| Revision as of 19:11, 6 February 2009 editDrbreznjev (talk | contribs)16,660 edits Undid revision 268901316 by 213.98.182.39 (talk)← Previous edit | Latest revision as of 18:53, 20 October 2024 edit undo2601:642:c303:f370:4df:e9a5:420a:1f96 (talk) Reclassified to Clostridioides in 2016. CE | ||
| (204 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{cs1 config|name-list-style=vanc}} | |||
| {{mergefrom|Walking pneumonia|Talk:Walking pneumonia#Merger proposal|date=October 2007}} | |||
| {{Infobox medical condition (new) | |||
| | name = <!--{{PAGENAME}} by default--> | |||
| | synonym = CAP | |||
| | image = | |||
| | image_size = | |||
| | alt = | |||
| | caption = | |||
| | pronounce = | |||
| | specialty = <!-- from Wikidata, can be overwritten --> | |||
| | symptoms = | |||
| | complications = | |||
| | onset = | |||
| | duration = | |||
| | types = | |||
| | causes = | |||
| | risks = | |||
| | diagnosis = | |||
| | differential = | |||
| | prevention = | |||
| | treatment = | |||
| | medication = | |||
| | prognosis = | |||
| | frequency = | |||
| | deaths = | |||
| }} | |||
| '''Community-acquired pneumonia''' (CAP) refers to ] (any of several lung diseases) contracted by a person outside of the healthcare system. In contrast, ] (HAP) is seen in patients who have recently visited a hospital or who live in long-term care facilities. CAP is common, affecting people of all ages, and its symptoms occur as a result of oxygen-absorbing areas of the lung (]) filling with fluid. This inhibits lung function, causing ], ], ]s and ]. | |||
| CAP, the most common type of pneumonia, is a leading ] worldwide{{Citation needed|date=May 2020}}. Its causes include ], ]es, ] and ].<ref>{{Cite web|title = Pneumonia Causes – Mayo Clinic|url = http://www.mayoclinic.org/diseases-conditions/pneumonia/basics/causes/con-20020032|website = www.mayoclinic.org|access-date = 2015-05-18}}</ref> CAP is diagnosed by assessing symptoms, performing a physical examination, by ] or by ] examination. Patients with CAP sometimes require hospitalization, and it is treated primarily with ], ]s and ].<ref>{{Cite web|title = Pneumonia Treatments and drugs – Mayo Clinic|url = http://www.mayoclinic.org/diseases-conditions/pneumonia/basics/treatment/con-20020032|website = www.mayoclinic.org|access-date = 2015-05-18}}</ref> Some forms of CAP can be prevented by ]<ref>{{Cite journal |doi = 10.1097/MCP.0000000000000369|pmid = 28198725|title = Adult pneumococcal vaccination|journal = Current Opinion in Pulmonary Medicine|volume = 23|issue = 3|pages = 225–230|year = 2017|last1 = José|first1 = Ricardo J.|last2 = Brown|first2 = Jeremy S.| s2cid=4700975 }}</ref> and by abstaining from tobacco products.<ref>{{Cite web|title = Pneumonia Prevention – Mayo Clinic|url = http://www.mayoclinic.org/diseases-conditions/pneumonia/basics/prevention/con-20020032|website = www.mayoclinic.org|access-date = 2015-05-18}}</ref> | |||
| {{pneumonia}} | |||
| '''Community-acquired pneumonia''' ('''CAP''') is a ] in which individuals who have not recently been ]ized develop an ] of the ]s (]). CAP is a common illness and can affect people of all ages. CAP often causes problems like ]ing, ], ]s, and a ]. CAP occurs because the areas of the lung which absorb ] (]) from the ] become filled with fluid and cannot work effectively. | |||
| == Signs and symptoms == | |||
| CAP occurs throughout the world and is a leading cause of illness and death. Causes of CAP include ], ], ], and ]. CAP can be ] by ]s and ] alone, though ]s, examination of the ], and other tests are often used. Individuals with CAP sometimes require ] in a ]. CAP is primarily treated with ] ]. Some forms of CAP can be ] by ].{{ref|Sharma}} | |||
| ==Symptoms== | ==={{anchor|Symptoms of CAP}}Common symptoms=== | ||
| ] | |||
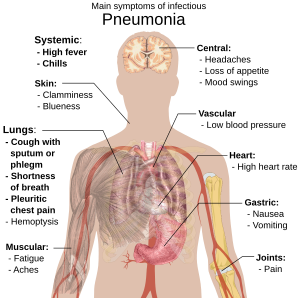
| Symptoms of CAP commonly include: | |||
| * Coughing which produces greenish or yellow sputum | |||
| *] | |||
| * A high fever, accompanied by sweating, chills and shivering | |||
| *coughing that produces greenish or yellow ] | |||
| * Sharp, stabbing chest pains | |||
| *a high ] that may be accompanied with sweating, chills, and ] | |||
| * Rapid, shallow, often painful breathing | |||
| *sharp or stabbing chest pain | |||
| *rapid, shallow breathing that is often painful | |||
| Less common symptoms |
==={{anchor|Less common symptoms}}Less-common symptoms=== | ||
| * |
* Coughing up blood (]) | ||
| * Headaches, including migraines | |||
| *]s (including migraine headaches) | |||
| *] | * ] | ||
| * |
* Excessive fatigue | ||
| * |
* Bluish skin (]) | ||
| *] | * ] | ||
| *] | * ] | ||
| *] | * ] | ||
| * |
* Joint pain (]) | ||
| * |
* Muscle aches (]) | ||
| * Rapid heartbeat | |||
| * Dizziness or lightheadedness | |||
| ==={{anchor|Symptoms in older people}}In the elderly=== | |||
| The manifestations of pneumonia, like those for many conditions, might not be typical in older people. They might instead experience: | |||
| * |
* New or worsening confusion | ||
| *] | * ] | ||
| * Poor coordination, which may lead to falls | |||
| *falls* | |||
| ==={{anchor|Symptoms for infants}}In infants=== | |||
| * Unusual sleepiness | |||
| *being overly sleepy | |||
| * |
* Yellowing of the skin (]) | ||
| * |
* Difficulty feeding<ref name=Metaly /> | ||
| === {{anchor|Sepsis|Respiratory failure|Pleural effusion and empyema|Abscess}}Complications === | |||
| Major complications of CAP include: | |||
| * ] - A life-threatening reaction to infection. A common cause of sepsis is ], frequently the result of infection with ''streptococcus pneumoniae''. Patients with sepsis require intensive care with blood pressure monitoring and support against hypotension. Sepsis can cause liver, kidney and heart damage. | |||
| * Respiratory failure - CAP patients often have ], which may require support. Non-invasive machines (such as ]), a ] or a ] may be used. | |||
| * Pleural effusion and empyema - Microorganisms from the lung may trigger fluid collection in the ], or ]. Pleural fluid, if present, should be ] and examined. Depending on the results, complete drainage of the fluid with a ] may be necessary to prevent proliferation of the infection. Antibiotics, which do not penetrate the pleural cavity well, are less effective. | |||
| * ] - A pocket of fluid and bacteria may appear on X-ray as a cavity in the lung. Abscesses, typical of ], usually contain a mixture of ]. Although antibiotics can usually cure abscesses, sometimes they require drainage by a surgeon or ]. | |||
| == {{anchor|Cause}}Causes == | |||
| ==Diagnosis== | |||
| Many different microorganisms can cause CAP. However, the most common cause is '']''. Certain groups of people are more susceptible to CAP-causing pathogens - ]s, adults with ]s (such as ]), and senior citizens. ] and others with compromised immune systems are more likely to develop CAP from '']'' or '']''.<ref>{{Cite web|title = What is pneumonia? What causes pneumonia?|url = http://www.medicalnewstoday.com/articles/151632.php|access-date = 2015-05-18}}</ref> A definitive cause is identified in only half the cases.{{cn|date=March 2022}} | |||
| Individuals with symptoms of CAP require further evaluation. ] by a health provider may reveal fever, an increased ] (]), low ] (]), a fast ] (]), and/or changes in the amount of oxygen in the ]. Feeling the way the chest expands (]) and tapping the chest wall (]) to identify dull areas which do not ] can identify areas of the lung which are stiff and full of fluid (consolidated). Examination of the lungs with the aid of a ] can reveal several things. A lack of normal breath sounds or the presence of crackling sounds (]) when the lungs are listened to (]) can also indicate consolidation. Increased vibration of the chest when speaking (tactile fremitus) and increased volume of whispered speech during ] of the chest can also reveal consolidation.{{ref|Metlay}} | |||
| ] | |||
| ]s of the chest, examination of the ] and ] for infectious ], and ] are commonly used to diagnose individuals with suspected CAP based upon symptoms and physical examination. The use of each test depends on the severity of illness, local practices, and the concern for any ]s resulting from the infection. | |||
| === Neonates and infants === | |||
| All patients with CAP should have the amount of oxygen in their blood monitored with a machine called a ]. This helps determine how well the lungs are able to work despite infection. In some cases, analysis of ] may be required to accurately determine the amount of oxygen in the blood. ] (CBC), a blood test, may reveal extra ]s, indicating an infection. Chest x-rays and chest ] (CT) can reveal areas of ] (seen as white) which represent consolidation. A normal chest x-ray makes CAP less likely; however, CAP is sometimes not seen on x-rays because the disease is either in its initial stages or involves a part of the lung not easily seen by x-ray. In some cases, chest CT can reveal a CAP which is not present on chest x-ray. X-rays can often be misleading, as many other diseases can mimic CAP such as ] or other types of lung damage.{{ref|Syrjala}} | |||
| It is possible for a fetus to develop a lung infection before birth by aspirating infected ] or through a blood-borne infection which crossed the ]. Infants can also inhale contaminated fluid from the vagina at birth. The most prevalent pathogen causing CAP in newborns is '']'', also known as group-B streptococcus (GBS). GBS causes more than half of CAP in the first week after birth.<ref name=Webber /> Other bacterial causes of neonatal CAP include '']'' and a variety of ]. CAP-causing viruses may also be transferred from mother to child; ], the most common, is life-threatening, and ], ] and ] can also cause pneumonia. Another cause of neonatal CAP is '']'', which, though acquired at birth, does not cause pneumonia until two to four weeks later. It usually presents with no fever and a characteristic, staccato cough. | |||
| CAP in older infants reflects increased exposure to microorganisms, with common bacterial causes including ''Streptococcus pneumoniae'', '']'', '']'', '']'' and '']''. Maternally-derived ] is also a cause of CAP in infants. Viral causes include ] (RSV), ], adenovirus, ], ] and ], and RSV is a common source of illness and hospitalization in infants.<ref name=Abzug /> CAP caused by fungi or parasites is not usually seen in otherwise-healthy infants. | |||
| Several tests can be performed to identify the cause of an individual's CAP. ]s can be drawn to isolate any bacteria or fungi in the blood stream. Sputum ] and culture can also reveal the causative microorganism. In more severe cases, a procedure wherein a flexible scope is passed through the mouth into the lungs (]) can be used collect fluid for culture. Special tests can be performed if an uncommon microorganism is suspected (such as testing the urine for ] ] when ] is a concern). | |||
| == |
=== Children === | ||
| Although children older than one month tend to be at risk for the same microorganisms as adults, children under five years of age are much less likely to have pneumonia caused by '']'', '']'' or '']'' than older children. In contrast, older children and teenagers are more likely to acquire ''Mycoplasma pneumoniae'' and ''Chlamydophila pneumoniae'' than adults.<ref name=Wubbel /> | |||
| The symptoms of CAP are the result of both the invasion of the lungs by ]s and the ]'s response to the infection. The mechanisms of infection are quite different for ]es and the other microorganisms. | |||
| === Adults === | |||
| *''Viruses'' | |||
| A full spectrum of microorganisms is responsible for CAP in adults, and patients with certain ]s are more susceptible to infections by certain groups of microorganisms. Identifying people at risk for infection by these organisms aids in appropriate treatment. | |||
| :Viruses must invade cells in order to reproduce. Typically, a virus will reach the lungs by traveling in droplets through the ] and ] with ]. There, the virus invades the cells lining the airways and the alveoli. This invasion often leads to cell death either through direct killing by the virus or by self-destruction through ]. Further damage to the lungs occurs when the immune system responds to the infection. ]s, in particular ]s, are responsible for activating a variety of chemicals (]s) which cause leaking of fluid into the alveoli. The combination of cellular destruction and fluid-filled alveoli interrupts the transportation of oxygen into the bloodstream. In addition to the effects on the lungs, many viruses affect other ]s and can lead to illness affecting many different bodily functions. Viruses also make the body more susceptible to bacterial infection; for this reason, bacterial pneumonia often complicates viral CAP. | |||
| Many less-common organisms can cause CAP in adults; these may be determined by identifying specific risk factors, or when treatment for more common causes fails. | |||
| === Risk factors === | |||
| *''Bacteria and fungi'' | |||
| Some patients have an underlying problem which increases their risk of infection. Some risk factors are: | |||
| :Bacteria and fungi also typically enter the lung with inhalation, though they can reach the lung through the bloodstream if other parts of the body are infected. Often, bacteria live in parts of the ] and are constantly being inhaled into the alveoli. Once inside the alveoli, ] and ] travel into the spaces between the cells and also between adjacent alveoli through connecting pores. This invasion triggers the ] to respond by sending white blood cells responsible for attacking microorganisms (]s) to the lungs. The neutrophils ] and kill the offending organisms but also release cytokines which result in a general activation of the immune system. This results in the fever, chills, and fatigue common in CAP. The neutrophils, bacteria, and fluid leaked from surrounding blood vessels fill the alveoli and result in impaired oxygen transportation. Bacteria often travel from the lung into the blood stream and can result in serious illness such as ], in which there is low blood pressure leading to damage in multiple parts of the body including the ], ], and ]. | |||
| * ''Obstruction'' - When part of the airway (]) leading to the alveoli is obstructed, the lung cannot eliminate fluid; this can lead to pneumonia. One cause of obstruction, especially in young children, is inhalation of a foreign object such as a marble or toy. The object lodges in a small airway, and pneumonia develops in the obstructed area of the lung. Another cause of obstruction is ], which can block the flow of air. | |||
| * ''Lung disease'' - Patients with underlying lung disease are more likely to develop pneumonia. Diseases such as emphysema and habits such as smoking result in more frequent and more severe bouts of pneumonia. In children, recurrent pneumonia may indicate ] or ]. | |||
| * ''Immune problems'' - ] patients, such as those with ], are more likely to develop pneumonia. Other immune problems that increase the risk of developing pneumonia range from severe childhood immune deficiencies, such as ], to the less severe ].<ref name=Mundy /> | |||
| == Pathophysiology == | |||
| *''Parasites'' | |||
| The symptoms of CAP are the result of lung infection by microorganisms and the response of the ] to the infection. Mechanisms of infection are different for viruses and other microorganisms.{{cn|date=March 2022}} | |||
| :There are a variety of parasites which can affect the lungs. In general, these parasites enter the body through the skin or by being swallowed. Once inside the body, these parasites travel to the lungs, most often through the blood. There, a similar combination of cellular destruction and immune response causes disruption of oxygen transportation. | |||
| ===Viruses=== | |||
| == Microorganisms causing CAP == | |||
| Up to 20 percent of CAP cases can be attributed to viruses.<ref>{{Cite book|title=Respiratory infections|last=Mandell|first=L|publisher=CRC Press|year=2006|pages=338}}</ref> The most common viral causes are influenza, parainfluenza, human respiratory syncytial virus, human metapneumovirus and adenovirus. Less common viruses which may cause serious illness include ], ], ] and ].<ref name="Roux" /> | |||
| There are over a hundred microorganisms which can cause CAP. The most common types of microorganisms are different among different groups of people. Newborn ]s, ], and ]s are at risk for different spectrums of disease causing microorganisms. In addition, adults with ] illnesses, who live in certain parts of the world, who reside in ]s, who have recently been treated with ]s, or who are ] are at risk for unique infections. Even when aggressive measures are taken, a definite cause for pneumonia is only identified in half the cases. | |||
| Typically, a virus enters the lungs through the inhalation of water droplets and invades the cells lining the airways and the alveoli. This leads to cell death; the cells are killed by the virus or they ]. Further lung damage occurs when the immune system responds to the infection. ]s, particularly ]s, activate chemicals known as ]s which cause fluid to leak into the alveoli. The combination of cell destruction and fluid-filled alveoli interrupts the transportation of oxygen into the bloodstream. In addition to their effects on the lungs, many viruses affect other organs. Viral infections weaken the immune system, making the body more susceptible to bacterial infection, including bacterial pneumonia. | |||
| === ''Infants'' === | |||
| Newborn infants can acquire lung infections prior to being born either by breathing infected ] or by blood-borne infection across the ]. Infants can also inhale (]) fluid from the ] canal as they are being born. The most important infection in newborns is caused by ], also known as Group B Streptococcus or GBS. GBS causes at least 50% of cases of CAP in the first week of life.{{ref|Webber}} Other bacterial causes in the newborn period include '']'' and ]. Viruses can also be transferred from mother to child; ] is the most common and life-threatening, but ], ], and ] can also cause disease. | |||
| ===Bacteria and fungi=== | |||
| CAP in older infants reflects increased exposure to microorganisms. Common bacterial causes include '']'', '']'', '']'', '']'', and '']''. A unique cause of CAP in this group is '']'', which is acquired during birth but which does not cause pneumonia until 2-4 weeks later. Common viruses include ] (RSV), ], ], ], ], and ]. RSV in particular is a common source of illness and hospitalization.{{ref|Abzug}} Fungi and parasites are not typically encountered in otherwise healthy infants, though maternally-derived ] can be a cause of CAP in this age group. | |||
| Although most cases of bacterial pneumonia are caused by ''Streptococcus pneumoniae'', infections by ] such as ''Mycoplasma pneumoniae,'' ''Chlamydophila pneumoniae,'' and ''Legionella pneumophila'' can also cause CAP. Enteric ], such as '']'' and '']'', are a group of bacteria that typically live in the ]; contamination of food and water by these bacteria can result in outbreaks of pneumonia. '']'', an uncommon cause of CAP, is a difficult bacteria to treat. | |||
| Bacteria and fungi typically enter the lungs by inhalation of water droplets, although they can reach the lung through the bloodstream if an infection is present. In the alveoli, bacteria and fungi travel into the spaces between cells and adjacent alveoli through connecting pores. The immune system responds by releasing ]s, white blood cells responsible for attacking microorganisms, into the lungs. The neutrophils ] and kill the microorganisms, releasing cytokines which activate the entire immune system. This response causes fever, chills and fatigue, common symptoms of CAP. The neutrophils, bacteria and fluids leaked from surrounding blood vessels fill the alveoli, impairing oxygen transport. Bacteria may travel from the lung to the bloodstream, causing ] (very low blood pressure which damages the brain, kidney, and heart). | |||
| === ''Children'' === | |||
| For the most part, children older than one month of life are at risk for the same microorganisms as adults. However, children less than five years are much less likely to have pneumonia caused by '']'', '']'', or '']''. In contrast, older children and teenagers are more likely to acquire '']'' and '']'' than adults.{{ref|Wubbel}} | |||
| === |
===Parasites=== | ||
| A variety of parasites can affect the lungs, generally entering the body through the skin or by being swallowed. They then travel to the lungs through the blood, where the combination of cell destruction and immune response disrupts oxygen transport. | |||
| The full spectrum of microorganisms are responsible for CAP in adults. Several important groups of organisms are more common among people with certain ]s. Identifying people at risk for these organisms is important for appropriate treatment. | |||
| == Diagnosis == | |||
| *''Viruses'' | |||
| Patients with symptoms of CAP require evaluation. Diagnosis of pneumonia is made clinically, rather than on the basis of a particular test.<ref name="Mandell">{{cite journal | last1=Mandell | first1=L. A. | last2=Wunderink | first2=R. G. | last3=Anzueto | first3=A. | last4=Bartlett | first4=J. G. | last5=Campbell | first5=G. D. | last6=Dean | first6=N. C. | last7=Dowell | first7=S. F. | last8=File | first8=T. M. | last9=Musher | first9=D. M. | last10=Niederman | first10=M. S. | last11=Torres | first11=A. | last12=Whitney | first12=C. G. | title=Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults | journal=Clinical Infectious Diseases | publisher=Oxford University Press (OUP) | volume=44 | issue=Supplement 2 | date=2007-03-01 | issn=1058-4838 | pmc=7107997| doi=10.1086/511159 | pages=S27–S72 | pmid=17278083| doi-access=free }}</ref> Evaluation begins with a physical examination by a health provider, which may reveal fever, an increased ] (]), low blood pressure (]), a fast heart rate (]) and changes in the amount of oxygen in the blood. ] the chest as it expands and ] the chest wall to identify dull, non-resonant areas can identify stiffness and fluid, signs of CAP. Listening to the lungs with a stethoscope (]) can also reveal signs associated with CAP. A lack of normal breath sounds or the presence of ] can indicate fluid consolidation. Increased vibration of the chest when speaking, known as tactile fremitus, and increased volume of whispered speech during auscultation can also indicate the presence of fluid.<ref name=Metlay /> | |||
| :Viruses cause 20% of CAP cases. The most common viruses are ], ], ], ], and ]. Less common viruses causing significant illness include ], ], ], and ].{{ref|Roux}} | |||
| Several tests can identify the cause of CAP. ]s can isolate bacteria or fungi in the bloodstream. Sputum ] and culture can also reveal the causative microorganism. In severe cases, ] can collect fluid for culture. Special tests, such as urinalysis, can be performed if an uncommon microorganism is suspected. | |||
| *''Atypical organisms'' | |||
| :The most common bacterial causes of pneumonia are the so-called atypical bacteria '']'' and ''].'' '']'' is considered atypical but is less common. Atypical organisms are more difficult to grow, respond to different antibiotics, and were discovered more recently than the typical bacteria discovered in the early twentieth century. | |||
| Chest X-rays and ] (CT) can reveal areas of ] (seen as white), indicating consolidation.<ref name="Mandell"/> CAP does not always appear on x-rays, sometimes because the disease is in its initial stages or involves a part of the lung not clearly visible on x-ray. In some cases, chest CT can reveal pneumonia not seen on x-rays. However, ] or other types of lung damage can mimic CAP on x-ray.<ref name=Syrjala /> | |||
| *''Streptococcus pneumoniae'' | |||
| :'']'' is a common bacterial cause of CAP. Prior to the development of antibiotics and vaccination, it was a leading cause of death. Traditionally highly sensitive to ], during the 1970s resistance to multiple antibiotics began to develop. Current strains of "drug resistant Streptococcus pneumoniae" or DRSP are common, accounting for twenty percent of all Streptococcus pneumoniae infections. Adults with risk factors for DRSP including being older than 65, having exposure to children in ], having alcoholism or other severe underlying disease, or recent treatment with antibiotics should initially be treated with antibiotics effective against DRSP.{{ref|Ruhe}} | |||
| When signs of pneumonia are discovered during evaluation, chest X-rays and examination of the blood and sputum for infectious microorganisms may be done to support a diagnosis of CAP. The diagnostic tools employed will depend on the severity of illness, local practices and concern about ] of the infection. All patients with CAP should have their blood oxygen monitored with ]. In some cases, ] analysis may be required to determine the amount of oxygen in the blood. A ] (CBC) may reveal extra ]s, indicating infection.{{cn|date=March 2022}} | |||
| *''Hemophilus influenzae'' | |||
| :'']'' is another common bacterial cause of CAP. First discovered in 1892, it was initially believed to be the cause of influenza because it commonly causes CAP in people who have suffered recent lung damage from viral pneumonia. | |||
| == Prevention == | |||
| *''Enteric Gram negative bacteria'' | |||
| CAP may be prevented by treating underlying illnesses that increases its risk, by ], and by ]. Vaccination against '']'' and '']'' in the first year of life has been protective against childhood CAP. A vaccine against '']'', available for adults, is recommended for healthy individuals over 65 and all adults with COPD, ], ], ], ], ] leaks or who have had a ]. Re-vaccination may be required after five or ten years.<ref name=Butler /> | |||
| :The enteric Gram negative bacteria such as '']'' and '']'' are a group of bacteria that typically live in the human ]. Adults with risk factors for infection including residence in a ], serious ] and ] disease, and recent antibiotic use should initially be treated with antibiotics effective against Enteric Gram negative bacteria. | |||
| *''Pseudomonas aeruginosa'' | |||
| :'']'' is an uncommon cause of CAP but is a particularly difficult bacteria to treat. Individuals who are malnourished, have a lung disease called ], are on ], or have recently had strong antibiotics for a week or more should initially be treated with antibiotics effective against ''Pseudomonas aeruginosa''.{{ref|Lieberman}} | |||
| Patients who have been vaccinated against ''Streptococcus pneumoniae'', health professionals, nursing-home residents and pregnant women should be vaccinated annually against ].<ref name=CDC /> During an outbreak, drugs such as ], ], ] and ] have been demonstrated to prevent influenza.<ref name=Hayden /> | |||
| Many less common organisms cause CAP. They are typically identified because an individual has special risk factors or after treatment for the common causes has failed. These rarer causes are covered in more detail in their specific pages: ], ], ], and ]. | |||
| == Treatment == | == Treatment == | ||
| {{Multiple image|image1=Lungs with CAP Pretreatment.jpg|image2=Lungs with CAP postreatment.jpg|footer=Chest X-rays of a CAP patient before (''left'') and after treatment|footer_align=center}} | |||
| CAP is treated by administering an antibiotic which is effective in killing the offending microorganism as well as managing any complications of the infection. If the causative microorganism is unidentified, different antibiotics are tested in the laboratory in order to identify which medication will be most effective. Often, however, no microorganism is ever identified. Also, since laboratory testing can take several days, there is some delay until an organism is identified. In both cases, a person's risk factors for different organisms must be remembered when choosing the initial antibiotics (called ] therapy). Additional consideration must be given to the setting in which the individual will be treated. Most people will be fully treated after taking oral pills while other people need to be hospitalized for ] antibiotics and, possibly, ]. In general, all therapies in older children and adults will include treatment for atypical bacteria. Typically this is a macrolide antibiotic such as ] or ] although a ] such as ] can substitute. ] is now the antibiotic of choice in the UK for complete coverage of the atypical bacteria. This is due to increased levels of clostridium difficile seen in hospital patients being linked to the increased use of ]. | |||
| CAP is treated with an antibiotic that kills the infecting microorganism; treatment also aims at managing complications. If the causative microorganism is unidentified, which is often the case, the laboratory identifies the most effective antibiotic; this may take several days. | |||
| Health professionals consider a person's risk factors for various organisms when choosing an initial antibiotic. Additional consideration is given to the treatment setting; most patients are cured by oral medication, while others must be hospitalized for ] or ]. | |||
| === ''Newborn infants'' === | |||
| Current treatment guidelines recommend a beta-lactam, like amoxicillin, and a macrolide, like azithromycin or clarithromycin, or a ], such as ]. ] is the antibiotic of choice in the UK for atypical bacteria, due to increased ] in hospital patients linked to the increased use of ]. | |||
| Most newborn infants with CAP are hospitalized and given ] ] and ] for at least ten days. This treats the common bacteria '']'', '']'', and '']''. If ] is the cause, intravenous ] is administered for 21 days. | |||
| ] and ] are often used to treat community-acquired pneumonia, which usually presents with a few days of cough, fever, and shortness of breath. Chest x-ray typically reveals a lobar infiltrate (rather than diffuse).<ref>{{Cite web|title=UWorld {{!}} Test Prep for NCLEX, SAT, ACT, MCAT, USMLE & More!|url=https://www.uworld.com/|access-date=2021-01-25|website=UWorld Test Prep}}</ref> | |||
| === ''Children'' === | |||
| Treatment of CAP in children depends on both the age of the child and the severity of his/her illness. Children less than five do not typically receive treatment to cover atypical bacteria. If a child does not need to be hospitalized, ] for seven days is a common treatment. However, with increasing prevalence of DRSP, other agents such as ] will most likely become more popular in the future.{{ref|Bradley}} Hospitalized children should receive intravenous ], ], or ]. | |||
| === |
=== Newborns === | ||
| Most newborn infants with CAP are hospitalized, receiving IV ] and ] for at least ten days to treat the common causative agents '']'', '']'' and '']''. To treat the ], IV ] is administered for 21 days. | |||
| === Children === | |||
| In 2001, the American Thoracic Society, drawing on work by the British and Canadian Thoracic Societies, established guidelines for the management of adults with CAP which divided individuals with CAP into four categories based upon common organisms encountered.{{ref|Neiderman}} | |||
| Treatment of CAP in children depends on the child's age and the severity of illness. Children under five are not usually treated for atypical bacteria. If hospitalization is not required, a seven-day course of ] is often prescribed, with ] as an alternative when there is allergy to penicillins.<ref name="ReferenceA">{{cite journal|last1=Lodha|first1=R|last2=Kabra|first2=SK|last3=Pandey|first3=RM|title=Antibiotics for community-acquired pneumonia in children.|journal=The Cochrane Database of Systematic Reviews|date=4 June 2013|volume=2013|issue=6|pages=CD004874|pmid=23733365|doi=10.1002/14651858.CD004874.pub4|pmc=7017636}}</ref> Further studies are needed to confirm the efficacy of newer antibiotics.<ref name="ReferenceA"/> With the increase in ], antibiotics such as ] may become more popular.<ref name=Bradley /> Hospitalized children receive intravenous ], ] or ], and a recent study found that a three-day course of antibiotics seems sufficient for most mild-to-moderate CAP in children.<ref name=pmid18729535>{{cite journal |vauthors=Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, Grammatikos AP, Athanassa Z, Falagas ME |title=Short- versus long-course antibacterial therapy for community-acquired pneumonia : a meta-analysis |journal=Drugs |volume=68 |issue=13 |pages=1841–54 |year=2008 |pmid=18729535 |doi=10.2165/00003495-200868130-00004|doi-access=free }}</ref> | |||
| === Adults === | |||
| *''Healthy outpatients without risk factors'' | |||
| In 2001 the ], drawing on the work of the ] and ], established guidelines for the management of adult CAP by dividing patients into four categories based on common organisms:<ref name=Neiderman /> | |||
| :This group, the largest, is composed of otherwise healthy patients without risk factors for DRSP, enteric Gram negative bacteria, ''Pseudomonas'', or other less common causes of CAP. The primary microoganisms in this group are viruses, atypical bacteria, penicillin sensitive ''Streptococcus pneumoniae'', and ''Hemophilus influenzae''. Recommended management is with a macrolide antibiotic such as ] or ] for seven<ref name="pmid17765048"> | |||
| * Healthy outpatients without risk factors: This group (the largest) is composed of otherwise-healthy patients without risk factors for DRSP, enteric ], ''Pseudomonas'' or other, less common, causes of CAP. Primary microorganisms are viruses, atypical bacteria, penicillin-sensitive ''Streptococcus pneumoniae'' and '']''. Recommended drugs are macrolide antibiotics, such as ] or ], for seven<ref name="pmid17765048">{{cite journal |vauthors=Li JZ, Winston LG, Moore DH, Bent S |title=Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis |journal=The American Journal of Medicine |volume=120 |issue=9 |pages=783–90 |date=September 2007 |pmid=17765048 |doi=10.1016/j.amjmed.2007.04.023}}</ref> to ten days. A shorter course of these antibiotics has been investigated, however, there is not sufficient evidence to make recommendations.<ref>{{cite journal |last1=López-Alcalde |first1=Jesús |last2=Rodriguez-Barrientos |first2=Ricardo |last3=Redondo-Sánchez |first3=Jesús |last4=Muñoz-Gutiérrez |first4=Javier |last5=Molero García |first5=José María |last6=Rodríguez-Fernández |first6=Carmen |last7=Heras-Mosteiro |first7=Julio |last8=Marin-Cañada |first8=Jaime |last9=Casanova-Colominas |first9=Jose |last10=Azcoaga-Lorenzo |first10=Amaya |last11=Hernandez Santiago |first11=Virginia |last12=Gómez-García |first12=Manuel |title=Short-course versus long-course therapy of the same antibiotic for community-acquired pneumonia in adolescent and adult outpatients |journal=Cochrane Database of Systematic Reviews |date=6 September 2018 |volume=2018 |issue=9 |pages=CD009070 |doi=10.1002/14651858.CD009070.pub2|pmid=30188565 |pmc=6513237 |hdl=10023/18430 |hdl-access=free }}</ref> | |||
| Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007 Sep;120(9):783-90. PMID 17765048</ref> to ten days. | |||
| * Outpatients with underlying illness or risk factors: Although this group does not require hospitalization, they have underlying health problems such as emphysema or heart failure or are at risk for DRSP or enteric gram-negative bacteria. They may be treated with a quinolone active against ''Streptococcus pneumoniae'' (such as ]) or a ] (such as ], ], ] or ]) and a macrolide antibiotic, such as ] or ], for seven to ten days.<ref>{{cite journal |vauthors=Vardakas KZ, Siempos II, Grammatikos A, Athanassa Z, Korbila IP, Falagas ME |title=Respiratory fluoroquinolones for the treatment of community-acquired pneumonia: a meta-analysis of randomized controlled trials |journal=CMAJ |volume=179 |issue=12 |pages=1269–77 |date=December 2008 |pmid=19047608 |pmc=2585120 |doi=10.1503/cmaj.080358}}</ref> | |||
| * Hospitalized patients without risk for ''Pseudomonas'': This group requires intravenous antibiotics, with a quinolone active against ''Streptococcus pneumoniae'' (such as ]), a β-lactam antibiotic (such as cefotaxime, ceftriaxone, ] or high-dose ampicillin plus a macrolide antibiotic (such as ] or ]) for seven to ten days. | |||
| * Intensive-care patients at risk for '']'': These patients require antibiotics targeting this difficult-to-eradicate bacterium. One regimen is an intravenous antipseudomonal beta-lactam such as ], ], ] or ], plus an IV antipseudomonal fluoroquinolone such as ]. Another is an IV antipseudomonal beta-lactam such as cefepime, imipenem, meropenem or piperacillin/tazobactam, plus an aminoglycoside such as ] or ], plus a macrolide (such as azithromycin) or a nonpseudomonal fluoroquinolone such as ]. | |||
| For mild-to-moderate CAP, shorter courses of antibiotics (3–7 days) seem to be sufficient.<ref name=pmid18729535/> | |||
| *''Outpatients with underlying illness and/or risk factors'' | |||
| :This group does not require hospitalization; its members either have underlying health problems (such as ] or ]) or is at risk for DRSP and/or enteric Gram negative bacteria. Treatment is with a ] active against ''Streptococcus pneumoniae'' such as ] or a ] such as ], ], ], or ] plus a macrolide antibiotic such as ] or ] for seven to ten days. | |||
| Some patients with CAP will be at increased risk of death despite antimicrobial treatment. A key reason for this is the host's exaggerated inflammatory response. There is a tension between controlling the infection on one hand and minimizing damage to other tissues on the other. Some recent research focuses on immunomodulatory therapy that can modulate the immune response in order to reduce injury to the lung and other affected organs such as the heart. Although the evidence for these agents has not resulted in their routine use, their potential benefits are promising.<ref>Woods DR, José RJ. Current and emerging evidence for immunomodulatory therapy in community-acquired pneumonia. Ann Res Hosp 2017;1:33 http://arh.amegroups.com/article/view/3806</ref> | |||
| *''Hospitalized individuals not at risk for Pseudomonas'' | |||
| :This group requires hospitalization and administration of intravenous antibiotics. Treatment is with either an intravenous ] active against ''Streptococcus pneumoniae'' such as ] or ] such as cefotaxime, ceftriaxone, ampicillin/sulbactam, or high-dose ampicillin plus an intravenous macrolide antibiotic such as ] or ] for seven to ten days. | |||
| === {{anchor|Hospitalize}}Hospitalization === | |||
| *''Individuals requiring intensive care at risk for Pseudomonas'' | |||
| Some CAP patients require intensive care, with ]s such as the ] and ] guiding the decision whether or not to hospitalize.<ref name=Fine /> Factors increasing the need for hospitalization include: | |||
| :Individuals being treated in an intensive care unit with risk factors for infection with ''Pseudomonas aeruginosa'' require specific antibiotics targeting this difficult to eradicate bacteria. One possible regimen is an intravenous antipseudomonal beta-lactam such as ], ], ], or ] plus an intravenous antipseudomonal fluoroquinolone such as ]. Another recommended regimen is an intravenous antipseudomonal beta-lactam such as cefepime, imipenem, meropenem, or piperacillin/ tazobactam plus an intravenous aminoglycoside such as ] or ] plus either an intravenous macrolide such azithromycin or an intravenous nonpseudomonal fluoroquinolone such as ]. | |||
| * Age greater than 65 | |||
| * Underlying chronic illnesses | |||
| * ] greater than 30 per minute | |||
| * Systolic ] less than 90 ] | |||
| * ] greater than 125 per minute | |||
| * ] below 35 or over 40 °C | |||
| * Confusion | |||
| * Evidence of infection outside the lung | |||
| Laboratory results indicating hospitalization include: | |||
| === The decision to hospitalize === | |||
| * Arterial oxygen tension less than 60 mm Hg | |||
| Some people with CAP require hospitalization and more intensive care than the majority. In general, a discussion between the individual and his or her health care provider determines the need for hospitalization. ]s, such as the ] and ] have been developed to help guide the decision.{{ref|Fine}} Factors which increase the need for hospitalization include age greater than 65; underlying chronic illnesses; a ] greater than thirty breaths per minute; a systolic ] less than 90 mmHg; a ] greater than 125 per minute; ] less than 35 or greater than 40°C; confusion; and evidence of infection outside the lung. Laboratory results which increase the need for hospitalization include arterial oxygen tension less than 60 mm Hg, ] of greater than 50 mmHg, or ] less than 7.35 while breathing room air; ] less than 30%; ] greater than 1.2 mg/dl or ] greater than 20 mg/ dl; white blood cell count less than 4 × 10^9/L or greater than 30 × 10^9/L; and absolute neutrophil count less than 1 x 10^9/L. X-ray findings which increase the need for hospitalization include involvement of more than one lobe of the ], presence of a cavity, and the presence of a ]. | |||
| * ] over 50 mmHg or ] under 7.35 while breathing room air | |||
| * ] under 30 percent | |||
| * ] over 1.2 mg/dl or ] over 20 mg/dl | |||
| * White-blood-cell count under 4 × 10^9/L or over 30 × 10^9/L | |||
| * Neutrophil count under 1 x 10^9/L | |||
| X-ray findings indicating hospitalization include: | |||
| * Involvement of more than one lobe of the ] | |||
| * Presence of a cavity | |||
| * ] | |||
| == Prognosis == | == Prognosis == | ||
| The CAP outpatient mortality rate is less than one percent, with fever typically responding within the first two days of therapy, and other symptoms abating in the first week. However, X-rays may remain abnormal for at least a month. Hospitalized patients have an average mortality rate of 12 percent, with the rate rising to 40 percent for patients with bloodstream infections or those who require intensive care.<ref name=Woodhead /> Factors increasing mortality are identical to those indicating hospitalization. | |||
| When CAP does not respond |
When CAP does not respond to treatment, this may indicate a previously unknown health problem, a treatment complication, inappropriate antibiotics for the causative organism, a previously unsuspected microorganism (such as ]) or a condition mimicking CAP (such as ] with polyangiitis). Additional tests include ], ] or lung ]. | ||
| == Complications of CAP == | |||
| Despite appropriate antibiotic therapy, severe complications can result from CAP, including: | |||
| === ''Sepsis'' === | |||
| ] can occur when microorganisms enter the blood stream and the ] responds. Sepsis most often occurs with ]; ''Streptococcus pneumoniae'' is the most common cause. Individuals with sepsis require hospitalization in an intensive care unit. They often require medications and intravenous fluids to keep their blood pressure from going too low. Sepsis can cause liver, kidney, and heart damage among other things. | |||
| === ''Respiratory failure'' === | |||
| Because CAP affects the lungs, often individuals with CAP have difficulty breathing. If enough of the lung is involved, it may not be possible for a person to breathe enough to live without support. Non-invasive machines such as a ] machine may be used. Otherwise, placement of a ] into the mouth may be necessary and a ] may be used to help the person breathe. | |||
| === ''Pleural effusion and empyema'' === | |||
| Occasionally, microorganisms from the lung will cause fluid to form in the space surrounding the lung, called the ]. If the microorganisms themselves are present, the fluid collection is often called an ]. If pleural fluid is present in a person with CAP, the fluid should be collected with a needle (]) and examined. Depending on the result of the examination, complete drainage of the fluid may be necessary, often with a ]. If the fluid is not drained, bacteria can continue to cause illness because antibiotics do not penetrate well into the pleural cavity. | |||
| === ''Abscess'' === | |||
| Rarely, microorganisms in the lung will form a pocket of fluid and bacteria called an ]. Abscesses can be seen on an x-ray as a cavity within the lung. Abscesses typically occur in ] and most often contain a mixture of ]. Usually antibiotics are able to fully treat abscesses, but sometimes they must be drained by a ] or ]. | |||
| == Special circumstances leading to CAP == | |||
| Some people have an underlying problem which increases their risk of getting an infection. Some important situations are covered below: | |||
| === ''Obstruction'' === | |||
| When part of the airway (]) leading to the alveoli is obstructed, the lung is not able to clear fluid when it accumulates. This can lead to infection of the fluid resulting in CAP. One cause of obstruction, especially in young children, is inhalation of a foreign object such as a marble or toy. The object is lodged in the small airways and pneumonia can form in the trapped areas of lung. Another cause of obstruction is ], which can grow into the airways block the flow of air. | |||
| === ''Lung disease'' === | |||
| People with underlying lung disease are more likely to develop CAP. Diseases such as ] or habits such as ] result in more frequent and more severe bouts of CAP. In children, recurrent episodes of CAP may be the first clue to diseases such as ] or ]. | |||
| === ''Immune problems'' === | |||
| People who have ] are more likely to get CAP. People who have ] are much more likely to develop CAP. Other immune problems range from severe immune deficiencies of childhood such as ] to less severe deficiencies such as ].{{ref|Mundy}} | |||
| == Epidemiology == | == Epidemiology == | ||
| CAP is |
CAP is common worldwide, and is a major cause of death in all age groups. In children, most deaths (over two million a year) occur in the newborn period. According to a ] estimate, one in three newborn deaths result from pneumonia.<ref name=Garenne /> Mortality decreases with age until late adulthood, with the elderly at risk for CAP and its associated mortality. | ||
| More cases |
More CAP cases occur during the winter than at other times of the year. CAP is more common in males than females, and more common in black people than Caucasians.<ref>{{Cite journal|last1=Ramirez|first1=Julio A|last2=Wiemken|first2=Timothy L|last3=Peyrani|first3=Paula|last4=Arnold|first4=Forest W|last5=Kelley|first5=Robert|last6=Mattingly|first6=William A|last7=Nakamatsu|first7=Raul|last8=Pena|first8=Senen|last9=Guinn|first9=Brian E|date=2017-07-28|title=Adults Hospitalized With Pneumonia in the United States: Incidence, Epidemiology, and Mortality|journal=Clinical Infectious Diseases|language=en|volume=65|issue=11|pages=1806–1812|doi=10.1093/cid/cix647|pmid=29020164|issn=1058-4838|doi-access=free}}</ref> Patients with underlying illnesses (such as ], ], COPD, ], ] or ]) have an increased risk of developing pneumonia.<ref name=Almirall /> | ||
| == |
==See also== | ||
| * ] | |||
| In addition to treating any underlying illness which can increase a person's risk for CAP, there are several additional ways to prevent CAP. ] is important not only for treatment of any underlying lung disease, but also because cigarette smoke interferes with many of the body's natural defenses against CAP. | |||
| * ] | |||
| * ] | |||
| * ] | |||
| == References == | |||
| ] is important in both children and adults. Vaccinations against '']'' and '']'' in the first year of life have greatly reduced their role in CAP in children. A vaccine against '']'' is also available for adults and is currently recommended for all healthy individuals older than 65 and any adults with ], ], ], ] of the ], ], ] leaks, or who do not have a ]. A repeat vaccination may also be required after five or ten years.{{ref|Butler}} | |||
| {{Reflist|2|refs= | |||
| <ref name=Metaly> | |||
| {{cite journal |vauthors=Metlay JP, Schulz R, Li YH |title=Influence of age on symptoms at presentation in patients with community-acquired pneumonia |journal=Archives of Internal Medicine |volume=157 |issue=13 |pages=1453–9 |date=July 1997 |pmid=9224224 |doi=10.1001/archinte.157.13.1453|display-authors=etal}}</ref> | |||
| <ref name=Metlay>{{cite journal |vauthors=Metlay JP, Kapoor WN, Fine MJ |title=Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination |journal=JAMA |volume=278 |issue=17 |pages=1440–5 |date=November 1997 |pmid=9356004 |doi=10.1001/jama.278.17.1440}}</ref> | |||
| <ref name=Syrjala>{{cite journal |vauthors=Syrjälä H, Broas M, Suramo I, Ojala A, Lähde S |title=High-resolution computed tomography for the diagnosis of community-acquired pneumonia |journal=Clinical Infectious Diseases |volume=27 |issue=2 |pages=358–63 |date=August 1998 |pmid=9709887 |doi=10.1086/514675|doi-access=free }}</ref> | |||
| <ref name=Webber>{{cite journal |vauthors=Webber S, Wilkinson AR, Lindsell D, Hope PL, Dobson SR, Isaacs D |title=Neonatal pneumonia |journal=Archives of Disease in Childhood |volume=65 |issue=2 |pages=207–11 |date=February 1990 |pmid=2107797 |pmc=1792235 |doi=10.1136/adc.65.2.207}}</ref> | |||
| <ref name=Abzug>{{cite journal |vauthors=Abzug MJ, Beam AC, Gyorkos EA, Levin MJ |title=Viral pneumonia in the first month of life |journal=The Pediatric Infectious Disease Journal |volume=9 |issue=12 |pages=881–5 |date=December 1990 |pmid=2177540 |doi=10.1097/00006454-199012000-00005|s2cid=2653523 }}</ref> | |||
| <ref name=Wubbel>{{cite journal |vauthors=Wubbel L, Muniz L, Ahmed A |title=Etiology and treatment of community-acquired pneumonia in ambulatory children |journal=The Pediatric Infectious Disease Journal |volume=18 |issue=2 |pages=98–104 |date=February 1999 |pmid=10048679 |doi=10.1097/00006454-199902000-00004|display-authors=etal}}</ref> | |||
| <ref name=Roux>{{cite journal |vauthors=de Roux A, Marcos MA, Garcia E |title=Viral community-acquired pneumonia in nonimmunocompromised adults |journal=Chest |volume=125 |issue=4 |pages=1343–51 |date=April 2004 |pmid=15078744 |doi=10.1378/chest.125.4.1343|display-authors=etal}}</ref> | |||
| <ref name=Bradley>{{cite journal |author=Bradley JS |title=Management of community-acquired pediatric pneumonia in an era of increasing antibiotic resistance and conjugate vaccines |journal=The Pediatric Infectious Disease Journal |volume=21 |issue=6 |pages=592–8; discussion 613–4 |date=June 2002 |pmid=12182396 |doi=10.1097/00006454-200206000-00035|s2cid=20412452 }}</ref> | |||
| <ref name=Neiderman>{{cite journal |vauthors=Niederman MS, Mandell LA, Anzueto A |title=Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention |journal=American Journal of Respiratory and Critical Care Medicine |volume=163 |issue=7 |pages=1730–54 |date=June 2001 |pmid=11401897 |doi=10.1164/ajrccm.163.7.at1010|display-authors=etal}}</ref> | |||
| <ref name=Mundy>{{cite journal |vauthors=Mundy LM, Auwaerter PG, Oldach D |title=Community-acquired pneumonia: impact of immune status |journal=American Journal of Respiratory and Critical Care Medicine |volume=152 |issue=4 Pt 1 |pages=1309–15 |date=October 1995 |pmid=7551387 |doi=10.1164/ajrccm.152.4.7551387|display-authors=etal}}</ref> | |||
| <ref name=Fine>{{cite journal |vauthors=Fine MJ, Auble TE, Yealy DM |title=A prediction rule to identify low-risk patients with community-acquired pneumonia |journal=The New England Journal of Medicine |volume=336 |issue=4 |pages=243–50 |date=January 1997 |pmid=8995086 |doi=10.1056/NEJM199701233360402|display-authors=etal|doi-access=free }}</ref> | |||
| <ref name=Woodhead>{{cite journal |vauthors=Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG |title=Prospective study of the aetiology and outcome of pneumonia in the community |journal=Lancet |volume=1 |issue=8534 |pages=671–4 |date=March 1987 |pmid=2882091 |doi=10.1016/S0140-6736(87)90430-2|s2cid=34844819 }}</ref> | |||
| <ref name=Garenne>{{cite journal |vauthors=Garenne M, Ronsmans C, Campbell H |title=The magnitude of mortality from acute respiratory infections in children under 5 years in developing countries |journal=World Health Statistics Quarterly |volume=45 |issue=2–3 |pages=180–91 |year=1992 |pmid=1462653}}</ref> | |||
| <ref name=Almirall>{{cite journal |vauthors=Almirall J, Bolíbar I, Balanzó X, González CA |title=Risk factors for community-acquired pneumonia in adults: a population-based case-control study |journal=The European Respiratory Journal |volume=13 |issue=2 |pages=349–55 |date=February 1999 |pmid=10065680 |doi=10.1183/09031936.99.13234999|doi-access=free }}</ref> | |||
| <ref name=Butler>{{cite journal |vauthors=Butler JC, Breiman RF, Campbell JF, Lipman HB, Broome CV, Facklam RR |title=Pneumococcal polysaccharide vaccine efficacy. An evaluation of current recommendations |journal=JAMA |volume=270 |issue=15 |pages=1826–31 |date=October 1993 |pmid=8411526 |doi=10.1001/jama.270.15.1826}}</ref> | |||
| <ref name=CDC>{{cite journal |author=Centers for Disease Control and Prevention |title=Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP) |journal=MMWR Recomm Rep |volume=48 |issue=RR–4 |pages=1–28 |date=April 1999 |pmid=10366138 |url=https://www.cdc.gov/mmwr/preview/mmwrhtml/00057028.htm}}</ref> | |||
| <ref name=Hayden>{{cite journal |vauthors=Hayden FG, Atmar RL, Schilling M |title=Use of the selective oral neuraminidase inhibitor oseltamivir to prevent influenza |journal=The New England Journal of Medicine |volume=341 |issue=18 |pages=1336–43 |date=October 1999 |pmid=10536125 |doi=10.1056/NEJM199910283411802|display-authors=etal|doi-access=free }}</ref> | |||
| }} | |||
| * {{cite journal |vauthors=Mandell LA, Wunderink RG, Anzueto A |title=Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults |journal=Clinical Infectious Diseases |volume=44 |issue=Suppl 2 |pages=S27–72 |date=March 2007 |pmid=17278083 |doi=10.1086/511159|display-authors=etal|doi-access=free |pmc=7107997 }} | |||
| == External links == | |||
| ] vaccines should be given yearly to the same individuals as receive vaccination against '']''. In addition, health care workers, nursing home residents, and pregnant women should receive the vaccine.{{ref|CDC}} When an influenza outbreak is occurring, medications such as ], ], ], and ] have been shown to prevent cases of influenza.{{ref|Hayden}} | |||
| * | |||
| {{Respiratory pathology}} | |||
| ==References== | |||
| {{ |
{{pneumonia}} | ||
| #{{note|Sharma}} | |||
| #{{note|Metaly}} Metaly JP, Schulz R, Li Y-H, Singer DE, Marrie TJ, Coley CM, Hough LJ, Obrosky DS, Kapoor WN, Fine MJ. ''Influence of age on symptoms at presentation in patients with community-acquired pneumonia.'' Arch Intern Med 1997; 157: 1453-1459 PMID 9224224 | |||
| #{{note|Metlay}} Metlay, JP, Kapoor, WN, Fine, MJ. D''oes this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination.'' JAMA 1997; 278:1440. PMID 9356004 | |||
| #{{note|Syrjala}} Syrjala H, Broas M, Suramo I, Ojala A, Lahde S. ''High resolution computed tomography for the diagnosis of community-acquired pneumonia.'' Clin Infect Dis 1998; 27: 358-363 PMID 9709887 | |||
| #{{note|Webber}} Webber, S, Wilkinson, AR, Lindsell, D, et al. ''Neonatal pneumonia.'' Arch Dis Child 1990; 65:207.PMID 2107797 | |||
| #{{note|Abzug}} Abzug, MJ, Beam, AC, Gyorkos, EA, Levin, MJ. ''Viral pneumonia in the first month of life.'' Pediatr Infect Dis J 1990; 9:881. PMID 2177540 | |||
| #{{note|Wubbel}} Wubbel, L, Muniz, L, Ahmed, A, et al. ''Etiology and treatment of community-acquired pneumonia in ambulatory children. Pediatr Infect Dis J 1999; 18:98.'' PMID 10048679 | |||
| #{{note|Roux}} de Roux, A, Marcos, MA, Garcia, E, et al. ''Viral community-acquired pneumonia in nonimmunocompromised adults.'' Chest 2004; 125:1343.PMID 15078744 | |||
| #{{note|Ruhe}} Ruhe, JJ, Myers, L, Mushatt, D, Hasbun, R. ''High-level penicillin-nonsusceptible Streptococcus pneumoniae bacteremia: identification of a low-risk subgroup.'' Clin Infect Dis 2004; 38:508 PMID 14765343 | |||
| #{{note|Lieberman}} Lieberman D, Schlaeffer F, Boldur I, Lieberman D, Horowitz S, Friedman MG, Leiononen M, Horovitz O, Manor E, Porath A. ''Multiple pathogens in adult patients admitted with community-acquired pneumonia: a one year prospective study of 346 consecutive patients.'' Thorax 1996; 51: 179-184 PMID 8711652 | |||
| #{{note|Bradley}} Bradley, JS. ''Management of community-acquired pediatric pneumonia in an era of increasing antibiotic resistance and conjugate vaccines.'' Pediatr Infect Dis J 2002; 21:592. PMID 12182396 | |||
| #{{note|Neiderman}} Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, Dean N, File T, Fine MJ, Gross PA, et al. ''Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention.'' Am J Respir Crit Care Med 2001;163:1730–1754 PMID 11401897 | |||
| #{{note|Mundy}} Mundy, LM, Auwaerter, PG, Oldach, D, et al. ''Community-acquired pneumonia: impact of immune status.'' Am J Respir Crit Care Med 1995; 152:1309. PMID 7551387 | |||
| #{{note|Fine}} Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. ''A prediction rule to identify low-risk patients with community-acquired pneumonia.'' N Engl J Med 1997; 336: 243-250 PMID 8995086 | |||
| #{{note|Woodhead}} Woodhead MA, MacFarlane JT, McCracken JS, Rose DH, Finch RG. ''Prospective study of the aetiology and outcome of pneumonia in the community.'' Lancet 1987; i: 671-674. PMID 2882091 | |||
| #{{note|Garenne}} Garenne, M, Ronsmans, C, Campbell, H. ''The magnitude of mortality from acute respiratory infections in children under 5 years in developing countries.'' World Health Stat Q 1992; 45:180. PMID 1462653 | |||
| #{{note|Almirall}} Almirall, J, Bolibar, I, Balanzo, X, Gonzalez, CA. ''Risk factors for community-acquired pneumonia in adults: A population-based case-control study.'' Eur Respir J 1999; 13:349. PMID 10065680 | |||
| #{{note|Butler}} Butler JC, Breiman RF, Campbell JF, Lipman HB, Broome CV, Facklam RR. ''Pneumococcal polysaccharide vaccine efficacy: an evaluation of current recommendations.'' JAMA 1993; 270: 1826-1831. PMID 8411526 | |||
| #{{note|CDC}} Centers for Disease Control and Prevention. ''Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP)''. MMWR 1999;48(RR-4):1-28. | |||
| #{{note|Hayden}} Hayden FG, Atmar RL, Schilling M, Johnson C, Poretz D, Paar D, Huson L, Ward P, Mills RG. ''Use of the selective oral neuraminidase inhibitor oseltamivir to prevent influenza.'' N Engl J Med 1999; 341: 1336-1343 PMID 10536125 | |||
| Infectious Disease Society of America Guidelines | |||
| http://www.journals.uchicago.edu/doi/pdf/10.1086/511159?cookieSet=1 | |||
| ==See also== | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| {{Respiratory pathology}} | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
Latest revision as of 18:53, 20 October 2024
Medical condition
| Community-acquired pneumonia | |
|---|---|
| Other names | CAP |
| Specialty | Infectious diseases, pulmonology |
Community-acquired pneumonia (CAP) refers to pneumonia (any of several lung diseases) contracted by a person outside of the healthcare system. In contrast, hospital-acquired pneumonia (HAP) is seen in patients who have recently visited a hospital or who live in long-term care facilities. CAP is common, affecting people of all ages, and its symptoms occur as a result of oxygen-absorbing areas of the lung (alveoli) filling with fluid. This inhibits lung function, causing dyspnea, fever, chest pains and cough.
CAP, the most common type of pneumonia, is a leading cause of illness and death worldwide. Its causes include bacteria, viruses, fungi and parasites. CAP is diagnosed by assessing symptoms, performing a physical examination, by x-ray or by sputum examination. Patients with CAP sometimes require hospitalization, and it is treated primarily with antibiotics, antipyretics and cough medicine. Some forms of CAP can be prevented by vaccination and by abstaining from tobacco products.
Signs and symptoms
Common symptoms
- Coughing which produces greenish or yellow sputum
- A high fever, accompanied by sweating, chills and shivering
- Sharp, stabbing chest pains
- Rapid, shallow, often painful breathing
Less-common symptoms
- Coughing up blood (hemoptysis)
- Headaches, including migraines
- Loss of appetite
- Excessive fatigue
- Bluish skin (cyanosis)
- Nausea
- Vomiting
- Diarrhea
- Joint pain (arthralgia)
- Muscle aches (myalgia)
- Rapid heartbeat
- Dizziness or lightheadedness
In the elderly
- New or worsening confusion
- Hypothermia
- Poor coordination, which may lead to falls
In infants
- Unusual sleepiness
- Yellowing of the skin (jaundice)
- Difficulty feeding
Complications
Major complications of CAP include:
- Sepsis - A life-threatening reaction to infection. A common cause of sepsis is bacterial pneumonia, frequently the result of infection with streptococcus pneumoniae. Patients with sepsis require intensive care with blood pressure monitoring and support against hypotension. Sepsis can cause liver, kidney and heart damage.
- Respiratory failure - CAP patients often have dyspnea, which may require support. Non-invasive machines (such as bilevel positive airway pressure), a tracheal tube or a ventilator may be used.
- Pleural effusion and empyema - Microorganisms from the lung may trigger fluid collection in the pleural cavity, or empyema. Pleural fluid, if present, should be collected with a needle and examined. Depending on the results, complete drainage of the fluid with a chest tube may be necessary to prevent proliferation of the infection. Antibiotics, which do not penetrate the pleural cavity well, are less effective.
- Abscess - A pocket of fluid and bacteria may appear on X-ray as a cavity in the lung. Abscesses, typical of aspiration pneumonia, usually contain a mixture of anaerobic bacteria. Although antibiotics can usually cure abscesses, sometimes they require drainage by a surgeon or radiologist.
Causes
Many different microorganisms can cause CAP. However, the most common cause is Streptococcus pneumoniae. Certain groups of people are more susceptible to CAP-causing pathogens - infants, adults with chronic conditions (such as chronic obstructive pulmonary disease), and senior citizens. Alcoholics and others with compromised immune systems are more likely to develop CAP from Haemophilus influenzae or Pneumocystis jirovecii. A definitive cause is identified in only half the cases.
Neonates and infants
It is possible for a fetus to develop a lung infection before birth by aspirating infected amniotic fluid or through a blood-borne infection which crossed the placenta. Infants can also inhale contaminated fluid from the vagina at birth. The most prevalent pathogen causing CAP in newborns is Streptococcus agalactiae, also known as group-B streptococcus (GBS). GBS causes more than half of CAP in the first week after birth. Other bacterial causes of neonatal CAP include Listeria monocytogenes and a variety of mycobacteria. CAP-causing viruses may also be transferred from mother to child; herpes simplex virus, the most common, is life-threatening, and adenoviridae, mumps and enterovirus can also cause pneumonia. Another cause of neonatal CAP is Chlamydia trachomatis, which, though acquired at birth, does not cause pneumonia until two to four weeks later. It usually presents with no fever and a characteristic, staccato cough.
CAP in older infants reflects increased exposure to microorganisms, with common bacterial causes including Streptococcus pneumoniae, Escherichia coli, Klebsiella pneumoniae, Moraxella catarrhalis and Staphylococcus aureus. Maternally-derived syphilis is also a cause of CAP in infants. Viral causes include human respiratory syncytial virus (RSV), human metapneumovirus, adenovirus, human parainfluenza viruses, influenza and rhinovirus, and RSV is a common source of illness and hospitalization in infants. CAP caused by fungi or parasites is not usually seen in otherwise-healthy infants.
Children
Although children older than one month tend to be at risk for the same microorganisms as adults, children under five years of age are much less likely to have pneumonia caused by Mycoplasma pneumoniae, Chlamydophila pneumoniae or Legionella pneumophila than older children. In contrast, older children and teenagers are more likely to acquire Mycoplasma pneumoniae and Chlamydophila pneumoniae than adults.
Adults
A full spectrum of microorganisms is responsible for CAP in adults, and patients with certain risk factors are more susceptible to infections by certain groups of microorganisms. Identifying people at risk for infection by these organisms aids in appropriate treatment. Many less-common organisms can cause CAP in adults; these may be determined by identifying specific risk factors, or when treatment for more common causes fails.
Risk factors
Some patients have an underlying problem which increases their risk of infection. Some risk factors are:
- Obstruction - When part of the airway (bronchus) leading to the alveoli is obstructed, the lung cannot eliminate fluid; this can lead to pneumonia. One cause of obstruction, especially in young children, is inhalation of a foreign object such as a marble or toy. The object lodges in a small airway, and pneumonia develops in the obstructed area of the lung. Another cause of obstruction is lung cancer, which can block the flow of air.
- Lung disease - Patients with underlying lung disease are more likely to develop pneumonia. Diseases such as emphysema and habits such as smoking result in more frequent and more severe bouts of pneumonia. In children, recurrent pneumonia may indicate cystic fibrosis or pulmonary sequestration.
- Immune problems - Immune-deficient patients, such as those with HIV/AIDS, are more likely to develop pneumonia. Other immune problems that increase the risk of developing pneumonia range from severe childhood immune deficiencies, such as Wiskott–Aldrich syndrome, to the less severe common variable immunodeficiency.
Pathophysiology
The symptoms of CAP are the result of lung infection by microorganisms and the response of the immune system to the infection. Mechanisms of infection are different for viruses and other microorganisms.
Viruses
Up to 20 percent of CAP cases can be attributed to viruses. The most common viral causes are influenza, parainfluenza, human respiratory syncytial virus, human metapneumovirus and adenovirus. Less common viruses which may cause serious illness include chickenpox, SARS, avian flu and hantavirus.
Typically, a virus enters the lungs through the inhalation of water droplets and invades the cells lining the airways and the alveoli. This leads to cell death; the cells are killed by the virus or they self-destruct. Further lung damage occurs when the immune system responds to the infection. White blood cells, particularly lymphocytes, activate chemicals known as cytokines which cause fluid to leak into the alveoli. The combination of cell destruction and fluid-filled alveoli interrupts the transportation of oxygen into the bloodstream. In addition to their effects on the lungs, many viruses affect other organs. Viral infections weaken the immune system, making the body more susceptible to bacterial infection, including bacterial pneumonia.
Bacteria and fungi
Although most cases of bacterial pneumonia are caused by Streptococcus pneumoniae, infections by atypical bacteria such as Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Legionella pneumophila can also cause CAP. Enteric gram-negative bacteria, such as Escherichia coli and Klebsiella pneumoniae, are a group of bacteria that typically live in the large intestine; contamination of food and water by these bacteria can result in outbreaks of pneumonia. Pseudomonas aeruginosa, an uncommon cause of CAP, is a difficult bacteria to treat.
Bacteria and fungi typically enter the lungs by inhalation of water droplets, although they can reach the lung through the bloodstream if an infection is present. In the alveoli, bacteria and fungi travel into the spaces between cells and adjacent alveoli through connecting pores. The immune system responds by releasing neutrophil granulocytes, white blood cells responsible for attacking microorganisms, into the lungs. The neutrophils engulf and kill the microorganisms, releasing cytokines which activate the entire immune system. This response causes fever, chills and fatigue, common symptoms of CAP. The neutrophils, bacteria and fluids leaked from surrounding blood vessels fill the alveoli, impairing oxygen transport. Bacteria may travel from the lung to the bloodstream, causing septic shock (very low blood pressure which damages the brain, kidney, and heart).
Parasites
A variety of parasites can affect the lungs, generally entering the body through the skin or by being swallowed. They then travel to the lungs through the blood, where the combination of cell destruction and immune response disrupts oxygen transport.
Diagnosis
Patients with symptoms of CAP require evaluation. Diagnosis of pneumonia is made clinically, rather than on the basis of a particular test. Evaluation begins with a physical examination by a health provider, which may reveal fever, an increased respiratory rate (tachypnea), low blood pressure (hypotension), a fast heart rate (tachycardia) and changes in the amount of oxygen in the blood. Palpating the chest as it expands and tapping the chest wall to identify dull, non-resonant areas can identify stiffness and fluid, signs of CAP. Listening to the lungs with a stethoscope (auscultation) can also reveal signs associated with CAP. A lack of normal breath sounds or the presence of crackles can indicate fluid consolidation. Increased vibration of the chest when speaking, known as tactile fremitus, and increased volume of whispered speech during auscultation can also indicate the presence of fluid.
Several tests can identify the cause of CAP. Blood cultures can isolate bacteria or fungi in the bloodstream. Sputum Gram staining and culture can also reveal the causative microorganism. In severe cases, bronchoscopy can collect fluid for culture. Special tests, such as urinalysis, can be performed if an uncommon microorganism is suspected.
Chest X-rays and X-ray computed tomography (CT) can reveal areas of opacity (seen as white), indicating consolidation. CAP does not always appear on x-rays, sometimes because the disease is in its initial stages or involves a part of the lung not clearly visible on x-ray. In some cases, chest CT can reveal pneumonia not seen on x-rays. However, congestive heart failure or other types of lung damage can mimic CAP on x-ray.
When signs of pneumonia are discovered during evaluation, chest X-rays and examination of the blood and sputum for infectious microorganisms may be done to support a diagnosis of CAP. The diagnostic tools employed will depend on the severity of illness, local practices and concern about complications of the infection. All patients with CAP should have their blood oxygen monitored with pulse oximetry. In some cases, arterial blood gas analysis may be required to determine the amount of oxygen in the blood. A complete blood count (CBC) may reveal extra white blood cells, indicating infection.
Prevention
CAP may be prevented by treating underlying illnesses that increases its risk, by smoking cessation, and by vaccination. Vaccination against Haemophilus influenzae and Streptococcus pneumoniae in the first year of life has been protective against childhood CAP. A vaccine against Streptococcus pneumoniae, available for adults, is recommended for healthy individuals over 65 and all adults with COPD, heart failure, diabetes mellitus, cirrhosis, alcoholism, cerebrospinal fluid leaks or who have had a splenectomy. Re-vaccination may be required after five or ten years.
Patients who have been vaccinated against Streptococcus pneumoniae, health professionals, nursing-home residents and pregnant women should be vaccinated annually against influenza. During an outbreak, drugs such as amantadine, rimantadine, zanamivir and oseltamivir have been demonstrated to prevent influenza.
Treatment

 Chest X-rays of a CAP patient before (left) and after treatment
Chest X-rays of a CAP patient before (left) and after treatment
CAP is treated with an antibiotic that kills the infecting microorganism; treatment also aims at managing complications. If the causative microorganism is unidentified, which is often the case, the laboratory identifies the most effective antibiotic; this may take several days.
Health professionals consider a person's risk factors for various organisms when choosing an initial antibiotic. Additional consideration is given to the treatment setting; most patients are cured by oral medication, while others must be hospitalized for intravenous therapy or intensive care. Current treatment guidelines recommend a beta-lactam, like amoxicillin, and a macrolide, like azithromycin or clarithromycin, or a quinolone, such as levofloxacin. Doxycycline is the antibiotic of choice in the UK for atypical bacteria, due to increased Clostridioides difficile infection in hospital patients linked to the increased use of clarithromycin.
Ceftriaxone and azithromycin are often used to treat community-acquired pneumonia, which usually presents with a few days of cough, fever, and shortness of breath. Chest x-ray typically reveals a lobar infiltrate (rather than diffuse).
Newborns
Most newborn infants with CAP are hospitalized, receiving IV ampicillin and gentamicin for at least ten days to treat the common causative agents Streptococcus agalactiae, Listeria monocytogenes and Escherichia coli. To treat the herpes simplex virus, IV acyclovir is administered for 21 days.
Children
Treatment of CAP in children depends on the child's age and the severity of illness. Children under five are not usually treated for atypical bacteria. If hospitalization is not required, a seven-day course of amoxicillin is often prescribed, with co-trimaxazole as an alternative when there is allergy to penicillins. Further studies are needed to confirm the efficacy of newer antibiotics. With the increase in drug-resistant Streptococcus pneumoniae, antibiotics such as cefpodoxime may become more popular. Hospitalized children receive intravenous ampicillin, ceftriaxone or cefotaxime, and a recent study found that a three-day course of antibiotics seems sufficient for most mild-to-moderate CAP in children.
Adults
In 2001 the American Thoracic Society, drawing on the work of the British and Canadian Thoracic Societies, established guidelines for the management of adult CAP by dividing patients into four categories based on common organisms:
- Healthy outpatients without risk factors: This group (the largest) is composed of otherwise-healthy patients without risk factors for DRSP, enteric gram-negative bacteria, Pseudomonas or other, less common, causes of CAP. Primary microorganisms are viruses, atypical bacteria, penicillin-sensitive Streptococcus pneumoniae and Haemophilus influenzae. Recommended drugs are macrolide antibiotics, such as azithromycin or clarithromycin, for seven to ten days. A shorter course of these antibiotics has been investigated, however, there is not sufficient evidence to make recommendations.
- Outpatients with underlying illness or risk factors: Although this group does not require hospitalization, they have underlying health problems such as emphysema or heart failure or are at risk for DRSP or enteric gram-negative bacteria. They may be treated with a quinolone active against Streptococcus pneumoniae (such as levofloxacin) or a β-lactam antibiotic (such as cefpodoxime, cefuroxime, amoxicillin or amoxicillin/clavulanic acid) and a macrolide antibiotic, such as azithromycin or clarithromycin, for seven to ten days.
- Hospitalized patients without risk for Pseudomonas: This group requires intravenous antibiotics, with a quinolone active against Streptococcus pneumoniae (such as levofloxacin), a β-lactam antibiotic (such as cefotaxime, ceftriaxone, ampicillin/sulbactam or high-dose ampicillin plus a macrolide antibiotic (such as azithromycin or clarithromycin) for seven to ten days.
- Intensive-care patients at risk for Pseudomonas aeruginosa: These patients require antibiotics targeting this difficult-to-eradicate bacterium. One regimen is an intravenous antipseudomonal beta-lactam such as cefepime, imipenem, meropenem or piperacillin/tazobactam, plus an IV antipseudomonal fluoroquinolone such as levofloxacin. Another is an IV antipseudomonal beta-lactam such as cefepime, imipenem, meropenem or piperacillin/tazobactam, plus an aminoglycoside such as gentamicin or tobramycin, plus a macrolide (such as azithromycin) or a nonpseudomonal fluoroquinolone such as ciprofloxacin.
For mild-to-moderate CAP, shorter courses of antibiotics (3–7 days) seem to be sufficient.
Some patients with CAP will be at increased risk of death despite antimicrobial treatment. A key reason for this is the host's exaggerated inflammatory response. There is a tension between controlling the infection on one hand and minimizing damage to other tissues on the other. Some recent research focuses on immunomodulatory therapy that can modulate the immune response in order to reduce injury to the lung and other affected organs such as the heart. Although the evidence for these agents has not resulted in their routine use, their potential benefits are promising.
Hospitalization
Some CAP patients require intensive care, with clinical prediction rules such as the pneumonia severity index and CURB-65 guiding the decision whether or not to hospitalize. Factors increasing the need for hospitalization include:
- Age greater than 65
- Underlying chronic illnesses
- Respiratory rate greater than 30 per minute
- Systolic blood pressure less than 90 mmHg
- Heart rate greater than 125 per minute
- Temperature below 35 or over 40 °C
- Confusion
- Evidence of infection outside the lung
Laboratory results indicating hospitalization include:
- Arterial oxygen tension less than 60 mm Hg
- Carbon dioxide over 50 mmHg or pH under 7.35 while breathing room air
- Hematocrit under 30 percent
- Creatinine over 1.2 mg/dl or blood urea nitrogen over 20 mg/dl
- White-blood-cell count under 4 × 10^9/L or over 30 × 10^9/L
- Neutrophil count under 1 x 10^9/L
X-ray findings indicating hospitalization include:
- Involvement of more than one lobe of the lung
- Presence of a cavity
- Pleural effusion
Prognosis
The CAP outpatient mortality rate is less than one percent, with fever typically responding within the first two days of therapy, and other symptoms abating in the first week. However, X-rays may remain abnormal for at least a month. Hospitalized patients have an average mortality rate of 12 percent, with the rate rising to 40 percent for patients with bloodstream infections or those who require intensive care. Factors increasing mortality are identical to those indicating hospitalization.
When CAP does not respond to treatment, this may indicate a previously unknown health problem, a treatment complication, inappropriate antibiotics for the causative organism, a previously unsuspected microorganism (such as tuberculosis) or a condition mimicking CAP (such as granuloma with polyangiitis). Additional tests include X-ray computed tomography, bronchoscopy or lung biopsy.
Epidemiology
CAP is common worldwide, and is a major cause of death in all age groups. In children, most deaths (over two million a year) occur in the newborn period. According to a World Health Organization estimate, one in three newborn deaths result from pneumonia. Mortality decreases with age until late adulthood, with the elderly at risk for CAP and its associated mortality.
More CAP cases occur during the winter than at other times of the year. CAP is more common in males than females, and more common in black people than Caucasians. Patients with underlying illnesses (such as Alzheimer's disease, cystic fibrosis, COPD, tobacco smoking, alcoholism or immune-system problems) have an increased risk of developing pneumonia.
See also
References
- "Pneumonia Causes – Mayo Clinic". www.mayoclinic.org. Retrieved 2015-05-18.
- "Pneumonia Treatments and drugs – Mayo Clinic". www.mayoclinic.org. Retrieved 2015-05-18.
- José RJ, Brown JS (2017). "Adult pneumococcal vaccination". Current Opinion in Pulmonary Medicine. 23 (3): 225–230. doi:10.1097/MCP.0000000000000369. PMID 28198725. S2CID 4700975.
- "Pneumonia Prevention – Mayo Clinic". www.mayoclinic.org. Retrieved 2015-05-18.
- Metlay JP, Schulz R, Li YH, et al. (July 1997). "Influence of age on symptoms at presentation in patients with community-acquired pneumonia". Archives of Internal Medicine. 157 (13): 1453–9. doi:10.1001/archinte.157.13.1453. PMID 9224224.
- "What is pneumonia? What causes pneumonia?". Retrieved 2015-05-18.
- Webber S, Wilkinson AR, Lindsell D, Hope PL, Dobson SR, Isaacs D (February 1990). "Neonatal pneumonia". Archives of Disease in Childhood. 65 (2): 207–11. doi:10.1136/adc.65.2.207. PMC 1792235. PMID 2107797.
- Abzug MJ, Beam AC, Gyorkos EA, Levin MJ (December 1990). "Viral pneumonia in the first month of life". The Pediatric Infectious Disease Journal. 9 (12): 881–5. doi:10.1097/00006454-199012000-00005. PMID 2177540. S2CID 2653523.
- Wubbel L, Muniz L, Ahmed A, et al. (February 1999). "Etiology and treatment of community-acquired pneumonia in ambulatory children". The Pediatric Infectious Disease Journal. 18 (2): 98–104. doi:10.1097/00006454-199902000-00004. PMID 10048679.
- Mundy LM, Auwaerter PG, Oldach D, et al. (October 1995). "Community-acquired pneumonia: impact of immune status". American Journal of Respiratory and Critical Care Medicine. 152 (4 Pt 1): 1309–15. doi:10.1164/ajrccm.152.4.7551387. PMID 7551387.
- Mandell L (2006). Respiratory infections. CRC Press. p. 338.
- de Roux A, Marcos MA, Garcia E, et al. (April 2004). "Viral community-acquired pneumonia in nonimmunocompromised adults". Chest. 125 (4): 1343–51. doi:10.1378/chest.125.4.1343. PMID 15078744.
- ^ Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Musher DM, Niederman MS, Torres A, Whitney CG (2007-03-01). "Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults". Clinical Infectious Diseases. 44 (Supplement 2). Oxford University Press (OUP): S27 – S72. doi:10.1086/511159. ISSN 1058-4838. PMC 7107997. PMID 17278083.
- Metlay JP, Kapoor WN, Fine MJ (November 1997). "Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination". JAMA. 278 (17): 1440–5. doi:10.1001/jama.278.17.1440. PMID 9356004.
- Syrjälä H, Broas M, Suramo I, Ojala A, Lähde S (August 1998). "High-resolution computed tomography for the diagnosis of community-acquired pneumonia". Clinical Infectious Diseases. 27 (2): 358–63. doi:10.1086/514675. PMID 9709887.
- Butler JC, Breiman RF, Campbell JF, Lipman HB, Broome CV, Facklam RR (October 1993). "Pneumococcal polysaccharide vaccine efficacy. An evaluation of current recommendations". JAMA. 270 (15): 1826–31. doi:10.1001/jama.270.15.1826. PMID 8411526.
- Centers for Disease Control and Prevention (April 1999). "Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP)". MMWR Recomm Rep. 48 (RR–4): 1–28. PMID 10366138.
- Hayden FG, Atmar RL, Schilling M, et al. (October 1999). "Use of the selective oral neuraminidase inhibitor oseltamivir to prevent influenza". The New England Journal of Medicine. 341 (18): 1336–43. doi:10.1056/NEJM199910283411802. PMID 10536125.
- "UWorld | Test Prep for NCLEX, SAT, ACT, MCAT, USMLE & More!". UWorld Test Prep. Retrieved 2021-01-25.
- ^ Lodha R, Kabra SK, Pandey RM (4 June 2013). "Antibiotics for community-acquired pneumonia in children". The Cochrane Database of Systematic Reviews. 2013 (6): CD004874. doi:10.1002/14651858.CD004874.pub4. PMC 7017636. PMID 23733365.
- Bradley JS (June 2002). "Management of community-acquired pediatric pneumonia in an era of increasing antibiotic resistance and conjugate vaccines". The Pediatric Infectious Disease Journal. 21 (6): 592–8, discussion 613–4. doi:10.1097/00006454-200206000-00035. PMID 12182396. S2CID 20412452.
- ^ Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, Grammatikos AP, Athanassa Z, Falagas ME (2008). "Short- versus long-course antibacterial therapy for community-acquired pneumonia : a meta-analysis". Drugs. 68 (13): 1841–54. doi:10.2165/00003495-200868130-00004. PMID 18729535.
- Niederman MS, Mandell LA, Anzueto A, et al. (June 2001). "Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention". American Journal of Respiratory and Critical Care Medicine. 163 (7): 1730–54. doi:10.1164/ajrccm.163.7.at1010. PMID 11401897.
- Li JZ, Winston LG, Moore DH, Bent S (September 2007). "Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis". The American Journal of Medicine. 120 (9): 783–90. doi:10.1016/j.amjmed.2007.04.023. PMID 17765048.
- López-Alcalde J, Rodriguez-Barrientos R, Redondo-Sánchez J, Muñoz-Gutiérrez J, Molero García JM, Rodríguez-Fernández C, Heras-Mosteiro J, Marin-Cañada J, Casanova-Colominas J, Azcoaga-Lorenzo A, Hernandez Santiago V, Gómez-García M (6 September 2018). "Short-course versus long-course therapy of the same antibiotic for community-acquired pneumonia in adolescent and adult outpatients". Cochrane Database of Systematic Reviews. 2018 (9): CD009070. doi:10.1002/14651858.CD009070.pub2. hdl:10023/18430. PMC 6513237. PMID 30188565.
- Vardakas KZ, Siempos II, Grammatikos A, Athanassa Z, Korbila IP, Falagas ME (December 2008). "Respiratory fluoroquinolones for the treatment of community-acquired pneumonia: a meta-analysis of randomized controlled trials". CMAJ. 179 (12): 1269–77. doi:10.1503/cmaj.080358. PMC 2585120. PMID 19047608.
- Woods DR, José RJ. Current and emerging evidence for immunomodulatory therapy in community-acquired pneumonia. Ann Res Hosp 2017;1:33 http://arh.amegroups.com/article/view/3806
- Fine MJ, Auble TE, Yealy DM, et al. (January 1997). "A prediction rule to identify low-risk patients with community-acquired pneumonia". The New England Journal of Medicine. 336 (4): 243–50. doi:10.1056/NEJM199701233360402. PMID 8995086.
- Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG (March 1987). "Prospective study of the aetiology and outcome of pneumonia in the community". Lancet. 1 (8534): 671–4. doi:10.1016/S0140-6736(87)90430-2. PMID 2882091. S2CID 34844819.
- Garenne M, Ronsmans C, Campbell H (1992). "The magnitude of mortality from acute respiratory infections in children under 5 years in developing countries". World Health Statistics Quarterly. 45 (2–3): 180–91. PMID 1462653.
- Ramirez JA, Wiemken TL, Peyrani P, Arnold FW, Kelley R, Mattingly WA, Nakamatsu R, Pena S, Guinn BE (2017-07-28). "Adults Hospitalized With Pneumonia in the United States: Incidence, Epidemiology, and Mortality". Clinical Infectious Diseases. 65 (11): 1806–1812. doi:10.1093/cid/cix647. ISSN 1058-4838. PMID 29020164.
- Almirall J, Bolíbar I, Balanzó X, González CA (February 1999). "Risk factors for community-acquired pneumonia in adults: a population-based case-control study". The European Respiratory Journal. 13 (2): 349–55. doi:10.1183/09031936.99.13234999. PMID 10065680.
- Mandell LA, Wunderink RG, Anzueto A, et al. (March 2007). "Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults". Clinical Infectious Diseases. 44 (Suppl 2): S27–72. doi:10.1086/511159. PMC 7107997. PMID 17278083.
External links
| Diseases of the respiratory system | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Upper RT (including URTIs, common cold) |
| ||||||||||||||||||||||
| Lower RT/ lung disease (including LRTIs) |
| ||||||||||||||||||||||
| Pleural cavity/ mediastinum |
| ||||||||||||||||||||||
| Other/general | |||||||||||||||||||||||
| Pneumonia | |
|---|---|
| Infectious pneumonias | |
| Pneumonias caused by infectious or noninfectious agents | |
| Noninfectious pneumonia | |