
The British Acupuncture Council
Acupuncture is also practiced by a number of registered medical practitioners, many of whom belong to the British Medical Acupunture Society (BMAS), which also publishes a quarterly journal "Acupuncture in Medicine". Medical practitioners of acupuncture in the UK vary in the degree to which they take account of traditional concepts like meridians, some thinking them to be very useful whilst others tend to concentrate on palpable "trigger points". Other acupuncture groups are the British Academy of Western Medical Acupuncture (BAWMA) - nurses trained in acupuncture, the Acupuncture Association of Chartered Physiotherapists (AACP), and qualified ear acupuncturists trained either in restricted practice NADA and SMART or full ear acupuncture EAR and SAA.
The British Acupuncture Council claims to act as the United Kingdom's main regulatory body for acupuncture, as noted on their website home page and on most of their literature, however there is no statutorily regulated body in the United Kingdom for acupuncture at present. although the UK Government do have plans to introduce a regulated body in 2010, In the interests of public safety, some health professionals find it questionable whether the British Acupuncture Council should be making such a statement.
Australia
In Australia, the legalities of practicing acupuncture also vary by state. In 2000, an independent government agency was established to oversee the practice of Chinese Herbal Medicine and Acupuncture in the state of Victoria. The Chinese Medicine Registration Board of Victoria aims to protect the public, ensuring that only appropriately experienced or qualified practitioners are registered to practice Chinese Medicine. The legislation put in place stipulates that only practitioners who are state registered may use the following titles: Acupuncture, Chinese Medicine, Chinese Herbal Medicine, Registered Acupuncturist, Registered Chinese Medicine Practitioner, and Registered Chinese Herbal Medicine Practitioner.
The Parliamentary Committee on the Health Care Complaints Commission in the Australian state of New South Wales commissioned a report investigating Traditional Chinese medicine practice. They recommended the introduction of a government appointed registration board that would regulate the profession by restricting use of the titles "acupuncturist", "Chinese herbal medicine practitioner" and "Chinese medicine practitioner". The aim of registration is to protect the public from the risks of acupuncture by ensuring a high baseline level of competency and education of registered acupuncturists, enforcing guidelines regarding continuing professional education and investigating complaints of practitioner conduct. The registration board will hold more power than local councils in respect to enforcing compliance with legal requirements and investigating and punishing misconduct. Victoria is the only state of Australia with an operational registration board. Currently acupuncturists in NSW are bound by the guidelines in the Public Health (Skin Penetration) Regulation 2000 which is enforced at local council level. Other states of Australia have their own skin penetration acts. The act describes explicitly that single-use disposable needles should be used wherever possible, and that a needle labelled as "single-use" should be disposed of in a sharps container and never reused. Any other type of needle that penetrates the skin should be appropriately sterilised (by autoclave) before reuse.
Many other countries do not license acupuncturists or require them be trained.
See also
- Acupoint therapy
- Acupressure
- Acupuncture detoxification
- Auriculotherapy
- Chin na
- Chinese martial arts
- Dragon Rises College of Oriental Medicine
- Electroacupuncture
- Medical acupuncture
- Pressure Points
- Qi
- Qigong
- Seitai
- Susuk
- T'ai Chi Ch'uan
- Taoism
- Traditional Chinese medicine
- Trigger point
Bibliography
- Vincent CA, Richardson PH (1986). "The evaluation of therapeutic acupuncture: concepts and methods". Pain. 24 (1): 1–13. PMID 3513094.
- Richardson PH, Vincent CA (1986). "Acupuncture for the treatment of pain". Pain. 24: 1540.
- Ter Riet G; et al. (1989). "The effectiveness of acupuncture". Huisarts Wet. 32: 170–175, 176–181, 308–312.
{{cite journal}}: Explicit use of et al. in:|author=(help) - Brinkhaus B, Hummelsberger J, Kohnen R; et al. (2004). "Acupuncture and Chinese herbal medicine in the treatment of patients with seasonal allergic rhinitis: a randomized-controlled clinical trial". Allergy. 59 (9): 953–60. doi:10.1111/j.1398-9995.2004.00540.x. PMID 15291903.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - G. Maciocia. The Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists. Second Edition. Churchill Livingstone. 1989
- P. Deadman, K. Baker, M. Al-Khafaji. A Manual of Acupuncture. Eastland Press
- Witt C, Brinkhaus B, Jena S; et al. (2005). "Acupuncture in patients with osteoarthritis of the knee: a randomised trial". Lancet. 366 (9480): 136–43. doi:10.1016/S0140-6736(05)66871-7. PMID 16005336.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Edwards, J. Acupuncture and Heart Health. Access, February 2002
- Wolfe HL (August/September 2005). "Chronic Fatigue Syndrome, Acupuncture and its related modalities" (Reprint at findarticles.com). Townsend Letter for Doctors and Patients.
{{cite web}}: Check date values in:|date=(help) - Abuaisha BB, Costanzi JB, Boulton AJ (1998). "Acupuncture for the treatment of chronic painful peripheral diabetic neuropathy: a long-term study". Diabetes Res. Clin. Pract. 39 (2): 115–21. PMID 9597381.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Altshul, Sara. "Incontinence: Finally, Relief That Works." Prevention December 2005: 33. Academic Search Premier. EBSCO. 30 January 2006
- Deluze C, Bosia L, Zirbs A, Chantraine A, Vischer TL (1992). "Electroacupuncture in fibromyalgia: results of a controlled trial". BMJ. 305 (6864): 1249–52. PMID 1477566.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Cademartori, Lorraine. "Facing the Point." Forbes October 2005: 85. Academic Search
- Ouyang H, Chen JD (2004). "Review article: therapeutic roles of acupuncture in functional gastrointestinal disorders". Aliment. Pharmacol. Ther. 20 (8): 831–41. doi:10.1111/j.1365-2036.2004.02196.x. PMID 15479354.
- Teng, Liang-yüeh; Chʻeng, Hsin-nung (1987). Chinese acupuncture and moxibustion. Beijing: Foreign Language Press. ISBN 7-119-00378-X.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Helms JM (1987). "Acupuncture for the management of primary dysmenorrhea". Obstetrics and gynecology. 69 (1): 51–6. PMID 3540764.
- Jin, Guanyuan, Xiang, Jia-Jia and Jin, Lei: Clinical Reflexology of Acupuncture and Moxibustion (Chinese). Beijing Science and Technology Press, Beijing, 2004. ISBN 7-5304-2862-4
- Jin, Guan-Yuan, Jin, Jia-Jia X. and Jin, Louis L.: Contemporary Medical Acupuncture - A Systems Approach (English). Springer, USA & Higher Education Press, PRC, 2006. ISBN 7-04-019257-8
- Kaptchuk, Ted J. (1983). The web that has no weaver: understanding Chinese medicine. New York, N.Y: Congdon & Weed. ISBN 0-86553-109-9.
- Premier. EBSCO. 30 January 2006
- "History of Acupuncture in China." Acupuncture Care. 2 February 2006 <http://www.acupuncturecare.com/acupunct.htm>
- Howard, Cori. "An Ancient Helper for Making a Baby." Maclean’s 23 January 2006: 40. Academic Search Premier. EBSCO. 30 January 2006
- Carter B (July 4th, 2007). "Is Acupuncture Safe?". ArticlesLog.com. Retrieved 2007-07-20.
{{cite web}}: Check date values in:|date=(help) - Health Professions Regulatory Advisory Council, Minister’s Referral Letter January 18, 2006 – Traditional Chinese Medicine (TCM) <http://www.hprac.org/english/projects.asp> 20 March 2006
- Porkert, Manfred (1974). The theoretical foundations of Chinese medicine: systems of correspondence. Cambridge, Mass: MIT Press. ISBN 0-262-16058-7.
- Wu MT, Hsieh JC, Xiong J; et al. (1999). "Central nervous pathway for acupuncture stimulation: localization of processing with functional MR imaging of the brain--preliminary experience". Radiology. 212 (1): 133–41. PMID 10405732.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link)
Footnotes
- Whole Medical Systems: An Overview [NCCAM Backgrounder]
- Energy Medicine: An Overview [NCCAM Backgrounder]
- ABC Chinese-English Comprehensive Dictionary edited by John DeFrancis, as used in Wenlin version 3.4.1
- ^ Ernst E, Pittler MH, Wider B, Boddy K. (2007). "Acupuncture: its evidence-base is changing". Am J Chin Med. 35 (1): 21–5. PMID 17265547.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lee A, Done ML (2004). "Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting". Cochrane database of systematic reviews (Online) (3): CD003281. doi:10.1002/14651858.CD003281.pub2. PMID 15266478.
- Dibble SL, Luce J, Cooper BA, Israel J, Cohen M, Nussey B, Rugo H (2007). "Acupressure for chemotherapy-induced nausea and vomiting: a randomized clinical trial". Oncol Nurs Forum. 34 (4): 813–20. doi:10.1188/07.ONF.xxx-xxx. PMID 17723973.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Furlan AD, van Tulder MW, Cherkin DC; et al. (2005). "Acupuncture and dry-needling for low back pain". Cochrane database of systematic reviews (Online) (1): CD001351. doi:10.1002/14651858.CD001351.pub2. PMID 15674876.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Manheimer E, White A, Berman B, Forys K, Ernst E (2005). "Meta-analysis: acupuncture for low back pain" (PDF). Ann. Intern. Med. 142 (8): 651–63. PMID 15838072.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Trinh K, Graham N, Gross A, Goldsmith C, Wang E, Cameron I, Kay T (2007). "Acupuncture for neck disorders". Spine. 32 (2): 236–43. PMID 17224820.
{{cite journal}}: CS1 maint: multiple names: authors list (link) Cite error: The named reference "Trinh K" was defined multiple times with different content (see the help page). - Trinh KV, Graham N, Gross AR; et al. (2006). "Acupuncture for neck disorders". Cochrane Database of Systematic Reviews (3). doi:10.1002/14651858.CD004870.pub3.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - The Cochrane Collaboration - Acupuncture for idiopathic headache. Melchart D, Linde K, Berman B, White A, Vickers A, Allais G, Brinkhaus B
- Cochrane Collaboration. [Search all Cochrane reviews for "acupuncture", retrieved 30 January 2008.
- Acupuncture and related interventions for smoking cessation
- Acupuncture for shoulder pain
- ^ Lewith GT, White PJ, Pariente J (2005). "Investigating acupuncture using brain imaging techniques: the current state of play". Evidence-based complementary and alternative medicine : eCAM. 2 (3): 315–9. doi:10.1093/ecam/neh110. PMID 16136210. Retrieved 2007-03-06.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ NIH Consensus Development Program (November 3–5, 1997). "Acupuncture --Consensus Development Conference Statement". National Institutes of Health. Retrieved 2007-07-17.
{{cite web}}: CS1 maint: date format (link) - ^ "Get the Facts, Acupuncture". National Institute of Health. 2006. Retrieved 2006-03-02.
- ^ Ernst G, Strzyz H, Hagmeister H (2003). "Incidence of adverse effects during acupuncture therapy-a multicentre survey". Complementary therapies in medicine. 11 (2): 93–7. PMID 12801494.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Felix Mann: "...acupuncture points are no more real than the black spots that a drunkard sees in front of his eyes." (Mann F. Reinventing Acupuncture: A New Concept of Ancient Medicine. Butterworth Heinemann, London, 1996,14.) Quoted by Matthew Bauer in Chinese Medicine Times, Vol 1 Issue 4 - Aug 2006, "The Final Days of Traditional Beliefs? - Part One"
- Kaptchuk, 1983, pp. 34-35
- Medical Acupuncture - Spring / Summer 2000- Volume 12 / Number 1
- Felix Mann, quoted by Matthew Bauer in Chinese Medicine Times, vol 1 issue 4, Aug. 2006, "The Final Days of Traditional Beliefs? - Part One"
- Skeptic's Dictionary on pseudoscience.
- Skeptic's Dictionary on acupuncture.
- Sampson, Wallace Sampson (1996). "Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 2)". Skeptical Inquirer. 20 (5). Retrieved 2007-01-06.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - Ulett GA, Acupuncture update 1984, Southern Medical Journal 78:233234, 1985. Comment found at NCBI - Traditional and evidence-based acupuncture: history, mechanisms, and present status. Ulett GA, Han J, Han S.
- MoonDragon's Health & Wellness Therapy: Acupuncture
- Acupuncture
- Medical Acupuncture Review: Safety, Efficacy, And Treatment Practices. Steven E. Braverman, MD
- ^ The World Health Organization Viewpoint On Acupuncture
- Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea. Proctor ML, Smith CA, Farquhar CM, Stones RW
- Parameter error in {{PMID}}: Missing PMID.
- Pomeranz B, Chiu D (1976). "Naloxone blockade of acupuncture analgesia: endorphin implicated". Life Sci. 19 (11): 1757–62. PMID 187888.
-
Mayer DJ, Price DD, Rafii A (1977). "Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone". Brain Res. 121 (2): 368–72. PMID 832169.
{{cite journal}}: CS1 maint: multiple names: authors list (link) -
Eriksson SV, Lundeberg T, Lundeberg S (1991). "Interaction of diazepam and naloxone on acupuncture induced pain relief". Am. J. Chin. Med. 19 (1): 1–7. PMID 1654741.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Bishop B. - Pain: its physiology and rationale for management. Part III. Consequences of current concepts of pain mechanisms related to pain management. Phys Ther. 1980, 60:24-37.
- Amanzio, M., Pollo, A., Maggi, G., Benedetti, F. (2001). "Response Variability to Analgesics: a Role for Non-specific Activation of Endogenous Opioids". Pain. 90 (3): 205–215.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Sandrew BB, Yang RC, Wang SC (1978). "Electro-acupuncture analgesia in monkeys: a behavioral and neurophysiological assessment". Archives internationales de pharmacodynamie et de thérapie. 231 (2): 274–84. PMID 417686.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Melzack R, Stillwell DM, Fox EJ (1977). "Trigger points and acupuncture points for pain: correlations and implications". Pain. 3 (1): 3–23. PMID 69288.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Li K, Shan B, Xu J; et al. (2006). "Changes in FMRI in the human brain related to different durations of manual acupuncture needling". Journal of alternative and complementary medicine (New York, N.Y.). 12 (7): 615–23. doi:10.1089/acm.2006.12.615. PMID 16970531.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Pariente J, White P, Frackowiak RS, Lewith G (2005). "Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture". Neuroimage. 25 (4): 1161–7. doi:10.1016/j.neuroimage.2005.01.016. PMID 15850733.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Shen J (2001). "Research on the neurophysiological mechanisms of acupuncture: review of selected studies and methodological issues". Journal of alternative and complementary medicine (New York, N.Y.). 7 Suppl 1: S121-7. doi:10.1089/107555301753393896. PMID 11822627.
- Liu JL, Han XW, Su SN (1990). "The role of frontal neurons in pain and acupuncture analgesia". Sci. China, Ser. B, Chem. Life Sci. Earth Sci. 33 (8): 938–45. PMID 2242217.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Wagner, T.D., Rilling, J.K., Smith, E.E., Sokolik, A., Casey, K.L.; et al. (2007). "Placebo-Induced Changes in fMRI in the Anticipation and Experience of Pain". Science. 303 (5661): 1162-1167.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Tsuchiya M, Sato EF, Inoue M, Asada A (2007). "Acupuncture enhances generation of nitric oxide and increases local circulation". Anesth. Analg. 104 (2): 301–7. doi:10.1213/01.ane.0000230622.16367.fb. PMID 17242084.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Blom M, Lundeberg T, Dawidson I, Angmar-Månsson B (1993). "Effects on local blood flux of acupuncture stimulation used to treat xerostomia in patients suffering from Sjögren's syndrome". Journal of oral rehabilitation. 20 (5): 541–8. PMID 10412476.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lundeberg T (1993). "Peripheral effects of sensory nerve stimulation (acupuncture) in inflammation and ischemia". Scandinavian journal of rehabilitation medicine. Supplement. 29: 61–86. PMID 8122077.
- Okmedi.net: The Bonghan Theory by Kim, Bong-Han
- HS Shin, HM Johng, BC Lee, S Cho, KS Soh, KY Baik, JS Yoo, KS Soh, Feulgen reaction study of novel threadlike structures (Bonghan ducts) on the surfaces of mammalian organs, Anatomical record. Part B New anatomist, 284(1), pp. 35-40, 2005. (Feature article)
- Biomedical Physics Laboratory for Korean Medicine, School of Physics, Seoul National University, South Korea. This lab. studies on the Bonghan system.
- White AR, Filshie J, Cummings TM (2001). "Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding". Complement Ther Med. 9 (4): 237–245. PMID 12184353.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Johnson MI (2006). "The clinical effectiveness of acupuncture for pain relief--you can be certain of uncertainty". Acupunct Med. 24 (2): 71–9. PMID 16783282.
- Furlan AD, van Tulder MW, Cherkin DC; et al. (2005). "Acupuncture and dry-needling for low back pain". Cochrane database of systematic reviews (Online) (1): CD001351. doi:10.1002/14651858.CD001351.pub2. PMID 15674876.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Manheimer E, White A, Berman B, Forys K, Ernst E (2005). "Meta-analysis: acupuncture for low back pain" (PDF). Ann. Intern. Med. 142 (8): 651–63. PMID 15838072.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Chou R, Huffman LH (2007). "Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline". Ann Intern Med. 147 (7): 492–504. PMID 17909210.
- For nausea, acupuncture at first appeared to be more effective than antiemetic drugs, per Lee and Done (2006); however, the authors later retracted this conclusion, finding that publication bias (in Asian countries) had skewed their results, and that acupuncture's efficacy in treating nausea did not exceed (but approximately equalled) that of antiemetic prophylaxis. Lee A, Copas JB, Henmi M, Gin T, Chung RC (2006). "Publication bias affected the estimate of postoperative nausea in an acupoint stimulation systematic review". J Clin Epidemiol. 59 (9): 980–3. PMID 16895822.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Ezzo JM, Richardson MA, Vickers A; et al. (2006). "Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting". Cochrane database of systematic reviews (Online) (2): CD002285. doi:10.1002/14651858.CD002285.pub2. PMID 16625560.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Acupuncture for idiopathic headache
- Acupuncture for osteoarthritis
- Meta-analysis: acupuncture for osteoarthritis of the knee
- Mayhew E, Ernst E (2007). "Acupuncture for fibromyalgia--a systematic review of randomized clinical trials". Rheumatology (Oxford, England). 46 (5): 801–4. doi:10.1093/rheumatology/kel406. PMID 17189243.
- Message to complementary and alternative medicine: evidence is a better friend than power. Andrew J Vickers
- "Report 12 of the Council on Scientific Affairs (A-97) -- Alternative Medicine". American Medical Association. 1997.
- Haake M, Müller HH, Schade-Brittinger C; et al. (2007). "German Acupuncture Trials (GERAC) for Chronic Low Back Pain: Randomized, Multicenter, Blinded, Parallel-Group Trial With 3 Groups". Arch. Intern. Med. 167 (17): 1892–8. doi:10.1001/archinte.167.17.1892. PMID 17893311.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - BBC NEWS, Acupuncture 'best for back pain'
- Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes MG, Weidenhammer W, Willich SN, Melchart D (2005). "Acupuncture for patients with migraine: a randomized controlled trial". JAMA. 293 (17): 2118–25. PMID 15870415.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Ann Intern Med - Rapid Responses for Scharf et al., 145 (1) 12-20
- Lao L, Hamilton GR, Fu J, Berman BM (2003). "Is acupuncture safe? A systematic review of case reports". Alternative therapies in health and medicine. 9 (1): 72–83. PMID 12564354.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Norheim AJ (1996). "Adverse effects of acupuncture: a study of the literature for the years 1981-1994". Journal of alternative and complementary medicine (New York, N.Y.). 2 (2): 291–7. PMID 9395661.
- Leow TK (2001). "Pneumothorax Using Bladder 14". Medical Acupuncture. 16 (2).
- Yekeler, Ensar. "Frequency of Sternal Variations and Anomalies Evaluated by MDCT". American Journal of Roentgenology. doi:10.2214. Retrieved 2007-11-24.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - "More than half of the physicians (59%) believed that acupuncture can be effective to some extent." Physicians Divided on Impact of CAM on U.S. Health Care; Aromatherapy Fares Poorly; Acupuncture Touted. HCD Research, 9 Sept. 2005.