| Revision as of 11:56, 24 January 2021 editBigdan201 (talk | contribs)Extended confirmed users2,409 edits restoring Risk section, there was no need to delete this.← Previous edit | Latest revision as of 01:19, 6 June 2024 edit undoCitation bot (talk | contribs)Bots5,407,951 edits Altered title. | Use this bot. Report bugs. | Suggested by Abductive | Category:Circumcision | #UCB_Category 23/36 | ||
| (281 intermediate revisions by 42 users not shown) | |||
| Line 1: | Line 1: | ||
| {{ |
{{Short description|Overview of relationship between male circumcision and HIV}} | ||
| {{About|male circumcision and HIV|female circumcision and HIV|Female genital mutilation#HIV}} | |||
| The relationship between '''circumcision and HIV''' has been researched since the late 1980s. Male ] reduces the risk of ] from HIV+ women to men.<ref name=farley>{{cite journal |vauthors=Farley TM, Samuelson J, Grabowski MK, Ameyan W, Gray RH, Baggaley R |title=Impact of male circumcision on risk of HIV infection in men in a changing epidemic context - systematic review and meta-analysis |journal=J Int AIDS Soc |volume=23 |issue=6 |pages=e25490 |date=June 2020 |pmid=32558344 |pmc=7303540 |doi=10.1002/jia2.25490 |type=Review}}</ref><ref>{{Cite book| vauthors = Jameson JL, Kasper DL, Longo DL, ], Hauser SL, Loscalzo J |title=Harrison's Principles of Internal Medicine|publisher= McGraw-Hill Education |year=2018|isbn=978-1-259-64403-0|edition=20th|location=New York|pages=1400|oclc=1029074059}}</ref> | |||
| Male ] reduces the risk of ] from HIV positive women to men in high risk populations.<ref>{{Cite journal |last1=Sharma |first1=Adhikarimayum Lakhikumar |last2=Hokello |first2=Joseph |last3=Tyagi |first3=Mudit |date=2021-06-25 |title=Circumcision as an Intervening Strategy against HIV Acquisition in the Male Genital Tract |journal=Pathogens |volume=10 |issue=7 |pages=806 |doi=10.3390/pathogens10070806 |pmid=34201976 |pmc=8308621 |issn=2076-0817 |quote=There is disputed immunological evidence in support of MC in preventing the heterosexual acquisition of HIV-1.|doi-access=free }}</ref><ref name=":0">{{Cite book |last1=Merson |first1=Michael |title=The AIDS Pandemic: Searching for a Global Response |last2=Inrig |first2=Stephen |publisher=] |year=2017 |isbn=9783319471334 |pages=379 |quote=This led to a consensus that male circumcision should be a priority for HIV prevention in countries and regions with heterosexual epidemics and high HIV and low male circumcision prevalence.}}</ref> | |||
| In |
In 2020, the ] (WHO) reiterated that male circumcision is an efficacious intervention for HIV prevention if carried out by medical professionals under safe conditions.<ref name="WHO-PrevHIV">{{cite web|title=Preventing HIV Through Safe Voluntary Medical Male Circumcision For Adolescent Boys And Men In Generalized HIV Epidemics | ||
| |year=2020|publisher=]|url=https://www.who.int/publications/i/item/978-92-4-000854-0 |access-date=2021-05-24}}</ref> | |||
| Circumcision reduces the risk that a man will acquire HIV and other ] (STIs) from an infected female partner through ].<ref name="CDCPrevHIV2018">{{cite report|title=Information for providers counseling male patients and parents regarding male circumcision and the prevention of HIV infection, STIs, and other health outcomes|publisher=]|date=August 22, 2018|url=https://stacks.cdc.gov/view/cdc/58456|access-date=2021-05-26|archive-date=2021-05-06|archive-url=https://web.archive.org/web/20210506034452/https://stacks.cdc.gov/view/cdc/58456|url-status=live}}</ref> The evidence regarding whether circumcision helps prevent HIV is not as clear among ] (MSM).<ref name="WHO-PrevHIV" /> The effectiveness of using circumcision to prevent HIV in the ] is not determined.<ref name="WHO-PrevHIV" /><ref name="kim_2010" /> | |||
| </ref><ref name="WHOpr0307">{{cite web |title=WHO and UNAIDS announce recommendations from expert consultation on male circumcision for HIV prevention |publisher=World Health Organisation |date=March 2007 |url=https://www.who.int/hiv/mediacentre/news68/en/index.html}}</ref> The ] (CDC) states that circumcision reduces the risk that a man will acquire HIV and other ] (STIs) from an infected female partner.{{medcn|date=August 2020}} | |||
| ==Efficacy== | ==Efficacy== | ||
| === Heterosexual men === | === Heterosexual men === | ||
| {{as of|2020}}, past research has shown that circumcision reduces the risk of HIV infection in heterosexual men, although these studies have had limitations.<ref name="farley">{{cite journal |vauthors=Farley TM, Samuelson J, Grabowski MK, Ameyan W, Gray RH, Baggaley R |title=Impact of male circumcision on risk of HIV infection in men in a changing epidemic context - systematic review and meta-analysis |journal=J Int AIDS Soc |volume=23 |issue=6 |pages=e25490 |date=June 2020 |pmid=32558344 |pmc=7303540 |doi=10.1002/jia2.25490 |type=Review}}</ref> | |||
| {{asof|2020}}, circumcision is well-established as being effective at reducing the risk of HIV infection in heterosexual men.<ref name=farley/> | |||
| The WHO Expert Group on Models To Inform Fast Tracking Voluntary Medical Male Circumcision In HIV Combination Prevention in 2016 found "large benefits" of circumcision in settings with high HIV prevalence and low circumcision prevalence. The Group estimated male circumcision is cost-saving in almost all high priority countries. Furthermore, WHO stated that: "While circumcision reduces a man’s individual lifetime HIV risk, the indirect effect of preventing further HIV transmissions to women, their babies (vertical transmission) and from women to other men has an even greater impact on the population incidence, particularly for circumcisions performed at younger ages (under age | |||
| The ], to prevent one HIV infection during ten years, is between five and fifteen men. The UNAIDS/WHO/SACEMA Expert Group on Modelling the Impact and Cost of Male Circumcision for HIV Prevention found "large benefits" of circumcision in settings with high HIV prevalence and low circumcision prevalence. The Group estimated "one HIV infection being averted for every five to fifteen male circumcisions performed, and costs to avert one HIV infection ranging from US$150 to US$900 using a 10-y time horizon".{{old fact|2020|8|13}}<ref>{{cite journal | vauthors = Hankins C, Hargrove J, Williams B, Abu Raddad L, Auvert B, Bollinger L, Dorrington R, Ghani A, Gray R, Hallett T, Kahn JG | display-authors = 6 | collaboration = UNAIDS/WHO/SACEMA Expert Group on Modelling the Impact and Cost of Male Circumcision for HIV Prevention | title = Male circumcision for HIV prevention in high HIV prevalence settings: what can mathematical modelling contribute to informed decision making? | journal = PLOS Medicine | volume = 6 | issue = 9 | pages = e1000109 | date = September 2009 | pmid = 19901974 | pmc = 2731851 | doi = 10.1371/journal.pmed.1000109 | type = Review }}</ref> The World Health Organisation states that circumcision is "highly cost-effective" in comparison to other HIV interventions when data from the South African trial are used, but less cost-effective when data from the Ugandan trial are used.<ref name="WHO-GTPDSA" /> | |||
| 25 years)."<ref name="WHOModel2016">{{cite web |title=Models To Inform Fast Tracking Voluntary Medical Male Circumcision In HIV Combination Prevention | |||
| |publisher=World Health Organization |date=March 2016 |url=https://apps.who.int/iris/bitstream/handle/10665/259706/WHO-HIV-2017.39-eng.pdf|access-date=2021-05-26 |archive-date=2020-09-23 |archive-url=https://web.archive.org/web/20200923203154/https://apps.who.int/iris/bitstream/handle/10665/259706/WHO-HIV-2017.39-eng.pdf|url-status=live }}</ref> | |||
| Newly circumcised HIV infected men who are not taking ] can ] the HIV virus from the circumcision wound, thus increasing the immediate risk of HIV transmission to female partners.<ref name="WHO-PrevHIV" /> This risk of post-operative transmission presents a challenge, although in the long-term it is possible the circumcision of HIV-infected men helps lessen heterosexual HIV transmission overall. Such viral shedding can be mitigated by the use of antiretroviral drugs.<ref>{{cite journal |vauthors=Tobian AA, Adamu T, Reed JB, Kiggundu V, Yazdi Y, Njeuhmeli E |title=Voluntary medical male circumcision in resource-constrained settings |journal=Nat Rev Urol |volume=12 |issue=12 |pages=661–70 |date=December 2015 |pmid=26526758 |doi=10.1038/nrurol.2015.253 |s2cid=10432723 |type=Review}}</ref> Additional research is needed to ascertain the existence and potential risk of viral shedding from circumcision wounds. | |||
| === Men who have sex with men === | |||
| A 2008 meta-analysis of gay and bisexual men (52% circumcised) found that the rate of HIV infection was not lower among men who were circumcised.<ref name="Millett">{{cite journal | vauthors = Yuan T, Fitzpatrick T, Ko NY, Cai Y, Chen Y, Zhao J, Li L, Xu J, Gu J, Li J, Hao C, Yang Z, Cai W, Cheng CY, Luo Z, Zhang K, Wu G, Meng X, Grulich AE, Hao Y, Zou H | display-authors = 6 | title = Circumcision to prevent HIV and other sexually transmitted infections in men who have sex with men: a systematic review and meta-analysis of global data | journal = The Lancet. Global Health | volume = 7 | issue = 4 | pages = e436–e447 | date = April 2019 | pmid = 30879508 | doi = 10.1016/S2214-109X(18)30567-9 | pmc = 7779827 | doi-access = free }}</ref> For men who engaged primarily in insertive anal sex, no effect was observed. Observational studies included in the meta-analysis that were conducted prior to the introduction of ] in 1996 demonstrated a protective effect for circumcised ] (MSM) against HIV infection.<ref name="Millett" /> | |||
| ===Men who have sex with men=== | |||
| Reviews in 2011<ref>{{cite journal | vauthors = Wiysonge CS, Kongnyuy EJ, Shey M, Muula AS, Navti OB, Akl EA, Lo YR | title = Male circumcision for prevention of homosexual acquisition of HIV in men | journal = The Cochrane Database of Systematic Reviews | issue = 6 | pages = CD007496 | date = June 2011 | pmid = 21678366 | doi = 10.1002/14651858.CD007496.pub2 }}</ref> and 2018 found some evidence that circumcision was protective in MSM.<ref>{{cite journal | vauthors = Sharma SC, Raison N, Khan S, Shabbir M, Dasgupta P, Ahmed K | title = Male circumcision for the prevention of human immunodeficiency virus (HIV) acquisition: a meta-analysis | journal = BJU International | volume = 121 | issue = 4 | pages = 515–526 | date = April 2018 | pmid = 29232046 | doi = 10.1111/bju.14102 | doi-access = free }}</ref> | |||
| The ] does not recommend circumcision as protection against male to male HIV transmission, as evidence is lacking in regards to receptive anal intercourse. The WHO also states that ] should not be excluded from circumcision services in countries in eastern and southern ], and that circumcision may be effective at limiting the spread of HIV for MSM if they also engage in vaginal sex with women.<ref name="WHO-PrevHIV" /> | |||
| ===Regional differences=== | |||
| A 2019 ] of MSM found circumcision was associated with a 42% reduction in the odds of HIV in low and middle income countries, but not in high income countries.<ref name="Millett" /> The CDC stated in 2013: "There are as yet no convincing data to help determine whether male circumcision will have any effect on HIV risk for men who engage in anal sex with either a female or male partner, as either the insertive or receptive partner."{{old fact|2020|8|13}}<ref name="CDC-2013">{{old fact|2020|8|13}}{{cite web |title=Male Circumcision |publisher=Centers for Disease Control and Prevention |year=2013 |url=https://www.cdc.gov/hiv/prevention/research/malecircumcision/ |archive-url=https://web.archive.org/web/20131221002411/http://www.cdc.gov/hiv/prevention/research/malecircumcision/ |archive-date=2013-12-21}}</ref> | |||
| Whether circumcision is beneficial to developed countries for HIV prevention purposes is undetermined.<ref name="WHO-PrevHIV" /><ref name="kim_2010">{{cite journal |vauthors=Kim HH, Li PS, Goldstein M |title=Male circumcision: Africa and beyond? |journal=Curr Opin Urol |volume=20 |issue=6 |pages=515–9 |date=November 2010 |pmid=20844437 |doi=10.1097/MOU.0b013e32833f1b21 |s2cid=2158164 |url=}}</ref> It is not known whether the effect of male circumcision differs by HIV-1 variant. The predominant subtype of HIV-1 in the ] is subtype B, and in Africa, the predominant subtypes are A, C, and D.<ref>{{Cite journal|doi = 10.1186/s12301-019-0005-2|title = Male circumcision and global HIV/AIDS epidemic challenges|year = 2019|last1 = Olapade-Olaopa|first1 = Emiola Oluwabunmi|last2 = Salami|first2 = Mudasiru Adebayo|last3 = Lawal|first3 = Taiwo Akeem|journal = African Journal of Urology|volume = 25|s2cid = 208085886|doi-access = free}}</ref> | |||
| ==Recommendations== | ==Recommendations== | ||
| <!-- dummy edit; can be deleted. --> | |||
| {{synthesis|section|date=October 2020}} | |||
| The most recent WHO review of the evidence reiterates prior estimates of the impact of male circumcision on HIV incidence rates. In 2020, WHO again concluded that male circumcision is an efficacious intervention for HIV prevention and that the promotion of male circumcision is an essential strategy, in addition to other preventive measures, for the prevention of heterosexually acquired HIV infection in men. Eastern and southern Africa had a particularly low prevalence of circumcised males. This region has a disproportionately high HIV infection rate, with a significant | |||
| number of those infections stemming from heterosexual transmission. | |||
| The WHO has made voluntary medical male circumcision (VMMC) a priority intervention in that region since their 2007 recommendations.<ref name="WHO-PrevHIV" /> | |||
| {{blockquote|text=Although these results confirm that male circumcision reduces the risk of men becoming infected with HIV, the UN agencies emphasize that it does not provide complete protection against HIV infection. Circumcised men can still become infected with the virus and, if HIV-positive, can infect their sexual partners. Male circumcision should never replace other known effective prevention methods and should always be considered as part of a comprehensive prevention package, which includes correct and consistent use of male or female condoms, reduction in the number of sexual partners, delaying the onset of sexual relations, and HIV testing, counseling, and treatment.|author=World Health Organization|source=Joint WHO/UNAIDS Statement made in 2007.<ref name="WHOsec">{{cite press release | url = https://www.who.int/mediacentre/news/statements/2007/s04/en/index.html | title = WHO and UNAIDS Secretariat welcome corroborating findings of trials assessing impact of male circumcision on HIV risk | access-date = 2007-02-23 | date = February 23, 2007 | publisher = World Health Organization | archive-date = 2007-02-26 | archive-url = https://web.archive.org/web/20070226135123/http://www.who.int/mediacentre/news/statements/2007/s04/en/index.html | url-status = dead }}</ref>}} | |||
| In the United States, the ] (AAP) led a 2012 task force which included the ] (AAFP), the ] (ACOG), and the ] (CDC). The task force concluded that circumcision may be helpful for the prevention of HIV in the United States.<ref name="AAP_2012">{{cite journal |author=American Academy of Pediatrics Task Force on Circumcision |title=Technical Report |journal=Pediatrics |volume=130 |issue=3 |year=2012 |pages=e756–e785 |issn=0031-4005 |pmid=22926175 |doi=10.1542/peds.2012-1990 |url=http://pediatrics.aappublications.org/content/130/3/e756.full |url-status=live |archive-url=https://web.archive.org/web/20120920054623/http://pediatrics.aappublications.org/content/130/3/e756.full |archive-date=2012-09-20 |doi-access=free }}</ref> The CDC 2018 position on circumcision and HIV recommended that circumcision should continue to be offered to parents who are ] of the benefits and risks, including a potential reduction in risk of HIV transmission. The position asserts that circumcision conducted after sexual debut can result in missed opportunities for HIV prevention.<ref name="CDCPrevHIV2018" /> | |||
| {{quote|text=Although these results demonstrate that male circumcision reduces the risk of men becoming infected with HIV, the UN agencies emphasize that it does not provide complete protection against HIV infection. Circumcised men can still become infected with the virus and, if HIV-positive, can infect their sexual partners. Male circumcision should never replace other known effective prevention methods and should always be considered as part of a comprehensive prevention package, which includes correct and consistent use of male or female condoms, reduction in the number of sexual partners, delaying the onset of sexual relations, and HIV testing and counselling.|author=World Health Organization|source=Joint WHO/UNAIDS Statement.<ref name="WHOsec">{{cite press release| url =https://www.who.int/mediacentre/news/statements/2007/s04/en/index.html | title = WHO and UNAIDS Secretariat welcome corroborating findings of trials assessing impact of male circumcision on HIV risk | access-date = 2007-02-23 | date = February 23, 2007 | publisher = World Health Organization}}</ref>}} | |||
| Because the evidence that circumcision prevents HIV mainly comes from studies conducted in Africa, the ] (KNMG) |
Because the evidence that circumcision prevents HIV mainly comes from studies conducted in Africa, the ] (KNMG) questioned the applicability of those studies to developed countries. Circumcision has not been included in their HIV prevention recommendations. The KNMG circumcision policy statement was endorsed by several Dutch medical associations. The policy statement was initially released in 2010, but was reviewed again and accepted in 2022.<ref>{{Cite web|title=Non-therapeutic circumcision of male minors KNMG viewpoint|url=https://www.knmg.nl/advies-richtlijnen/dossiers/jongensbesnijdenis|date=31 March 2022}}</ref> | ||
| In the ], the ] (AAP) led a 2012 task force which included the ] (AAFP), the ] (ACOG), and the ] (CDC). The task force policy statement, found that circumcision may be helpful for the prevention of HIV in the United States. The AAP task force policy was endorsed by the ACOG.<ref name=AAP_2012>{{cite journal |author=American Academy of Pediatrics Task Force on Circumcision |title=Technical Report |journal=Pediatrics |volume=130 |issue=3 |year=2012 |pages=e756–e785 |issn=0031-4005 |pmid=22926175 |doi=10.1542/peds.2012-1990 |url=http://pediatrics.aappublications.org/content/130/3/e756.full |url-status=live |archive-url=https://web.archive.org/web/20120920054623/http://pediatrics.aappublications.org/content/130/3/e756.full |archive-date=2012-09-20 |doi-access=free }}</ref> The CDC expressed uncertainty if circumcision would help in the United States, stating the transmission patterns in the U.S. vary from those studied in the primary studies examined, namely the U.S. has a higher prevalence of MSM transmission. In line with the AAP task force, the CDC 2018 position on circumcision and HIV recommended that circumcision should continue to be offered to parents who are ] of the benefits and risks, including a potential reduction in risk of HIV transmission.<ref name="CDC2018" /> The CDC says that circumcision can be done in adulthood, when the man can make a decision for himself. Circumcision conducted after sexual debut can result in missed opportunities for HIV prevention.<ref name="CDC2018">{{cite web |title=Information for providers counseling male patients and parents regarding male circumcision and the prevention of HIV infection, STIs, and other health outcomes |url=https://stacks.cdc.gov/view/cdc/58456 |website=CDC stacks |publisher=] |access-date=26 August 2020}}</ref> | |||
| == Process == | |||
| The WHO recommends voluntary medical male circumcision, as opposed to circumcision by traditional healers or untrained individuals. {{cn|date=January 2021}} | |||
| Newly circumcised men must refrain from sexual activity until the wounds are fully healed. Some circumcised men might have a false sense of security that could lead to increased risky sexual behavior.<ref> | |||
| {{cite journal | vauthors = Kalichman S, Eaton L, Pinkerton S | title = Circumcision for HIV prevention: failure to fully account for behavioral risk compensation | journal = PLOS Medicine | volume = 4 | issue = 3 | pages = e138; author reply e146 | date = March 2007 | pmid = 17388676 | pmc = 1831748 | doi = 10.1371/journal.pmed.0040138 }}</ref> | |||
| ==Mechanism of action== | ==Mechanism of action== | ||
| While the biological mechanism of action is not known, a 2020 meta-analysis stated "the consistent protective effect suggests that the reasons for the heterogeneity lie in concomitant individual social and medical factors, such as presence of STIs, rather than a different biological impact of circumcision."<ref name=farley/> | While the biological mechanism of action is not known, a 2020 meta-analysis stated "the consistent protective effect suggests that the reasons for the heterogeneity lie in concomitant individual social and medical factors, such as presence of STIs, rather than a different biological impact of circumcision."<ref name="farley" /> The inner foreskin harbours an increased density of CD4 T-cells and releases increased levels of pro-inflammatory cytokines. Hence the sub-preputial space displays a pro-inflammatory environment, conducive to HIV infection.<ref>{{cite journal |last1=Prodger |first1=Jessica L. |title=The biology of how circumcision reduces HIV susceptibility: broader implications for the prevention field |journal=AIDS Research and Therapy |date=September 2017 |volume=14 |issue=1 |page=49 |doi=10.1186/s12981-017-0167-6|pmid=28893286 |pmc=5594533 |doi-access=free }}</ref> | ||
| ]s (part of the human immune system) under the foreskin may be a source of entry for HIV.<ref>{{cite journal | vauthors = Weiss HA, Dickson KE, Agot K, Hankins CA | title = Male circumcision for HIV prevention: current research and programmatic issues | journal = AIDS | volume = 24 | issue = Suppl 4 | pages = S61-9 | date = October 2010 | pmid = 21042054 | pmc = 4233247 | doi = 10.1097/01.aids.0000390708.66136.f4 | type = Randomized controlled trial }}</ref> Excising the foreskin removes what is thought to be a main entry point for the HIV virus.<ref>{{cite journal |vauthors=Szabo R, Short RV |title=How does male circumcision protect against HIV infection? |journal=BMJ |volume=320 |issue=7249 |pages=1592–4 |date=June 2000 |pmid=10845974 |pmc=1127372 |doi=10.1136/bmj.320.7249.1592 |type=Review}}</ref> | |||
| == Risk == | |||
| If proper hygienic procedures are not adhered to, the circumcision operation itself can spread HIV. Brewer ''et al.'' (2007)<ref>{{npsn|date=January 2014}}{{cite journal |type=Research article| last = Brewer | first= Devon |date=February 2007 | title = Male and Female Circumcision Associated with Prevalent HIV Infection in Virgins and Adolescents in Kenya, Lesotho, and Tanzania | journal = Annals of Epidemiology | volume = 17 | issue = 3 |pages=217–26 |url=http://www.annalsofepidemiology.org/article/PIIS1047279706002651/abstract | doi = 10.1016/j.annepidem.2006.10.010 | pmid = 17320788 | last2 = Potterat | first2 = JJ | last3 = Roberts Jr | first3 = JM | last4 = Brody | first4 = S}}</ref> report, " male and female virgins were substantially more likely to be HIV infected than uncircumcised virgins. Among adolescents, regardless of sexual experience, circumcision was just as strongly associated with prevalent HIV infection. However, uncircumcised adults were more likely to be HIV positive than circumcised adults." They concluded: "HIV transmission may occur through circumcision-related blood exposures in eastern and southern Africa." | |||
| An interim analysis from the Rakai Health Sciences Program in Uganda suggested that newly circumcised HIV positive men may be more likely to spread HIV to their female partners if they have sexual intercourse before the wound is fully healed. “Because the total number of men who resumed sex before certified wound healing is so small, the finding of increased transmission after surgery may have occurred by chance alone. However, we need to err on the side of caution to protect women in the context of any future male circumcision programme,” said Maria Wawer, the study's principal investigator.<ref>{{cite web | |||
| | url =http://www.aidsmap.com/en/news/3CBF12A3-A1AC-4A0E-A79C-54FC6EF93E28.asp | |||
| | author = Virginia Differding | |||
| | title = Women may be at heightened risk of HIV infection immediately after male partner is circumcised | |||
| | accessdate = 2007-03-14 | |||
| | date = March 12, 2007 | |||
| | publisher = Aidsmap News}} | |||
| </ref> | |||
| Kalichman ''et al.'' (2007) argue that any protective effects circumcision could offer would be partially offset by increased HIV risk behavior, or “risk compensation" including reduction in condom use or increased numbers of sex partners. They note that circumcised men in the South African trial had 18% more sexual contacts than uncircumcised men at follow-up. They also said that because participants were given ongoing risk-reduction counseling and free condoms, it "reduced the utility of these trials for estimating the potential behavioral impact of male circumcision when implemented in a natural setting." They also criticised current models for failing to account for increased HIV risk behaviour. Increased HIV risk behaviour would mean more women would be infected which would consequently increase the risk of men. It would also mean that non-HIV STI's, which have been associated with increased HIV risk, would increase.<ref name="kalichman">{{cite journal | |||
| |type=Letter | |||
| | last = Kalichman | |||
| | first = S | |||
| |author2=Eaton L|author3=Pinkerton S | |||
| | date = March 27, 2007 | |||
| | title = Circumcision for HIV Prevention: Failure to Fully Account for Behavioral Risk Compensation | |||
| | journal = ] | |||
| | volume = 4 | |||
| | issue = 3 | |||
| | pages = e138 | |||
| | pmid = | |||
| 17388676 | |||
| | pmc = 1831748| doi = 10.1371/journal.pmed.0040138 | |||
| | url = http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0040138 | |||
| | accessdate = 2008-10-08 | |||
| }} | |||
| </ref> | |||
| The ] of HIV infection, defined as the rate of HIV infection in circumcised divided by rate in uncircumcised men, is 0.42 (95% ] 0.31-0.57),<ref name="weiss2008">{{cite journal | |||
| |type= Editorial, review | |||
| |author=Weiss HA, Halperin D, Bailey RC, Hayes RJ, Schmid G, Hankins CA | |||
| |title=Male circumcision for HIV prevention: from evidence to action? | |||
| |journal=AIDS | |||
| |volume=22 | |||
| |issue=5 | |||
| |pages=567–74 | |||
| |date=March 2008 | |||
| |pmid=18316997 | |||
| |doi=10.1097/QAD.0b013e3282f3f406 | |||
| |url= http://www.aidsvaccineclearinghouse.org/pdf/MC/Weiss_AIDS_2008.pdf|format=PDF}}</ref> 0.44 (0.33-0.60)<ref name="mills2008">{{cite journal | |||
| |author=Mills E, Cooper C, Anema A, Guyatt G | |||
| |title=Male circumcision for the prevention of heterosexually acquired HIV infection: a meta-analysis of randomized trials involving 11,050 men | |||
| |journal=HIV Med. | |||
| |volume=9 | |||
| |issue=6 | |||
| |pages=332–5 | |||
| |date=July 2008 | |||
| |pmid=18705758 | |||
| |doi=10.1111/j.1468-1293.2008.00596.x | |||
| |url=}}</ref> and 0.43 (0.32-0.59)<ref name="byakika2008">{{cite journal | |||
| |type=Meta-analysis | |||
| |author=Byakika-Tusiime J | |||
| |title=Circumcision and HIV Infection: Assessment of Causality | |||
| |journal=AIDS Behav | |||
| |volume=12 | |||
| |issue=6 | |||
| |pages=835–41 | |||
| |date=September 2008 | |||
| |pmid=18800244 | |||
| |doi=10.1007/s10461-008-9453-6 | |||
| |url=}}</ref> as reported in the publications ], ], and ] respectively. Weiss ''et al.'' report that meta-analysis of "as-treated" figures from ] reveals a stronger protective effect (0.35; 95% CI 0.24-0.54) than if "intention-to-treat" figures are used.<ref name="weiss2008"/> Byakika-Tusiime also estimated a summary relative risk of 0.39 (0.27-0.56) for observational studies, and 0.42 (0.33-0.53) overall (including both observational and RCT data).<ref name="byakika2008"/> Weiss ''et al.'' report that the estimated relative risk using RCT data was "identical" to that found in observational studies (0.42).<ref name="weiss2008"/> Byakika-Tusiime states that available evidence satisfies six of ], and concludes that the results of her analysis "provide unequivocal evidence that circumcision plays a causal role in reducing the risk of HIV infection among men."<ref name="byakika2008"/> Mills ''et al.'' conclude that circumcision is an "effective strategy for reducing new male HIV infections", but caution that consistently safe sexual practices will be required to maintain the protective effect at the population level.<ref name="mills2008"/> Weiss ''et al.'' conclude that the evidence from the trials is conclusive, but that challenges to implementation remain, and will need to be faced.<ref name="weiss2008"/> Lei ''et al.'' found that the relative risk of HIV acquisition by HIV- men having sex with women was 0.30. The authors also found that circumcision did not protect against HIV infection among women.<ref>{{cite journal|last1=Lei|first1=JH|last2=Liu|first2=LR|last3=Wei|first3=Q|last4=Yan|first4=SB|last5=Yang|first5=L|last6=Song|first6=TR|last7=Yuan|first7=HC|last8=Lv|first8=X|last9=Han|first9=P|title=Circumcision Status and Risk of HIV Acquisition during Heterosexual Intercourse for Both Males and Females: A Meta-Analysis.|journal=PLOS ONE|date=2015|volume=10|issue=5|pages=e0125436|doi=10.1371/journal.pone.0125436|pmid=25942703}}</ref> | |||
| ==History== | ==History== | ||
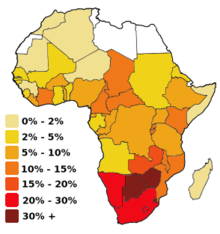
| ] based on 1999–2001 figures]] | ] based on 1999–2001 figures]] | ||
| Valiere Alcena, in a 1986 letter to the ''New York State Journal of Medicine,'' noted that low rates of circumcision in parts of Africa had been linked to the ].<ref name="taken">{{cite journal |type= Comment | vauthors = Alcena V |title = AIDS in Third World countries |journal= PLOS Medicine |date = 19 October 2006| volume = 86 | issue = 8 | page = 446 | pmid = 3463895 |url = http://www.plosmedicine.org/annotation/listThread.action?root=15231}}</ref><ref>{{cite journal |type = Letter | |
Valiere Alcena, in a 1986 letter to the ''New York State Journal of Medicine,'' noted that low rates of circumcision in parts of Africa had been linked to the ].<ref name="taken">{{cite journal | type = Comment | vauthors = Alcena V | title = AIDS in Third World countries | journal = PLOS Medicine | date = 19 October 2006 | volume = 86 | issue = 8 | page = 446 | pmid = 3463895 | url = http://www.plosmedicine.org/annotation/listThread.action?root=15231 | access-date = 10 January 2014 | archive-date = 10 January 2014 | archive-url = https://web.archive.org/web/20140110204325/http://www.plosmedicine.org/annotation/listThread.action?root=15231 | url-status = dead }}</ref><ref>{{cite journal |type = Letter |vauthors = Alcena V |title = AIDS in Third World countries |journal = New York State Journal of Medicine |volume = 86 |issue = 8 |pages = 446 |date = August 1986 |pmid = 3463895 |url = http://www.popline.org/node/363663 |access-date = 2014-01-10 |archive-date = 2014-01-10 |archive-url = https://web.archive.org/web/20140110194304/http://www.popline.org/node/363663 |url-status = live }}</ref> Aaron J. Fink several months later also proposed that circumcision could have a preventive role when the '']'' published his letter, "A possible explanation for heterosexual male infection with AIDS," in October, 1986.<ref>{{cite journal | vauthors = Fink AJ | title = A possible explanation for heterosexual male infection with AIDS | journal = The New England Journal of Medicine | volume = 315 | issue = 18 | pages = 1167 | date = October 1986 | pmid = 3762636 | doi = 10.1056/nejm198610303151818 | type = Letter }}</ref> By 2000, over 40 epidemiological studies had been conducted to investigate the relationship between circumcision and HIV infection.<ref name="Szabo">{{cite journal | vauthors = Szabo R, Short RV | title = How does male circumcision protect against HIV infection? | journal = BMJ | volume = 320 | issue = 7249 | pages = 1592–4 | date = June 2000 | pmid = 10845974 | pmc = 1127372 | doi = 10.1136/bmj.320.7249.1592 | type = Review }}</ref> A meta-analysis conducted by researchers at the ] examined 27 studies of circumcision and HIV in sub-Saharan Africa and concluded that these showed circumcision to be "associated with a significantly reduced risk of HIV infection" that could form part of a useful public health strategy.<ref name="Weiss2000">{{cite journal | vauthors = Weiss HA, Quigley MA, Hayes RJ | s2cid = 21857086 | title = Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis | journal = AIDS | volume = 14 | issue = 15 | pages = 2361–70 | date = October 2000 | pmid = 11089625 | doi = 10.1097/00002030-200010200-00018 | url = http://www.aidsonline.com/pt/re/aids/pdfhandler.00002030-200010200-00018.pdf | url-status = dead | type = Meta-analysis | archive-url = https://web.archive.org/web/20140110151608/http://journals.lww.com/aidsonline/Fulltext/2000/10200/Male_circumcision_and_risk_of_HIV_infection_in.18.aspx | archive-date = 2014-01-10 }}</ref> A 2005 review of 37 observational studies expressed reservations about the conclusion because of possible ]s, since all studies to date had been observational as opposed to ]s. The authors stated that three randomized controlled trials then underway in Africa would provide "essential evidence" about the effects of circumcision on preventing HIV.<ref name="Siegfried2005">{{cite journal | vauthors = Siegfried N, Muller M, Deeks J, Volmink J, Egger M, Low N, Walker S, Williamson P | display-authors = 6 | title = HIV and male circumcision--a systematic review with assessment of the quality of studies | journal = The Lancet. Infectious Diseases | volume = 5 | issue = 3 | pages = 165–73 | date = March 2005 | pmid = 15766651 | doi = 10.1016/S1473-3099(05)01309-5 | type = Review }}</ref> | ||
| Experimental evidence was needed to establish a causal relationship, so three ]s (RCT) were commissioned as a means to reduce the effect of any confounding factors. Trials took place in ], ] and ].<ref name=":1">{{cite journal |vauthors=Siegfried N, Muller M, Deeks JJ, Volmink J |date=April 2009 |title=Male circumcision for prevention of heterosexual acquisition of HIV in men |journal=The Cochrane Database of Systematic Reviews |issue=2 |pages=CD003362 |doi=10.1002/14651858.CD003362.pub2 |pmid=19370585 |veditors=Siegfried N}}</ref> All three trials were stopped early by their monitoring boards because those in the circumcised group had a substantially lower rate of HIV incidence than the control group, and hence it was seen as unethical to withhold the procedure, in light of strong evidence of efficacy.<ref name=":1" /> In 2009, a ] which included the results of the three ]s found "strong" evidence that the acquisition of HIV by a man during sex with a woman was decreased by 54% (], 38% to 66%) over 24 months if the man was circumcised. The review also found a low incidence of adverse effects from circumcision in the trials reviewed.<ref name="Cochrane2009">{{cite journal |last1=Siegfried |first1=Nandi |last2=Muller |first2=Martie |last3=Deeks |first3=Jonathan J |last4=Volmink |first4=Jimmy |title=Male circumcision for prevention of heterosexual acquisition of HIV in men |journal=Cochrane Database of Systematic Reviews |date=15 April 2009 |issue=2 |pages=CD003362 |doi=10.1002/14651858.CD003362.pub2|pmid=19370585 }}</ref> WHO assessed the trials as "gold standard" studies and found "strong and consistent" evidence from later studies that confirmed the results.<ref name="WHO-PrevHIV" /> In 2020, a review including post-study follow up from the three randomized controlled trials, as well as newer observational studies, found a 59% relative reduction in HIV incidence, and 1.31% absolute decrease across the three randomized controlled trials, as well as continued protection for up to 6 years after the studies began.<ref>{{cite journal |last1=Farley |first1=Timothy MM |last2=Samuelson |first2=Julia |last3=Grabowski |first3=M Kate |last4=Ameyan |first4=Wole |last5=Gray |first5=Ronald H |last6=Baggaley |first6=Rachel |title=Impact of male circumcision on risk of HIV infection in men in a changing epidemic context – systematic review and meta-analysis |journal=Journal of the International AIDS Society |date=June 2020 |volume=23 |issue=6 |pages=e25490 |doi=10.1002/jia2.25490|pmid=32558344 |pmc=7303540 |doi-access=free }}</ref> | |||
| A 2005 review of 37 observational studies expressed reservations about the conclusion because of possible ]s, since all studies to date had been observational as opposed to ]s. The authors stated that three randomized controlled trials then underway in Africa would provide "essential evidence" about the effects of circumcision on preventing HIV.<ref name="Siegfried2005">{{cite journal | vauthors = Siegfried N, Muller M, Deeks J, Volmink J, Egger M, Low N, Walker S, Williamson P | display-authors = 6 | title = HIV and male circumcision--a systematic review with assessment of the quality of studies | journal = The Lancet. Infectious Diseases | volume = 5 | issue = 3 | pages = 165–73 | date = March 2005 | pmid = 15766651 | doi = 10.1016/S1473-3099(05)01309-5 | type = Review }}</ref> | |||
| == Society and culture == | |||
| In 2009, a ] which included the results of the three 2000s trials found "strong" evidence that the acquisition of HIV by a man during sex with a woman was decreased by 38% and 66% over 24 months if the man was circumcised. The review also found a low incidence of adverse effects from circumcision in the trials reviewed.<ref name="Cochrane2009">{{cite journal |last1=Siegfried |first1=Nandi |last2=Muller |first2=Martie |last3=Deeks |first3=Jonathan J |last4=Volmink |first4=Jimmy |title=Male circumcision for prevention of heterosexual acquisition of HIV in men |journal=Cochrane Database of Systematic Reviews |date=15 April 2009 |issue=2 |pages=CD003362 |doi=10.1002/14651858.CD003362.pub2|pmid=19370585 }}</ref> In 2020, a review including post-study follow up from the three randomized controlled trials, as well as newer observational studies, found a 59% reduction in HIV incidence across the three randomized controlled trials, as well as continued protection for up to 6 years after the studies began.<ref>{{cite journal |last1=Farley |first1=Timothy MM |last2=Samuelson |first2=Julia |last3=Grabowski |first3=M Kate |last4=Ameyan |first4=Wole |last5=Gray |first5=Ronald H |last6=Baggaley |first6=Rachel |title=Impact of male circumcision on risk of HIV infection in men in a changing epidemic context – systematic review and meta‐analysis |journal=Journal of the International AIDS Society |date=June 2020 |volume=23 |issue=6 |pages=e25490 |doi=10.1002/jia2.25490|pmid=32558344 |pmc=7303540 |doi-access=free }}</ref> | |||
| ] became the 1 millionth VMMC against HIV/AIDS transmission in the ] of ], ] in 2018.<ref>{{Cite web |last=Seeth |first=Avantika |date=June 1, 2018 |title='It's hassle-free,' says actor Melusi Yeni about his medical circumcision |url=https://www.news24.com/citypress/news/its-hassle-free-says-actor-melusi-yeni-about-his-medical-circumcision-20180601 |access-date=September 6, 2022|website=] |language=en-US |quote=Actor Melusi Yeni was the millionth man to undergo voluntary male medical circumcision at the Sivananda Clinic in KwaZulu-Natal.}}</ref>]]The WHO recommends VMMC, as opposed to traditional circumcision. There is some evidence that traditionally circumcised men (i.e. who have been circumcised by a person who is not medically trained) use condoms less often and have higher numbers of sexual partners, increasing their risk of contracting HIV.{{r|WHO-PrevHIV|p=3/42}} Newly circumcised men must refrain from sexual activity until the wounds are fully healed.<ref name=WHO-PrevHIV/> | |||
| The prevalence of circumcision varies across Africa.<ref>{{cite journal | vauthors = Marck J | title = Aspects of male circumcision in sub-equatorial African culture history | journal = Health Transition Review | volume = 7 Suppl | issue = Suppl | pages = 337–60 | year = 1997 | pmid = 10173099 | url = http://htc.anu.edu.au/pdfs/Marck1.pdf | access-date = 2009-03-23 | url-status = dead | type = Review | archive-url = https://web.archive.org/web/20080906115430/http://htc.anu.edu.au/pdfs/Marck1.pdf | archive-date = 2008-09-06 }}</ref><ref>{{cite journal|year=2007|title=Male circumcision: global trends and determinants of prevalence, safety and acceptability|journal=Who/Unaids|url=http://whqlibdoc.who.int/publications/2007/9789241596169_eng.pdf|access-date=2008-10-16|archive-date=2015-07-15|archive-url=https://web.archive.org/web/20150715135808/http://whqlibdoc.who.int/publications/2007/9789241596169_eng.pdf|url-status=live}}</ref> Studies were conducted to assess the acceptability of promoting circumcision; in 2007, country consultations and planning to scale up male circumcision programmes took place in ], ], ], ], ], ], ], ], ], ], ], ] and ].<ref>{{cite journal | year = 2008 | title = Towards Universal access: Scaling up priority HIV/AIDS interventions in the health sector | journal = Who/Unaids/Unicef | pages = 75 | url = http://www.unicef.org/aids/files/towards_universal_access_report_2008.pdf | access-date = 2008-10-16 | archive-date = 2008-10-18 | archive-url = https://web.archive.org/web/20081018050047/http://www.unicef.org/aids/files/towards_universal_access_report_2008.pdf | url-status = live }}</ref> | |||
| In 2011, a ] of observational studies found that circumcision may provide some protection for men during insertive anal sex with men, but noted that there have been no randomized controlled trials examining men who have sex with men and circumcision and that the evidence is not as strong as for heterosexual intercourse.<ref>{{cite journal |last1=Wiysonge |first1=Charles Shey |last2=Kongnyuy |first2=Eugene J |last3=Shey |first3=Muki |last4=Muula |first4=Adamson S |last5=Navti |first5=Osric B |last6=Akl |first6=Elie A |last7=Lo |first7=Ying-Ru |title=Male circumcision for prevention of homosexual acquisition of HIV in men |journal=Cochrane Database of Systematic Reviews |date=15 June 2011 |issue=6 |pages=CD007496 |doi=10.1002/14651858.CD007496.pub2|pmid=21678366 }}</ref> | |||
| == Society and culture == | |||
| The prevalence of circumcision varies across Africa.<ref>{{cite journal | vauthors = Marck J | title = Aspects of male circumcision in sub-equatorial African culture history | journal = Health Transition Review | volume = 7 Suppl | issue = Suppl | pages = 337–60 | year = 1997 | pmid = 10173099 | url = http://htc.anu.edu.au/pdfs/Marck1.pdf | access-date = 2009-03-23 | url-status = dead | type = Review | archive-url = https://web.archive.org/web/20080906115430/http://htc.anu.edu.au/pdfs/Marck1.pdf | archive-date = 2008-09-06 }}</ref><ref>{{cite journal|year=2007|title=Male circumcision: global trends and determinants of prevalence, safety and acceptability|journal=Who/Unaids|url= http://whqlibdoc.who.int/publications/2007/9789241596169_eng.pdf|access-date=2008-10-16}}</ref> Studies were conducted to assess the acceptability of promoting circumcision; in 2007, country consultations and planning to scale up male circumcision programmes took place in ], ], ], ], ], ], ], ], ], ], ], ] and ].<ref>{{cite journal | year = 2008 | title = Towards Universal access: Scaling up priority HIV/AIDS interventions in the health sector | journal = Who/Unaids/Unicef | pages = 75 | url = http://www.unicef.org/aids/files/towards_universal_access_report_2008.pdf | access-date = 2008-10-16 }}</ref> | |||
| ===Programs=== | ===Programs=== | ||
| In 2011, UNAIDS prioritized |
In 2011, UNAIDS prioritized 15 high HIV prevalence countries in eastern and southern Africa, with a goal of circumcising 80% of men (20.8 million) by the end of 2016.<ref name="UNAIDS"> {{Webarchive|url=https://web.archive.org/web/20170729033902/http://www.unaids.org/sites/default/files/media_asset/JC2686_WAD2014report_en.pdf |date=2017-07-29 }} WHO. 2014.</ref> As of 2020, WHO estimated that 250,000 HIV infections have been averted by the 23 million circumcisions conducted in the 15 priority countries of eastern and southern Africa.<ref name=WHO-PrevHIV /> | ||
| UNAIDS' Fast-Track Plan for ending the ] Epidemic by 2030 calls for an additional 25 million circumcisions in these high-priority countries by 2020, which will require to 5 million procedures per year, nearly double the current rate.<ref name="ref12">{{cite web|date=2016|title=Voluntary medical male circumcision: a core campaign to reach the Fast-Track Targets|url=http://www.unaids.org/en/resources/presscentre/featurestories/2016/october/20161017_VMMC|publisher=UNAIDS}}</ref> To reach this goal, UNAIDS is counting on advances in circumcision techniques.<ref name="Framework" /> | |||
| == See also == | == See also == | ||
| Line 130: | Line 60: | ||
| == References == | == References == | ||
| {{reflist|30em}} | {{reflist|30em}} | ||
| == Further reading == | |||
| {{update section|date=August 2020}} | |||
| {{refbegin|30em}} | |||
| * {{cite journal | vauthors = Chang LW, Serwadda D, Quinn TC, Wawer MJ, Gray RH, Reynolds SJ | title = Combination implementation for HIV prevention: moving from clinical trial evidence to population-level effects | journal = The Lancet. Infectious Diseases | volume = 13 | issue = 1 | pages = 65–76 | date = January 2013 | pmid = 23257232 | pmc = 3792852 | doi = 10.1016/S1473-3099(12)70273-6 | type = Review }} | |||
| * {{cite journal | vauthors = Darby R, Van Howe R | title = Not a surgical vaccine: there is no case for boosting infant male circumcision to combat heterosexual transmission of HIV in Australia | journal = Australian and New Zealand Journal of Public Health | volume = 35 | issue = 5 | pages = 459–65 | date = October 2011 | pmid = 21973253 | doi = 10.1111/j.1753-6405.2011.00761.x | s2cid = 24665227 | type = Review | doi-access = free }} | |||
| * {{cite journal | vauthors = Morris BJ, Bailey RC, Klausner JD, Leibowitz A, Wamai RG, Waskett JH, Banerjee J, Halperin DT, Zoloth L, Weiss HA, Hankins CA | display-authors = 6 | title = Review: a critical evaluation of arguments opposing male circumcision for HIV prevention in developed countries | journal = AIDS Care | volume = 24 | issue = 12 | pages = 1565–75 | year = 2012 | pmid = 22452415 | pmc = 3663581 | doi = 10.1080/09540121.2012.661836 | type = Review }} | |||
| * {{cite journal | vauthors = Reed JB, Njeuhmeli E, Thomas AG, Bacon MC, Bailey R, Cherutich P, Curran K, Dickson K, Farley T, Hankins C, Hatzold K, Justman J, Mwandi Z, Nkinsi L, Ridzon R, Ryan C, Bock N | display-authors = 6 | title = Voluntary medical male circumcision: an HIV prevention priority for PEPFAR | journal = Journal of Acquired Immune Deficiency Syndromes | volume = 60 Suppl 3 | issue = Suppl 3 | pages = S88-95 | date = August 2012 | pmid = 22797745 | pmc = 3663585 | doi = 10.1097/QAI.0b013e31825cac4e | type = Review }} | |||
| * {{cite journal | vauthors = Ryan CA, Conly SR, Stanton DL, Hasen NS | s2cid = 33440082 | title = Prevention of sexually transmitted HIV infections through the President's Emergency Plan for AIDS Relief: a history of achievements and lessons learned | journal = Journal of Acquired Immune Deficiency Syndromes | volume = 60 Suppl 3 | issue = Suppl 3 | pages = S70-7 | date = August 2012 | pmid = 22797743 | doi = 10.1097/QAI.0b013e31825e3149 | type = Review }} | |||
| * {{cite journal | vauthors = Uthman OA, Popoola TA, Uthman MM, Aremu O | title = Economic evaluations of adult male circumcision for prevention of heterosexual acquisition of HIV in men in sub-Saharan Africa: a systematic review | journal = PLOS ONE | volume = 5 | issue = 3 | pages = e9628 | date = March 2010 | pmid = 20224784 | pmc = 2835757 | doi = 10.1371/journal.pone.0009628 | veditors = Van Baal PH | type = Review | bibcode = 2010PLoSO...5.9628U }} | |||
| * World Health Organization | |||
| ** {{cite web |url=http://whqlibdoc.who.int/publications/2011/9789241501651_eng.pdf|title=Global health sector strategy on HIV/AIDS 2011-2015|publisher=World Health Organization|date=2011|access-date=January 11, 2014}} | |||
| ** {{cite web |url=https://www.who.int/hiv/topics/malecircumcision/fact_sheet/en/index.html|title=Voluntary medical male circumcision for HIV prevention|publisher=World Health Organization|date=July 2012|access-date=January 11, 2014}} | |||
| ** {{cite web |url=https://www.who.int/hiv/pub/malecircumcision/devices_guidelines/en/index.html|title=Guideline on the use of devices for adult male circumcision for HIV prevention|publisher=World Health Organization|date=October 2013|access-date=January 11, 2014}} | |||
| {{refend}} | |||
| == External links == | |||
| * {{cite web |url=https://www.who.int/hiv/topics/malecircumcision/en/ |publisher= World Health Organization |title= Male circumcision for HIV prevention |access-date= January 11, 2014}} | |||
| {{Circumcision series}} | {{Circumcision series}} | ||
Latest revision as of 01:19, 6 June 2024
Overview of relationship between male circumcision and HIV This article is about male circumcision and HIV. For female circumcision and HIV, see Female genital mutilation § HIV.Male circumcision reduces the risk of human immunodeficiency virus (HIV) transmission from HIV positive women to men in high risk populations.
In 2020, the World Health Organization (WHO) reiterated that male circumcision is an efficacious intervention for HIV prevention if carried out by medical professionals under safe conditions. Circumcision reduces the risk that a man will acquire HIV and other sexually transmitted infections (STIs) from an infected female partner through vaginal sex. The evidence regarding whether circumcision helps prevent HIV is not as clear among men who have sex with men (MSM). The effectiveness of using circumcision to prevent HIV in the developed world is not determined.
Efficacy
Heterosexual men
As of 2020, past research has shown that circumcision reduces the risk of HIV infection in heterosexual men, although these studies have had limitations.
The WHO Expert Group on Models To Inform Fast Tracking Voluntary Medical Male Circumcision In HIV Combination Prevention in 2016 found "large benefits" of circumcision in settings with high HIV prevalence and low circumcision prevalence. The Group estimated male circumcision is cost-saving in almost all high priority countries. Furthermore, WHO stated that: "While circumcision reduces a man’s individual lifetime HIV risk, the indirect effect of preventing further HIV transmissions to women, their babies (vertical transmission) and from women to other men has an even greater impact on the population incidence, particularly for circumcisions performed at younger ages (under age 25 years)."
Newly circumcised HIV infected men who are not taking antiretroviral therapy can shed the HIV virus from the circumcision wound, thus increasing the immediate risk of HIV transmission to female partners. This risk of post-operative transmission presents a challenge, although in the long-term it is possible the circumcision of HIV-infected men helps lessen heterosexual HIV transmission overall. Such viral shedding can be mitigated by the use of antiretroviral drugs. Additional research is needed to ascertain the existence and potential risk of viral shedding from circumcision wounds.
Men who have sex with men
The WHO does not recommend circumcision as protection against male to male HIV transmission, as evidence is lacking in regards to receptive anal intercourse. The WHO also states that MSM should not be excluded from circumcision services in countries in eastern and southern Africa, and that circumcision may be effective at limiting the spread of HIV for MSM if they also engage in vaginal sex with women.
Regional differences
Whether circumcision is beneficial to developed countries for HIV prevention purposes is undetermined. It is not known whether the effect of male circumcision differs by HIV-1 variant. The predominant subtype of HIV-1 in the United States is subtype B, and in Africa, the predominant subtypes are A, C, and D.
Recommendations
The most recent WHO review of the evidence reiterates prior estimates of the impact of male circumcision on HIV incidence rates. In 2020, WHO again concluded that male circumcision is an efficacious intervention for HIV prevention and that the promotion of male circumcision is an essential strategy, in addition to other preventive measures, for the prevention of heterosexually acquired HIV infection in men. Eastern and southern Africa had a particularly low prevalence of circumcised males. This region has a disproportionately high HIV infection rate, with a significant number of those infections stemming from heterosexual transmission. The WHO has made voluntary medical male circumcision (VMMC) a priority intervention in that region since their 2007 recommendations.
Although these results confirm that male circumcision reduces the risk of men becoming infected with HIV, the UN agencies emphasize that it does not provide complete protection against HIV infection. Circumcised men can still become infected with the virus and, if HIV-positive, can infect their sexual partners. Male circumcision should never replace other known effective prevention methods and should always be considered as part of a comprehensive prevention package, which includes correct and consistent use of male or female condoms, reduction in the number of sexual partners, delaying the onset of sexual relations, and HIV testing, counseling, and treatment.
— World Health Organization, Joint WHO/UNAIDS Statement made in 2007.
In the United States, the American Academy of Pediatrics (AAP) led a 2012 task force which included the American Academy of Family Physicians (AAFP), the American College of Obstetricians and Gynecologists (ACOG), and the Centers for Disease Control (CDC). The task force concluded that circumcision may be helpful for the prevention of HIV in the United States. The CDC 2018 position on circumcision and HIV recommended that circumcision should continue to be offered to parents who are informed of the benefits and risks, including a potential reduction in risk of HIV transmission. The position asserts that circumcision conducted after sexual debut can result in missed opportunities for HIV prevention.
Because the evidence that circumcision prevents HIV mainly comes from studies conducted in Africa, the Royal Dutch Medical Association (KNMG) questioned the applicability of those studies to developed countries. Circumcision has not been included in their HIV prevention recommendations. The KNMG circumcision policy statement was endorsed by several Dutch medical associations. The policy statement was initially released in 2010, but was reviewed again and accepted in 2022.
Mechanism of action
While the biological mechanism of action is not known, a 2020 meta-analysis stated "the consistent protective effect suggests that the reasons for the heterogeneity lie in concomitant individual social and medical factors, such as presence of STIs, rather than a different biological impact of circumcision." The inner foreskin harbours an increased density of CD4 T-cells and releases increased levels of pro-inflammatory cytokines. Hence the sub-preputial space displays a pro-inflammatory environment, conducive to HIV infection.
Langerhans cells (part of the human immune system) under the foreskin may be a source of entry for HIV. Excising the foreskin removes what is thought to be a main entry point for the HIV virus.
History
Valiere Alcena, in a 1986 letter to the New York State Journal of Medicine, noted that low rates of circumcision in parts of Africa had been linked to the high rate of HIV infection. Aaron J. Fink several months later also proposed that circumcision could have a preventive role when the New England Journal of Medicine published his letter, "A possible explanation for heterosexual male infection with AIDS," in October, 1986. By 2000, over 40 epidemiological studies had been conducted to investigate the relationship between circumcision and HIV infection. A meta-analysis conducted by researchers at the London School of Hygiene & Tropical Medicine examined 27 studies of circumcision and HIV in sub-Saharan Africa and concluded that these showed circumcision to be "associated with a significantly reduced risk of HIV infection" that could form part of a useful public health strategy. A 2005 review of 37 observational studies expressed reservations about the conclusion because of possible confounding factors, since all studies to date had been observational as opposed to randomized controlled trials. The authors stated that three randomized controlled trials then underway in Africa would provide "essential evidence" about the effects of circumcision on preventing HIV.
Experimental evidence was needed to establish a causal relationship, so three randomized controlled trials (RCT) were commissioned as a means to reduce the effect of any confounding factors. Trials took place in South Africa, Kenya and Uganda. All three trials were stopped early by their monitoring boards because those in the circumcised group had a substantially lower rate of HIV incidence than the control group, and hence it was seen as unethical to withhold the procedure, in light of strong evidence of efficacy. In 2009, a Cochrane review which included the results of the three randomized controlled trials found "strong" evidence that the acquisition of HIV by a man during sex with a woman was decreased by 54% (95% confidence interval, 38% to 66%) over 24 months if the man was circumcised. The review also found a low incidence of adverse effects from circumcision in the trials reviewed. WHO assessed the trials as "gold standard" studies and found "strong and consistent" evidence from later studies that confirmed the results. In 2020, a review including post-study follow up from the three randomized controlled trials, as well as newer observational studies, found a 59% relative reduction in HIV incidence, and 1.31% absolute decrease across the three randomized controlled trials, as well as continued protection for up to 6 years after the studies began.
Society and culture

The WHO recommends VMMC, as opposed to traditional circumcision. There is some evidence that traditionally circumcised men (i.e. who have been circumcised by a person who is not medically trained) use condoms less often and have higher numbers of sexual partners, increasing their risk of contracting HIV. Newly circumcised men must refrain from sexual activity until the wounds are fully healed.
The prevalence of circumcision varies across Africa. Studies were conducted to assess the acceptability of promoting circumcision; in 2007, country consultations and planning to scale up male circumcision programmes took place in Botswana, Eswatini, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Uganda, Tanzania, Zambia and Zimbabwe.
Programs
In 2011, UNAIDS prioritized 15 high HIV prevalence countries in eastern and southern Africa, with a goal of circumcising 80% of men (20.8 million) by the end of 2016. As of 2020, WHO estimated that 250,000 HIV infections have been averted by the 23 million circumcisions conducted in the 15 priority countries of eastern and southern Africa.
See also
References
- Sharma, Adhikarimayum Lakhikumar; Hokello, Joseph; Tyagi, Mudit (2021-06-25). "Circumcision as an Intervening Strategy against HIV Acquisition in the Male Genital Tract". Pathogens. 10 (7): 806. doi:10.3390/pathogens10070806. ISSN 2076-0817. PMC 8308621. PMID 34201976.
There is disputed immunological evidence in support of MC in preventing the heterosexual acquisition of HIV-1.
- Merson, Michael; Inrig, Stephen (2017). The AIDS Pandemic: Searching for a Global Response. Springer Publishing. p. 379. ISBN 9783319471334.
This led to a consensus that male circumcision should be a priority for HIV prevention in countries and regions with heterosexual epidemics and high HIV and low male circumcision prevalence.
- ^ "Preventing HIV Through Safe Voluntary Medical Male Circumcision For Adolescent Boys And Men In Generalized HIV Epidemics". World Health Organization. 2020. Retrieved 2021-05-24.
- ^ Information for providers counseling male patients and parents regarding male circumcision and the prevention of HIV infection, STIs, and other health outcomes (Report). Centers for Disease Control and Prevention. August 22, 2018. Archived from the original on 2021-05-06. Retrieved 2021-05-26.
- ^ Kim HH, Li PS, Goldstein M (November 2010). "Male circumcision: Africa and beyond?". Curr Opin Urol. 20 (6): 515–9. doi:10.1097/MOU.0b013e32833f1b21. PMID 20844437. S2CID 2158164.
- ^ Farley TM, Samuelson J, Grabowski MK, Ameyan W, Gray RH, Baggaley R (June 2020). "Impact of male circumcision on risk of HIV infection in men in a changing epidemic context - systematic review and meta-analysis". J Int AIDS Soc (Review). 23 (6): e25490. doi:10.1002/jia2.25490. PMC 7303540. PMID 32558344.
- "Models To Inform Fast Tracking Voluntary Medical Male Circumcision In HIV Combination Prevention" (PDF). World Health Organization. March 2016. Archived (PDF) from the original on 2020-09-23. Retrieved 2021-05-26.
- Tobian AA, Adamu T, Reed JB, Kiggundu V, Yazdi Y, Njeuhmeli E (December 2015). "Voluntary medical male circumcision in resource-constrained settings". Nat Rev Urol (Review). 12 (12): 661–70. doi:10.1038/nrurol.2015.253. PMID 26526758. S2CID 10432723.
- Olapade-Olaopa, Emiola Oluwabunmi; Salami, Mudasiru Adebayo; Lawal, Taiwo Akeem (2019). "Male circumcision and global HIV/AIDS epidemic challenges". African Journal of Urology. 25. doi:10.1186/s12301-019-0005-2. S2CID 208085886.
- "WHO and UNAIDS Secretariat welcome corroborating findings of trials assessing impact of male circumcision on HIV risk" (Press release). World Health Organization. February 23, 2007. Archived from the original on 2007-02-26. Retrieved 2007-02-23.
- American Academy of Pediatrics Task Force on Circumcision (2012). "Technical Report". Pediatrics. 130 (3): e756–e785. doi:10.1542/peds.2012-1990. ISSN 0031-4005. PMID 22926175. Archived from the original on 2012-09-20.
- "Non-therapeutic circumcision of male minors KNMG viewpoint". 31 March 2022.
- Prodger, Jessica L. (September 2017). "The biology of how circumcision reduces HIV susceptibility: broader implications for the prevention field". AIDS Research and Therapy. 14 (1): 49. doi:10.1186/s12981-017-0167-6. PMC 5594533. PMID 28893286.
- Weiss HA, Dickson KE, Agot K, Hankins CA (October 2010). "Male circumcision for HIV prevention: current research and programmatic issues". AIDS (Randomized controlled trial). 24 (Suppl 4): S61-9. doi:10.1097/01.aids.0000390708.66136.f4. PMC 4233247. PMID 21042054.
- Szabo R, Short RV (June 2000). "How does male circumcision protect against HIV infection?". BMJ (Review). 320 (7249): 1592–4. doi:10.1136/bmj.320.7249.1592. PMC 1127372. PMID 10845974.
- Alcena V (19 October 2006). "AIDS in Third World countries". PLOS Medicine (Comment). 86 (8): 446. PMID 3463895. Archived from the original on 10 January 2014. Retrieved 10 January 2014.
- Alcena V (August 1986). "AIDS in Third World countries". New York State Journal of Medicine (Letter). 86 (8): 446. PMID 3463895. Archived from the original on 2014-01-10. Retrieved 2014-01-10.
- Fink AJ (October 1986). "A possible explanation for heterosexual male infection with AIDS". The New England Journal of Medicine (Letter). 315 (18): 1167. doi:10.1056/nejm198610303151818. PMID 3762636.
- Szabo R, Short RV (June 2000). "How does male circumcision protect against HIV infection?". BMJ (Review). 320 (7249): 1592–4. doi:10.1136/bmj.320.7249.1592. PMC 1127372. PMID 10845974.
- Weiss HA, Quigley MA, Hayes RJ (October 2000). "Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis". AIDS (Meta-analysis). 14 (15): 2361–70. doi:10.1097/00002030-200010200-00018. PMID 11089625. S2CID 21857086. Archived from the original (PDF) on 2014-01-10.
- Siegfried N, Muller M, Deeks J, Volmink J, Egger M, Low N, et al. (March 2005). "HIV and male circumcision--a systematic review with assessment of the quality of studies". The Lancet. Infectious Diseases (Review). 5 (3): 165–73. doi:10.1016/S1473-3099(05)01309-5. PMID 15766651.
- ^ Siegfried N, Muller M, Deeks JJ, Volmink J (April 2009). Siegfried N (ed.). "Male circumcision for prevention of heterosexual acquisition of HIV in men". The Cochrane Database of Systematic Reviews (2): CD003362. doi:10.1002/14651858.CD003362.pub2. PMID 19370585.
- Siegfried, Nandi; Muller, Martie; Deeks, Jonathan J; Volmink, Jimmy (15 April 2009). "Male circumcision for prevention of heterosexual acquisition of HIV in men". Cochrane Database of Systematic Reviews (2): CD003362. doi:10.1002/14651858.CD003362.pub2. PMID 19370585.
- Farley, Timothy MM; Samuelson, Julia; Grabowski, M Kate; Ameyan, Wole; Gray, Ronald H; Baggaley, Rachel (June 2020). "Impact of male circumcision on risk of HIV infection in men in a changing epidemic context – systematic review and meta-analysis". Journal of the International AIDS Society. 23 (6): e25490. doi:10.1002/jia2.25490. PMC 7303540. PMID 32558344.
- Seeth, Avantika (June 1, 2018). "'It's hassle-free,' says actor Melusi Yeni about his medical circumcision". News24. Retrieved September 6, 2022.
Actor Melusi Yeni was the millionth man to undergo voluntary male medical circumcision at the Sivananda Clinic in KwaZulu-Natal.
- Marck J (1997). "Aspects of male circumcision in sub-equatorial African culture history" (PDF). Health Transition Review (Review). 7 Suppl (Suppl): 337–60. PMID 10173099. Archived from the original (PDF) on 2008-09-06. Retrieved 2009-03-23.
- "Male circumcision: global trends and determinants of prevalence, safety and acceptability" (PDF). Who/Unaids. 2007. Archived (PDF) from the original on 2015-07-15. Retrieved 2008-10-16.
- "Towards Universal access: Scaling up priority HIV/AIDS interventions in the health sector" (PDF). Who/Unaids/Unicef: 75. 2008. Archived (PDF) from the original on 2008-10-18. Retrieved 2008-10-16.
- Joint strategic action framework to accelerate the scale-up of voluntary medical male circumcision for HIV prevention in Eastern and Southern Africa, 2012-2016. Archived 2017-07-29 at the Wayback Machine WHO. 2014.
| Circumcision | |
|---|---|
| Medical aspects | |
| History and prevalence | |
| Religious aspects | |
| Ethical and legal aspects | |
| Category | |
