| Revision as of 07:58, 28 October 2011 editBeetstra (talk | contribs)Edit filter managers, Administrators172,031 edits Script assisted update of identifiers for the Chem/Drugbox validation project (updated: 'DrugBank', 'ChEMBL').← Previous edit | Latest revision as of 20:12, 14 November 2024 edit undoCitation bot (talk | contribs)Bots5,391,876 edits Altered volume. Added issue. | Use this bot. Report bugs. | Suggested by Whoop whoop pull up | Category:Thioxanthene antipsychotics | #UCB_Category 5/5 | ||
| (252 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Typical antipsychotic drug of the thioxanthene class}} | |||
| {{cs1 config|name-list-style=vanc}} | |||
| {{Drugbox | {{Drugbox | ||
| | Verifiedfields = changed | | Verifiedfields = changed | ||
| | Watchedfields = changed | |||
| | verifiedrevid = 407230655 | |||
| | verifiedrevid = 457784839 | |||
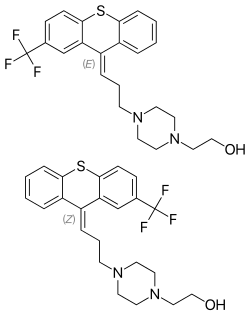
| | IUPAC_name = (''EZ'')-2-propyl]piperazin-1-yl]ethanol | |||
| | IUPAC_name = ''(EZ)''-2-propyl]piperazin-1-yl]ethanol | |||
| | image = E-Z-Isomers of Flupentixol.png | |||
| | image = Flupentixol structure.svg | |||
| | width = 250 | |||
| <!--Clinical data--> | <!--Clinical data--> | ||
| | tradename = | | tradename = Depixol, Fluanxol | ||
| | Drugs.com = {{drugs.com|CONS|flupentixol}} | | Drugs.com = {{drugs.com|CONS|flupentixol}} | ||
| | |
| pregnancy_AU = C | ||
| | legal_AU = S4 | |||
| | legal_BR = C1 | |||
| | legal_BR_comment = <ref>{{Cite web |author=Anvisa |author-link=Brazilian Health Regulatory Agency |date=2023-03-31 |title=RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial |trans-title=Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control|url=https://www.in.gov.br/en/web/dou/-/resolucao-rdc-n-784-de-31-de-marco-de-2023-474904992 |url-status=live |archive-url=https://web.archive.org/web/20230803143925/https://www.in.gov.br/en/web/dou/-/resolucao-rdc-n-784-de-31-de-marco-de-2023-474904992 |archive-date=2023-08-03 |access-date=2023-08-16 |publisher=] |language=pt-BR |publication-date=2023-04-04}}</ref> | |||
| | legal_UK = POM | |||
| | legal_CA = Rx-only | |||
| | legal_status = Rx-only | | legal_status = Rx-only | ||
| | routes_of_administration = Oral, IM | | routes_of_administration = Oral, ] (including a ]) | ||
| | class = ] | |||
| <!--Pharmacokinetic data--> | <!--Pharmacokinetic data--> | ||
| | bioavailability = | | bioavailability = 40–55% (oral)<ref name = EMC/> | ||
| | protein_bound = |
| protein_bound = | ||
| | metabolism = Gut wall, ]<ref>{{cite journal | vauthors = Jann MW, Ereshefsky L, Saklad SR | title = Clinical pharmacokinetics of the depot antipsychotics | journal = Clinical Pharmacokinetics | volume = 10 | issue = 4 | pages = 315–333 | date = July–August 1985 | pmid = 2864156 | doi = 10.2165/00003088-198510040-00003 | s2cid = 12848774 }}</ref> | |||
| | metabolism = | |||
| | elimination_half-life = 35 hours<ref name = EMC>{{cite web|title=Depixol Tablets 3mg - Summary of Product Characteristics (SPC)|date=27 December 2012|work=electronic Medicines Compendium|publisher = Lundbeck Ltd|access-date=20 October 2013|url=http://www.medicines.org.uk/emc/medicine/1076/SPC/Depixol+Tablets+3mg/}}</ref> | |||
| | elimination_half-life = 19-39 hours | |||
| | excretion = ] (negligible)<ref>{{cite journal | vauthors = Balant-Gorgia AE, Balant L | title = Antipsychotic drugs. Clinical pharmacokinetics of potential candidates for plasma concentration monitoring | journal = Clinical Pharmacokinetics | volume = 13 | issue = 2 | pages = 65–90 | date = August 1987 | pmid = 2887326 | doi = 10.2165/00003088-198713020-00001 | s2cid = 24707620 }}</ref> | |||
| | excretion = | |||
| <!--Identifiers--> | <!--Identifiers--> | ||
| | |
| CAS_number_Ref = {{cascite|correct|CAS}} | ||
| | CAS_number_Ref = {{cascite|correct|??}} | |||
| | CAS_number = 2709-56-0 | | CAS_number = 2709-56-0 | ||
| | ATC_prefix = N05 | | ATC_prefix = N05 | ||
| | ATC_suffix = AF01 | | ATC_suffix = AF01 | ||
| | PubChem = 5281881 | | PubChem = 5281881 | ||
| | IUPHAR_ligand = 968 | |||
| | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| | DrugBank_Ref = {{drugbankcite|changed|drugbank}} | |||
| | DrugBank = <!-- blanked - oldvalue: APRD00388 --> | |||
| | DrugBank = DB00875 | |||
| | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | ||
| | ChemSpiderID = 4445173 | | ChemSpiderID = 4445173 | ||
| | UNII_Ref = {{fdacite| |
| UNII_Ref = {{fdacite|changed|FDA}} | ||
| | UNII = |
| UNII = 21HMQ851IS | ||
| | KEGG_Ref = {{keggcite|correct|kegg}} | | KEGG_Ref = {{keggcite|correct|kegg}} | ||
| | KEGG = D01044 | | KEGG = D01044 | ||
| | ChEMBL_Ref = {{ebicite|changed|EBI}} | | ChEMBL_Ref = {{ebicite|changed|EBI}} | ||
| | ChEMBL = |
| ChEMBL = 42055 | ||
| | chemical_formula = C<sub>23</sub>H<sub>25</sub>F<sub>3</sub>N<sub>2</sub>OS | |||
| <!--Chemical data--> | |||
| | molecular_weight = 434.5219 g/mol | |||
| | C=23 | H=25 | F=3 | N=2 | O=1 | S=1 | |||
| | smiles = FC(F)(F)c2cc1C(\c3c(Sc1cc2)cccc3)=C/CCN4CCN(CCO)CC4 | | smiles = FC(F)(F)c2cc1C(\c3c(Sc1cc2)cccc3)=C/CCN4CCN(CCO)CC4 | ||
| | InChI = 1/C23H25F3N2OS/c24-23(25,26)17-7-8-22-20(16-17)18(19-4-1-2-6-21(19)30-22)5-3-9-27-10-12-28(13-11-27)14-15-29/h1-2,4-8,16,29H,3,9-15H2/b18-5- | |||
| | InChIKey = NJMYODHXAKYRHW-DVZOWYKEBC | |||
| | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChI = 1S/C23H25F3N2OS/c24-23(25,26)17-7-8-22-20(16-17)18(19-4-1-2-6-21(19)30-22)5-3-9-27-10-12-28(13-11-27)14-15-29/h1-2,4-8,16,29H,3,9-15H2/b18-5- | | StdInChI = 1S/C23H25F3N2OS/c24-23(25,26)17-7-8-22-20(16-17)18(19-4-1-2-6-21(19)30-22)5-3-9-27-10-12-28(13-11-27)14-15-29/h1-2,4-8,16,29H,3,9-15H2/b18-5- | ||
| Line 48: | Line 56: | ||
| }} | }} | ||
| '''Flupentixol''' (]), also known as '''flupenthixol''' (former ]), marketed under brand names such as '''Depixol''' and '''Fluanxol''' |
'''Flupentixol''' (]), also known as '''flupenthixol''' (former ]), marketed under brand names such as '''Depixol''' and '''Fluanxol''' is a ] ] of the ] class. It was introduced in 1965 by ]. In addition to single drug preparations, it is also available as ]—a ] containing both ] (a ]) and flupentixol (marketed as Deanxit). | ||
| Flupentixol is not approved for use in the United States. It is, however, approved for use in the ],<ref name="BNF">{{cite book | isbn = 978-0-85711-084-8 | title = British National Formulary (BNF) | last1 = Joint Formulary Committee | year = 2013 | publisher = Pharmaceutical Press | location = London, UK | edition = 65 | url-access = registration | url = https://archive.org/details/bnf65britishnati0000unse }}</ref> ],<ref name="AMH">{{cite book | editor = Rossi, S | isbn = 978-0-9805790-9-3 | title = Australian Medicines Handbook | place = Adelaide | publisher = The Australian Medicines Handbook Unit Trust | year = 2013 | edition = 2013 }}</ref> ], ],<ref>{{cite web|title=Fluanxol® (flupentixol) Tablets Registration Certificate|url=http://grls.rosminzdrav.ru/Grls_View.aspx?idReg=5644&isOld=1&t=|publisher=Russian State Register of Medicinal Products|access-date=29 July 2014}}</ref> ], ], ], ], ], and various other countries. | |||
| == |
== Medical uses == | ||
| Flupentixol's main use is as a long-acting injection given once in every two or three weeks to individuals with ] who have poor compliance with medication and have frequent relapses of illness, though it is also commonly given as a tablet. There is little formal evidence to support its use for this indication but it has been in use for over fifty years.<ref name = BNF/><ref>{{cite journal | vauthors = Shen X, Xia J, Adams CE | title = Flupenthixol versus placebo for schizophrenia | journal = The Cochrane Database of Systematic Reviews | volume = 2012 | pages = CD009777 | date = November 2012 | issue = 11 | pmid = 23152280 | doi = 10.1002/14651858.CD009777.pub2 | editor1-last = Shen | editor1-first = Xiaohong | pmc = 11531908 }}</ref> | |||
| Flupentixol is also used in low doses as an ].<ref name = BNF/><ref name="pmid7291129">{{cite journal | vauthors = Robertson MM, Trimble MR | title = The antidepressant action of flupenthixol | journal = The Practitioner | volume = 225 | issue = 1355 | pages = 761–763 | date = May 1981 | pmid = 7291129 }}</ref><ref name="pmid6674820">{{cite journal | vauthors = Pöldinger W, Sieberns S | title = Depression-inducing and antidepressive effects of neuroleptics. Experiences with flupenthixol and flupenthixol decanoate | journal = Neuropsychobiology | volume = 10 | issue = 2–3 | pages = 131–136 | year = 1983 | pmid = 6674820 | doi = 10.1159/000117999 }}</ref><ref name="pmid369298">{{cite journal | vauthors = Johnson DA | title = A double-blind comparison of flupenthixol, nortriptyline and diazepam in neurotic depression | journal = Acta Psychiatrica Scandinavica | volume = 59 | issue = 1 | pages = 1–8 | date = January 1979 | pmid = 369298 | doi = 10.1111/j.1600-0447.1979.tb06940.x | s2cid = 144717662 }}</ref><ref name="pmid773506">{{cite journal | vauthors = Young JP, Hughes WC, Lader MH | title = A controlled comparison of flupenthixol and amitriptyline in depressed outpatients | journal = British Medical Journal | volume = 1 | issue = 6018 | pages = 1116–1118 | date = May 1976 | pmid = 773506 | pmc = 1639983 | doi = 10.1136/bmj.1.6018.1116 }}</ref><ref name="pmid961463">{{cite journal | vauthors = Fujiwara J, Ishino H, Baba O, Hanaoka M, Sasaki K | title = Effect of flupenthixol on depression with special reference to combination use with tricyclic antidepressants. An uncontrolled pilot study with 45 patients | journal = Acta Psychiatrica Scandinavica | volume = 54 | issue = 2 | pages = 99–105 | date = August 1976 | pmid = 961463 | doi = 10.1111/j.1600-0447.1976.tb00101.x | s2cid = 25364795 }}</ref><ref name="pmid7093597">{{cite journal | vauthors = Tam W, Young JP, John G, Lader MH | title = A controlled comparison of flupenthixol decanoate injections and oral amitriptyline in depressed out-patients | journal = The British Journal of Psychiatry | volume = 140 | issue = 3 | pages = 287–291 | date = March 1982 | pmid = 7093597 | doi = 10.1192/bjp.140.3.287 | s2cid = 30537435 }}</ref> There is tentative evidence that it reduces the rate of deliberate ], among those who self-harm repeatedly.<ref>{{cite journal | vauthors = Hawton K, Witt KG, Taylor Salisbury TL, Arensman E, Gunnell D, Hazell P, Townsend E, van Heeringen K | display-authors = 6 | title = Pharmacological interventions for self-harm in adults | journal = The Cochrane Database of Systematic Reviews | volume = 2015 | issue = 7 | pages = CD011777 | date = July 2015 | pmid = 26147958 | pmc = 8637297 | doi = 10.1002/14651858.CD011777 | hdl-access = free | hdl = 10536/DRO/DU:30080508 }}</ref> | |||
| Flupentixol's main use is as a long-acting injection given two or three times weekly to individuals with ] who have poor compliance with medication and suffer frequent relapses of illness. | |||
| == Adverse effects == | |||
| Flupentixol is also used in low doses as an ].<ref name="pmid7291129">{{cite journal | author = Robertson MM, Trimble MR | title = The antidepressant action of flupenthixol | journal = The Practitioner | volume = 225 | issue = 1355 | pages = 761–3 | year = 1981 | month = May | pmid = 7291129 | doi = | url = }}</ref><ref name="pmid6674820">{{cite journal | author = Pöldinger W, Sieberns S | title = Depression-inducing and antidepressive effects of neuroleptics. Experiences with flupenthixol and flupenthixol decanoate | journal = Neuropsychobiology | volume = 10 | issue = 2-3 | pages = 131–6 | year = 1983 | pmid = 6674820 | doi = | url = }}</ref><ref name="pmid369298">{{cite journal | author = Johnson DA | title = A double-blind comparison of flupenthixol, nortriptyline and diazepam in neurotic depression | journal = Acta Psychiatrica Scandinavica | volume = 59 | issue = 1 | pages = 1–8 | year = 1979 | month = January | pmid = 369298 | doi = | url = }}</ref><ref name="pmid773506">{{cite journal | author = Young JP, Hughes WC, Lader MH | title = A controlled comparison of flupenthixol and amitriptyline in depressed outpatients | journal = British Medical Journal | volume = 1 | issue = 6018 | pages = 1116–8 | year = 1976 | month = May | pmid = 773506 | pmc = 1639983 | doi = | url = }}</ref><ref name="pmid961463">{{cite journal | author = Fujiwara J, Ishino H, Baba O, Hanaoka M, Sasaki K | title = Effect of flupenthixol on depression with special reference to combination use with tricyclic antidepressants. An uncontrolled pilot study with 45 patients | journal = Acta Psychiatrica Scandinavica | volume = 54 | issue = 2 | pages = 99–105 | year = 1976 | month = August | pmid = 961463 | doi = | url = }}</ref><ref name="pmid7093597">{{cite journal | author = Tam W, Young JP, John G, Lader MH | title = A controlled comparison of flupenthixol decanoate injections and oral amitriptyline in depressed out-patients | journal = The British Journal of Psychiatry : the Journal of Mental Science | volume = 140 | issue = | pages = 287–91 | year = 1982 | month = March | pmid = 7093597 | doi = | url = }}</ref> | |||
| '''Adverse effect incidence'''<ref name = EMC/><ref name = BNF/><ref name = AMH/><ref>{{cite journal | vauthors = Bostwick JR, Guthrie SK, Ellingrod VL | title = Antipsychotic-induced hyperprolactinemia | journal = Pharmacotherapy | volume = 29 | issue = 1 | pages = 64–73 | date = January 2009 | pmid = 19113797 | doi = 10.1592/phco.29.1.64 | hdl-access = free | s2cid = 25981099 | hdl = 2027.42/90238 }}</ref><ref name = FLUANXOL>{{cite web|title=FLUANXOL® DEPOT FLUANXOL® CONCENTRATED DEPOT|work = TGA eBusiness Services|publisher = Lundbeck Australia Pty Ltd|date=28 June 2013|access-date=20 October 2013|url=https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05706-3}}</ref> | |||
| ;Common (>1% incidence) adverse effects include: | |||
| * Extrapyramidal side effects such as: (which ''usually'' become apparent soon after therapy is begun or soon after an increase in dose is made) | |||
| ** ] | |||
| ** ] | |||
| ** ] | |||
| ** ] | |||
| ** Tremor | |||
| ** ] | |||
| ** ] | |||
| * Dry mouth | |||
| * Constipation | |||
| * Hypersalivation – excessive salivation | |||
| * Blurred vision | |||
| * Diaphoresis – excessive sweating | |||
| * Nausea | |||
| * Dizziness | |||
| * ] | |||
| * Restlessness | |||
| * Insomnia | |||
| * Overactivity | |||
| * Headache | |||
| * Nervousness | |||
| * ] | |||
| * ] | |||
| * ] and its complications such as: (''acutely'') | |||
| ** Sexual dysfunction | |||
| ** Amenorrhea – cessation of menstrual cycles | |||
| ** Gynecomastia – enlargement of breast tissue in males | |||
| ** Galactorrhea – the expulsion of breast milk that's not related to breastfeeding or pregnancy | |||
| : and if the hyperprolactinemia persists ''chronically'', the following adverse effects may be seen: | |||
| :* Reduced bone mineral density leading to ] (brittle bones) | |||
| :* Infertility | |||
| * Dyspepsia – indigestion | |||
| * Abdominal pain | |||
| * Flatulence | |||
| * Nasal congestion | |||
| * Polyuria – passing more urine than usual | |||
| ;Uncommon (0.1–1% incidence) adverse effects include: | |||
| * Fainting | |||
| * Palpitations | |||
| ;Rare (<0.1% incidence) adverse effects include: | |||
| * Blood dyscrasias (abnormalities in the cell composition of blood), such as: | |||
| ** ] – a drop in white blood cell counts that leaves one open to potentially life-threatening infections | |||
| ** ] – a drop in the number of ] (white blood cells that specifically fight bacteria) in one's blood | |||
| ** ] – a less severe drop in white blood cell counts than agranulocytosis | |||
| ** ] – a drop in the number of platelets in the blood. Platelets are responsible for blood clotting and hence this leads to an increased risk of bruising and other bleeds | |||
| * ] – a potentially fatal condition that appear to result from central ] blockade. The symptoms include: | |||
| ** ] | |||
| ** Muscle rigidity | |||
| ** ] | |||
| ** Autonomic instability (e.g., ], diarrhea, diaphoresis, etc.) | |||
| ** Mental status changes (e.g., coma, agitation, anxiety, confusion, etc.) | |||
| ;Unknown incidence adverse effects include: | |||
| * Jaundice | |||
| * Abnormal liver function test results | |||
| * ] – an often incurable movement disorder that usually results from years of continuous treatment with antipsychotic drugs, especially ] like flupenthixol. It presents with repetitive, involuntary, purposeless and slow movements; TD can be triggered by a fast dose reduction in any antipsychotic. | |||
| * Hypotension | |||
| * Confusional state | |||
| * Seizures | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * Hot flush | |||
| * Anergia | |||
| * Appetite changes | |||
| * Weight changes | |||
| * Hyperglycemia – high blood glucose (sugar) levels | |||
| * Abnormal glucose tolerance | |||
| * Pruritus – itchiness | |||
| * Rash | |||
| * Dermatitis | |||
| * Photosensitivity – sensitivity to light | |||
| * Oculogyric crisis | |||
| * Accommodation disorder | |||
| * Sleep disorder | |||
| * Impaired concentration | |||
| * Tachycardia | |||
| * ] prolongation – an abnormality in the ] that can lead to potentially fatal changes in heart rhythm (only in ] or <10 ms increases in QTc)<ref>{{Cite web|title=Guidelines for the Management of QTc Prolongation in Adults Prescribed Antipsychotics|url=https://www.england.nhs.uk/north/wp-content/uploads/sites/5/2018/12/QTc-flow-diagram-with-medications-final-Dec-17-A3-with-logos.pdf |website=nhs.uk}}</ref><ref>{{cite journal | vauthors = Lambiase PD, de Bono JP, Schilling RJ, Lowe M, Turley A, Slade A, Collinson J, Rajappan K, Harris S, Collison J, Carpenter V, Daw H, Hall A, Roberts E, Holding S, Paisey J, Sopher M, Wright I, Wiles B, Murgatroyd F, Taylor D | display-authors = 6 | title = British Heart Rhythm Society Clinical Practice Guidelines on the Management of Patients Developing QT Prolongation on Antipsychotic Medication | journal = Arrhythmia & Electrophysiology Review | volume = 8 | issue = 3 | pages = 161–165 | date = July 2019 | pmid = 31463053 | pmc = 6702465 | doi = 10.15420/aer.2019.8.3.G1 }}</ref> | |||
| * ] | |||
| * Miosis – constriction of the pupil of the eye | |||
| * Paralytic ] – paralysis of the bowel muscles leading to severe constipation, inability to pass wind, etc. | |||
| * Mydriasis | |||
| * ] | |||
| === Interactions === | |||
| It should not be used concomitantly with medications known to prolong the QTc interval (e.g., ]s, ], ], etc.) as this may lead to an increased risk of QTc interval prolongation.<ref name = " | |||
| FLUANXOL"/><ref name = EMC/> Neither should it be given concurrently with ] as it may increase the risk of lithium toxicity and ].<ref name = BNF/><ref name = AMH/><ref name = FLUANXOL/> It should not be given concurrently with other antipsychotics due to the potential for this to increase the risk of side effects, especially neurological side effects such as ].<ref name = BNF/><ref name = AMH/><ref name = FLUANXOL/> It should be avoided in patients on CNS depressants such as opioids, alcohol and barbiturates.<ref name = FLUANXOL/> | |||
| ===Contraindications=== | |||
| It should not be given in the following disease states:<ref name = EMC/><ref name = BNF/><ref name = AMH/><ref name = FLUANXOL/> | |||
| * ] | |||
| * Prolactin-dependent tumors such as pituitary ]s and ] | |||
| * ] | |||
| * Coma | |||
| * Circulatory collapse | |||
| * Subcortical brain damage | |||
| * ] | |||
| * Parkinson's disease | |||
| * ] | |||
| == Pharmacology == | == Pharmacology == | ||
| ===Pharmacodynamics=== | |||
| Flupentixol acts as an ] at various ] (]-]), ] (]), ] (]), and ] (]) ]s,<ref name="urlPDSP Database - UNC">{{cite web | url = http://pdsp.med.unc.edu/pdsp.php | title = PDSP Database - UNC}}</ref> without affecting the ]s.<ref name="pmid7052344">{{cite journal | author = Golds PR, Przyslo FR, Strange PG | title = The binding of some antidepressant drugs to brain muscarinic acetylcholine receptors | journal = British Journal of Pharmacology | volume = 68 | issue = 3 | pages = 541–9 | year = 1980 | month = March | pmid = 7052344 | pmc = 2044199 | doi = | url = }}</ref> | |||
| '''Binding profile'''<ref>{{cite web|title=PDSP K<sub>i</sub> Database |work=Psychoactive Drug Screening Program (PDSP)|author1-link=Bryan Roth |author1=Roth, BL |author2=Driscol, J |url=http://pdsp.med.unc.edu/pdsp.php |publisher=University of North Carolina at Chapel Hill and the United States National Institute of Mental Health |date=12 January 2011 |access-date=20 October 2013 |url-status=dead |archive-url=https://web.archive.org/web/20131108013656/http://pdsp.med.unc.edu/pdsp.php |archive-date=8 November 2013 }}</ref> | |||
| {| class="wikitable" | |||
| Its antipsychotic effects are likely caused by D<sub>2</sub> and/or 5-HT<sub>2A</sub> antagonism, whereas its antidepressant effects at lower doses may be mediated by preferential D<sub>2</sub>/D<sub>3</sub> ] blockade, resulting in increased postsynaptic activation. | |||
| |- | |||
| ! Protein !! ''cis''-flupentixol !! ''trans''-flupentixol | |||
| |- | |||
| | ] || 8028 || — | |||
| |- | |||
| | ] || 87.5 (HFC) || — | |||
| |- | |||
| | ] || 102.2 (RC) || — | |||
| |- | |||
| | ]<ref name="pmid7052344">{{cite journal | vauthors = Golds PR, Przyslo FR, Strange PG | title = The binding of some antidepressant drugs to brain muscarinic acetylcholine receptors | journal = British Journal of Pharmacology | volume = 68 | issue = 3 | pages = 541–549 | date = March 1980 | pmid = 7052344 | pmc = 2044199 | doi = 10.1111/j.1476-5381.1980.tb14570.x }}</ref> || Neg. || Neg. | |||
| |- | |||
| | ] || 3.5 || 474 (MB) | |||
| |- | |||
| | ] || 0.35 || 120 | |||
| |- | |||
| | ] || 1.75 || 162.5 | |||
| |- | |||
| | ] || 66.3 || >1000 | |||
| |- | |||
| | ] || 0.86 || 5.73 | |||
| |} | |||
| '''Acronyms used:'''<br /> | |||
| == Side effects == | |||
| HFC – Human frontal cortex receptor<br /> | |||
| MB – Mouse brain receptor<br /> | |||
| RC – Cloned rat receptor | |||
| A study measuring the ] receptor occupancies of 13 schizophrenic patients treated with 5.7 ± 1.4 mg/day of flupentixol found 50-70% receptor occupancy for D2, 20 ± 5% for D1, and 20 ± 10% for 5-HT2A.<ref>{{cite journal | vauthors = Reimold M, Solbach C, Noda S, Schaefer JE, Bartels M, Beneke M, Machulla HJ, Bares R, Glaser T, Wormstall H | display-authors = 6 | title = Occupancy of dopamine D(1), D (2) and serotonin (2A) receptors in schizophrenic patients treated with flupentixol in comparison with risperidone and haloperidol | journal = Psychopharmacology | volume = 190 | issue = 2 | pages = 241–249 | date = February 2007 | pmid = 17111172 | doi = 10.1007/s00213-006-0611-0 | s2cid = 2231884 }}</ref> | |||
| The side effects of flupentixol are similar to most other typical antipsychotics, namely ] symptoms of ], ]s, and ] and ] effects like ] and ]. However, it lacks ] adverse effects. But seizures have been reported in some users, and long-term use may even inflict ] on some takers. | |||
| Its antipsychotic effects are predominantly a function of D<sub>2</sub> antagonism. | |||
| == See also == | |||
| * ] | |||
| * ] | |||
| Its antidepressant effects at lower doses are not well understood; however, it may be mediated by ] and/or preferentially binding to D<sub>2</sub> ]s at low doses, resulting in increased postsynaptic activation via higher dopamine levels. Flupentixol's demonstrated ability to raise dopamine levels in mice<ref>{{cite journal | vauthors = Hyttel J | title = Changes in dopamine synthesis rate in the supersensitivity phase after treatment with a single dose of neuroleptics | journal = Psychopharmacology | volume = 51 | issue = 2 | pages = 205–207 | date = January 1977 | pmid = 14353 | doi = 10.1007/BF00431742 | s2cid = 22801301 }}</ref> and flies<ref>{{cite journal | vauthors = Vickrey TL, Venton BJ | title = Drosophila Dopamine2-like receptors function as autoreceptors | journal = ACS Chemical Neuroscience | volume = 2 | issue = 12 | pages = 723–729 | date = December 2011 | pmid = 22308204 | pmc = 3269839 | doi = 10.1021/cn200057k | author2-link = Jill Venton }}</ref> lends credibility to the supposition of autoreceptor bias. Functional selectivity may be responsible through causing preferential autoreceptor binding or other means. The effective dosage guideline for an antipsychotic is very closely related to its receptor residency time (i.e., where drugs like aripiprazole take several minutes or more to disassociate from a receptor while drugs like quetiapine and clozapine—with guideline dosages in the hundreds of milligrams—take under 30s)<ref>{{cite journal | vauthors = Kapur S, Seeman P | title = Does fast dissociation from the dopamine d(2) receptor explain the action of atypical antipsychotics?: A new hypothesis | journal = The American Journal of Psychiatry | volume = 158 | issue = 3 | pages = 360–369 | date = March 2001 | pmid = 11229973 | doi = 10.1176/appi.ajp.158.3.360 }}</ref><ref>{{cite journal | vauthors = Kapur S, Seeman P | title = Antipsychotic agents differ in how fast they come off the dopamine D2 receptors. Implications for atypical antipsychotic action | journal = Journal of Psychiatry & Neuroscience | volume = 25 | issue = 2 | pages = 161–166 | date = March 2000 | pmid = 10740989 | pmc = 1408069 }}</ref><ref>{{cite journal | vauthors = Carboni L, Negri M, Michielin F, Bertani S, Fratte SD, Oliosi B, Cavanni P | title = Slow dissociation of partial agonists from the D₂ receptor is linked to reduced prolactin release | journal = The International Journal of Neuropsychopharmacology | volume = 15 | issue = 5 | pages = 645–656 | date = June 2012 | pmid = 21733233 | doi = 10.1017/S1461145711000824 | s2cid = 31885144 }}</ref> and long receptor residency time is strongly correlated with likehood of pronounced functional selectivity;<ref>{{cite journal | vauthors = Klein Herenbrink C, Sykes DA, Donthamsetti P, Canals M, Coudrat T, Shonberg J, Scammells PJ, Capuano B, Sexton PM, Charlton SJ, Javitch JA, Christopoulos A, Lane JR | display-authors = 6 | title = The role of kinetic context in apparent biased agonism at GPCRs | journal = Nature Communications | volume = 7 | pages = 10842 | date = February 2016 | pmid = 26905976 | pmc = 4770093 | doi = 10.1038/ncomms10842 | bibcode = 2016NatCo...710842K }}</ref> thus, with a maximum guideline dose of only 18 mg/day for schizophrenia, there is a significant possibility of this drug possessing unique signalling characteristics that permit counterintuitive dopaminergic action at low doses. | |||
| == References == | |||
| {{Reflist|2}} | |||
| ===Pharmacokinetics=== | |||
| {{Pharmacokinetics of long-acting injectable antipsychotics}} | |||
| ==History== | |||
| In March 1963 the Danish pharmaceutical company Lundbeck began research into further agents for schizophrenia, having already developed the thioxanthene derivatives clopenthixol and chlorprothixene. By 1965 the promising agent flupenthixol had been developed and trialled in two hospitals in Vienna by Austrian psychiatrist ].<ref>{{cite journal | vauthors = Gross H, Kaltenbäck E |doi=10.1111/j.1600-0447.1965.tb04969.x|title=Flupenthixol (Fluanxol®), ein Neues Neuroleptikum aus der Thiaxanthenreihe (Klinische Erfahrungen bei Einem Psychiatrischen Krankengut)|year=1965 |journal=Acta Psychiatrica Scandinavica|volume=41|pages=42–56|s2cid=145021607}}</ref> The long- acting decanoate preparation was synthesised in 1967 and introduced into hospital practice in Sweden in 1968, with a reduction in relapses among patients who were put on the depot.<ref>{{cite journal | vauthors = Gottfries CG, Green L | title = Flupenthixol decanoate--in treatment of out-patients | journal = Acta Psychiatrica Scandinavica. Supplementum | volume = 255 | pages = 15–24 | year = 1974 | pmid = 4533707 | doi = 10.1111/j.1600-0447.1974.tb08890.x | s2cid = 42657501 }}</ref> | |||
| == References == | |||
| {{reflist|30em}} | |||
| {{Antipsychotics}} | {{Antipsychotics}} | ||
| {{Antidepressants}} | {{Antidepressants}} | ||
| {{Anxiolytics}} | {{Anxiolytics}} | ||
| {{Navboxes | |||
| {{Adrenergics}} | |||
| | title = ] | |||
| {{Dopaminergics}} | |||
| | titlestyle = background:#ccccff | |||
| {{Histaminergics}} | |||
| | list1 = | |||
| {{Serotonergics}} | |||
| {{Adrenergic receptor modulators}} | |||
| {{Piperazines}} | |||
| {{Dopamine receptor modulators}} | |||
| {{Histamine receptor modulators}} | |||
| {{Serotonin receptor modulators}} | |||
| }} | |||
| {{Tricyclics}} | {{Tricyclics}} | ||
| ] | ] | ||
| ] | |||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 20:12, 14 November 2024
Typical antipsychotic drug of the thioxanthene classPharmaceutical compound
 | |
| Clinical data | |
|---|---|
| Trade names | Depixol, Fluanxol |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category |
|
| Routes of administration | Oral, IM (including a depot) |
| Drug class | Typical antipsychotic |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 40–55% (oral) |
| Metabolism | Gut wall, hepatic |
| Elimination half-life | 35 hours |
| Excretion | Renal (negligible) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.018.459 |
| Chemical and physical data | |
| Formula | C23H25F3N2OS |
| Molar mass | 434.52 g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (what is this?) (verify) | |
Flupentixol (INN), also known as flupenthixol (former BAN), marketed under brand names such as Depixol and Fluanxol is a typical antipsychotic drug of the thioxanthene class. It was introduced in 1965 by Lundbeck. In addition to single drug preparations, it is also available as flupentixol/melitracen—a combination product containing both melitracen (a tricyclic antidepressant) and flupentixol (marketed as Deanxit). Flupentixol is not approved for use in the United States. It is, however, approved for use in the UK, Australia, Canada, Russian Federation, South Africa, New Zealand, Philippines, Iran, Germany, and various other countries.
Medical uses
Flupentixol's main use is as a long-acting injection given once in every two or three weeks to individuals with schizophrenia who have poor compliance with medication and have frequent relapses of illness, though it is also commonly given as a tablet. There is little formal evidence to support its use for this indication but it has been in use for over fifty years.
Flupentixol is also used in low doses as an antidepressant. There is tentative evidence that it reduces the rate of deliberate self-harm, among those who self-harm repeatedly.
Adverse effects
Adverse effect incidence
- Common (>1% incidence) adverse effects include
- Extrapyramidal side effects such as: (which usually become apparent soon after therapy is begun or soon after an increase in dose is made)
- Dry mouth
- Constipation
- Hypersalivation – excessive salivation
- Blurred vision
- Diaphoresis – excessive sweating
- Nausea
- Dizziness
- Somnolence
- Restlessness
- Insomnia
- Overactivity
- Headache
- Nervousness
- Fatigue
- Myalgia
- Hyperprolactinemia and its complications such as: (acutely)
- Sexual dysfunction
- Amenorrhea – cessation of menstrual cycles
- Gynecomastia – enlargement of breast tissue in males
- Galactorrhea – the expulsion of breast milk that's not related to breastfeeding or pregnancy
- and if the hyperprolactinemia persists chronically, the following adverse effects may be seen:
- Reduced bone mineral density leading to osteoporosis (brittle bones)
- Infertility
- Dyspepsia – indigestion
- Abdominal pain
- Flatulence
- Nasal congestion
- Polyuria – passing more urine than usual
- Uncommon (0.1–1% incidence) adverse effects include
- Fainting
- Palpitations
- Rare (<0.1% incidence) adverse effects include
- Blood dyscrasias (abnormalities in the cell composition of blood), such as:
- Agranulocytosis – a drop in white blood cell counts that leaves one open to potentially life-threatening infections
- Neutropenia – a drop in the number of neutrophils (white blood cells that specifically fight bacteria) in one's blood
- Leucopenia – a less severe drop in white blood cell counts than agranulocytosis
- Thrombocytopenia – a drop in the number of platelets in the blood. Platelets are responsible for blood clotting and hence this leads to an increased risk of bruising and other bleeds
- Neuroleptic malignant syndrome – a potentially fatal condition that appear to result from central D2 receptor blockade. The symptoms include:
- Hyperthermia
- Muscle rigidity
- Rhabdomyolysis
- Autonomic instability (e.g., tachycardia, diarrhea, diaphoresis, etc.)
- Mental status changes (e.g., coma, agitation, anxiety, confusion, etc.)
- Unknown incidence adverse effects include
- Jaundice
- Abnormal liver function test results
- Tardive dyskinesia – an often incurable movement disorder that usually results from years of continuous treatment with antipsychotic drugs, especially typical antipsychotics like flupenthixol. It presents with repetitive, involuntary, purposeless and slow movements; TD can be triggered by a fast dose reduction in any antipsychotic.
- Hypotension
- Confusional state
- Seizures
- Mania
- Hypomania
- Depression
- Hot flush
- Anergia
- Appetite changes
- Weight changes
- Hyperglycemia – high blood glucose (sugar) levels
- Abnormal glucose tolerance
- Pruritus – itchiness
- Rash
- Dermatitis
- Photosensitivity – sensitivity to light
- Oculogyric crisis
- Accommodation disorder
- Sleep disorder
- Impaired concentration
- Tachycardia
- QTc interval prolongation – an abnormality in the electrical activity of the heart that can lead to potentially fatal changes in heart rhythm (only in overdose or <10 ms increases in QTc)
- Torsades de pointes
- Miosis – constriction of the pupil of the eye
- Paralytic ileus – paralysis of the bowel muscles leading to severe constipation, inability to pass wind, etc.
- Mydriasis
- Glaucoma
Interactions
It should not be used concomitantly with medications known to prolong the QTc interval (e.g., 5-HT3 antagonists, tricyclic antidepressants, citalopram, etc.) as this may lead to an increased risk of QTc interval prolongation. Neither should it be given concurrently with lithium (medication) as it may increase the risk of lithium toxicity and neuroleptic malignant syndrome. It should not be given concurrently with other antipsychotics due to the potential for this to increase the risk of side effects, especially neurological side effects such as neuroleptic malignant syndrome. It should be avoided in patients on CNS depressants such as opioids, alcohol and barbiturates.
Contraindications
It should not be given in the following disease states:
- Pheochromocytoma
- Prolactin-dependent tumors such as pituitary prolactinomas and breast cancer
- Long QT syndrome
- Coma
- Circulatory collapse
- Subcortical brain damage
- Blood dyscrasia
- Parkinson's disease
- Dementia with Lewy bodies
Pharmacology
Pharmacodynamics
Binding profile
| Protein | cis-flupentixol | trans-flupentixol |
|---|---|---|
| 5-HT1A | 8028 | — |
| 5-HT2A | 87.5 (HFC) | — |
| 5-HT2C | 102.2 (RC) | — |
| mAChRs | Neg. | Neg. |
| D1 | 3.5 | 474 (MB) |
| D2 | 0.35 | 120 |
| D3 | 1.75 | 162.5 |
| D4 | 66.3 | >1000 |
| H1 | 0.86 | 5.73 |
Acronyms used:
HFC – Human frontal cortex receptor
MB – Mouse brain receptor
RC – Cloned rat receptor
A study measuring the in vivo receptor occupancies of 13 schizophrenic patients treated with 5.7 ± 1.4 mg/day of flupentixol found 50-70% receptor occupancy for D2, 20 ± 5% for D1, and 20 ± 10% for 5-HT2A.
Its antipsychotic effects are predominantly a function of D2 antagonism.
Its antidepressant effects at lower doses are not well understood; however, it may be mediated by functional selectivity and/or preferentially binding to D2 autoreceptors at low doses, resulting in increased postsynaptic activation via higher dopamine levels. Flupentixol's demonstrated ability to raise dopamine levels in mice and flies lends credibility to the supposition of autoreceptor bias. Functional selectivity may be responsible through causing preferential autoreceptor binding or other means. The effective dosage guideline for an antipsychotic is very closely related to its receptor residency time (i.e., where drugs like aripiprazole take several minutes or more to disassociate from a receptor while drugs like quetiapine and clozapine—with guideline dosages in the hundreds of milligrams—take under 30s) and long receptor residency time is strongly correlated with likehood of pronounced functional selectivity; thus, with a maximum guideline dose of only 18 mg/day for schizophrenia, there is a significant possibility of this drug possessing unique signalling characteristics that permit counterintuitive dopaminergic action at low doses.
Pharmacokinetics
| Medication | Brand name | Class | Vehicle | Dosage | Tmax | t1/2 single | t1/2 multiple | logP | Ref |
|---|---|---|---|---|---|---|---|---|---|
| Aripiprazole lauroxil | Aristada | Atypical | Water | 441–1064 mg/4–8 weeks | 24–35 days | ? | 54–57 days | 7.9–10.0 | |
| Aripiprazole monohydrate | Abilify Maintena | Atypical | Water | 300–400 mg/4 weeks | 7 days | ? | 30–47 days | 4.9–5.2 | |
| Bromperidol decanoate | Impromen Decanoas | Typical | Sesame oil | 40–300 mg/4 weeks | 3–9 days | ? | 21–25 days | 7.9 | |
| Clopentixol decanoate | Sordinol Depot | Typical | Viscoleo | 50–600 mg/1–4 weeks | 4–7 days | ? | 19 days | 9.0 | |
| Flupentixol decanoate | Depixol | Typical | Viscoleo | 10–200 mg/2–4 weeks | 4–10 days | 8 days | 17 days | 7.2–9.2 | |
| Fluphenazine decanoate | Prolixin Decanoate | Typical | Sesame oil | 12.5–100 mg/2–5 weeks | 1–2 days | 1–10 days | 14–100 days | 7.2–9.0 | |
| Fluphenazine enanthate | Prolixin Enanthate | Typical | Sesame oil | 12.5–100 mg/1–4 weeks | 2–3 days | 4 days | ? | 6.4–7.4 | |
| Fluspirilene | Imap, Redeptin | Typical | Water | 2–12 mg/1 week | 1–8 days | 7 days | ? | 5.2–5.8 | |
| Haloperidol decanoate | Haldol Decanoate | Typical | Sesame oil | 20–400 mg/2–4 weeks | 3–9 days | 18–21 days | 7.2–7.9 | ||
| Olanzapine pamoate | Zyprexa Relprevv | Atypical | Water | 150–405 mg/2–4 weeks | 7 days | ? | 30 days | – | |
| Oxyprothepin decanoate | Meclopin | Typical | ? | ? | ? | ? | ? | 8.5–8.7 | |
| Paliperidone palmitate | Invega Sustenna | Atypical | Water | 39–819 mg/4–12 weeks | 13–33 days | 25–139 days | ? | 8.1–10.1 | |
| Perphenazine decanoate | Trilafon Dekanoat | Typical | Sesame oil | 50–200 mg/2–4 weeks | ? | ? | 27 days | 8.9 | |
| Perphenazine enanthate | Trilafon Enanthate | Typical | Sesame oil | 25–200 mg/2 weeks | 2–3 days | ? | 4–7 days | 6.4–7.2 | |
| Pipotiazine palmitate | Piportil Longum | Typical | Viscoleo | 25–400 mg/4 weeks | 9–10 days | ? | 14–21 days | 8.5–11.6 | |
| Pipotiazine undecylenate | Piportil Medium | Typical | Sesame oil | 100–200 mg/2 weeks | ? | ? | ? | 8.4 | |
| Risperidone | Risperdal Consta | Atypical | Microspheres | 12.5–75 mg/2 weeks | 21 days | ? | 3–6 days | – | |
| Zuclopentixol acetate | Clopixol Acuphase | Typical | Viscoleo | 50–200 mg/1–3 days | 1–2 days | 1–2 days | 4.7–4.9 | ||
| Zuclopentixol decanoate | Clopixol Depot | Typical | Viscoleo | 50–800 mg/2–4 weeks | 4–9 days | ? | 11–21 days | 7.5–9.0 | |
| Note: All by intramuscular injection. Footnotes: = Microcrystalline or nanocrystalline aqueous suspension. = Low-viscosity vegetable oil (specifically fractionated coconut oil with medium-chain triglycerides). = Predicted, from PubChem and DrugBank. Sources: Main: See template. | |||||||||
History
In March 1963 the Danish pharmaceutical company Lundbeck began research into further agents for schizophrenia, having already developed the thioxanthene derivatives clopenthixol and chlorprothixene. By 1965 the promising agent flupenthixol had been developed and trialled in two hospitals in Vienna by Austrian psychiatrist Heinrich Gross. The long- acting decanoate preparation was synthesised in 1967 and introduced into hospital practice in Sweden in 1968, with a reduction in relapses among patients who were put on the depot.
References
- Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- ^ "Depixol Tablets 3mg - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Lundbeck Ltd. 27 December 2012. Retrieved 20 October 2013.
- Balant-Gorgia AE, Balant L (August 1987). "Antipsychotic drugs. Clinical pharmacokinetics of potential candidates for plasma concentration monitoring". Clinical Pharmacokinetics. 13 (2): 65–90. doi:10.2165/00003088-198713020-00001. PMID 2887326. S2CID 24707620.
- Jann MW, Ereshefsky L, Saklad SR (July–August 1985). "Clinical pharmacokinetics of the depot antipsychotics". Clinical Pharmacokinetics. 10 (4): 315–333. doi:10.2165/00003088-198510040-00003. PMID 2864156. S2CID 12848774.
- ^ Joint Formulary Committee (2013). British National Formulary (BNF) (65 ed.). London, UK: Pharmaceutical Press. ISBN 978-0-85711-084-8.
- ^ Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- "Fluanxol® (flupentixol) Tablets Registration Certificate". Russian State Register of Medicinal Products. Retrieved 29 July 2014.
- Shen X, Xia J, Adams CE (November 2012). Shen X (ed.). "Flupenthixol versus placebo for schizophrenia". The Cochrane Database of Systematic Reviews. 2012 (11): CD009777. doi:10.1002/14651858.CD009777.pub2. PMC 11531908. PMID 23152280.
- Robertson MM, Trimble MR (May 1981). "The antidepressant action of flupenthixol". The Practitioner. 225 (1355): 761–763. PMID 7291129.
- Pöldinger W, Sieberns S (1983). "Depression-inducing and antidepressive effects of neuroleptics. Experiences with flupenthixol and flupenthixol decanoate". Neuropsychobiology. 10 (2–3): 131–136. doi:10.1159/000117999. PMID 6674820.
- Johnson DA (January 1979). "A double-blind comparison of flupenthixol, nortriptyline and diazepam in neurotic depression". Acta Psychiatrica Scandinavica. 59 (1): 1–8. doi:10.1111/j.1600-0447.1979.tb06940.x. PMID 369298. S2CID 144717662.
- Young JP, Hughes WC, Lader MH (May 1976). "A controlled comparison of flupenthixol and amitriptyline in depressed outpatients". British Medical Journal. 1 (6018): 1116–1118. doi:10.1136/bmj.1.6018.1116. PMC 1639983. PMID 773506.
- Fujiwara J, Ishino H, Baba O, Hanaoka M, Sasaki K (August 1976). "Effect of flupenthixol on depression with special reference to combination use with tricyclic antidepressants. An uncontrolled pilot study with 45 patients". Acta Psychiatrica Scandinavica. 54 (2): 99–105. doi:10.1111/j.1600-0447.1976.tb00101.x. PMID 961463. S2CID 25364795.
- Tam W, Young JP, John G, Lader MH (March 1982). "A controlled comparison of flupenthixol decanoate injections and oral amitriptyline in depressed out-patients". The British Journal of Psychiatry. 140 (3): 287–291. doi:10.1192/bjp.140.3.287. PMID 7093597. S2CID 30537435.
- Hawton K, Witt KG, Taylor Salisbury TL, Arensman E, Gunnell D, Hazell P, et al. (July 2015). "Pharmacological interventions for self-harm in adults". The Cochrane Database of Systematic Reviews. 2015 (7): CD011777. doi:10.1002/14651858.CD011777. hdl:10536/DRO/DU:30080508. PMC 8637297. PMID 26147958.
- Bostwick JR, Guthrie SK, Ellingrod VL (January 2009). "Antipsychotic-induced hyperprolactinemia". Pharmacotherapy. 29 (1): 64–73. doi:10.1592/phco.29.1.64. hdl:2027.42/90238. PMID 19113797. S2CID 25981099.
- ^ "FLUANXOL® DEPOT FLUANXOL® CONCENTRATED DEPOT". TGA eBusiness Services. Lundbeck Australia Pty Ltd. 28 June 2013. Retrieved 20 October 2013.
- "Guidelines for the Management of QTc Prolongation in Adults Prescribed Antipsychotics" (PDF). nhs.uk.
- Lambiase PD, de Bono JP, Schilling RJ, Lowe M, Turley A, Slade A, et al. (July 2019). "British Heart Rhythm Society Clinical Practice Guidelines on the Management of Patients Developing QT Prolongation on Antipsychotic Medication". Arrhythmia & Electrophysiology Review. 8 (3): 161–165. doi:10.15420/aer.2019.8.3.G1. PMC 6702465. PMID 31463053.
- Roth, BL, Driscol, J (12 January 2011). "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 8 November 2013. Retrieved 20 October 2013.
- Golds PR, Przyslo FR, Strange PG (March 1980). "The binding of some antidepressant drugs to brain muscarinic acetylcholine receptors". British Journal of Pharmacology. 68 (3): 541–549. doi:10.1111/j.1476-5381.1980.tb14570.x. PMC 2044199. PMID 7052344.
- Reimold M, Solbach C, Noda S, Schaefer JE, Bartels M, Beneke M, et al. (February 2007). "Occupancy of dopamine D(1), D (2) and serotonin (2A) receptors in schizophrenic patients treated with flupentixol in comparison with risperidone and haloperidol". Psychopharmacology. 190 (2): 241–249. doi:10.1007/s00213-006-0611-0. PMID 17111172. S2CID 2231884.
- Hyttel J (January 1977). "Changes in dopamine synthesis rate in the supersensitivity phase after treatment with a single dose of neuroleptics". Psychopharmacology. 51 (2): 205–207. doi:10.1007/BF00431742. PMID 14353. S2CID 22801301.
- Vickrey TL, Venton BJ (December 2011). "Drosophila Dopamine2-like receptors function as autoreceptors". ACS Chemical Neuroscience. 2 (12): 723–729. doi:10.1021/cn200057k. PMC 3269839. PMID 22308204.
- Kapur S, Seeman P (March 2001). "Does fast dissociation from the dopamine d(2) receptor explain the action of atypical antipsychotics?: A new hypothesis". The American Journal of Psychiatry. 158 (3): 360–369. doi:10.1176/appi.ajp.158.3.360. PMID 11229973.
- Kapur S, Seeman P (March 2000). "Antipsychotic agents differ in how fast they come off the dopamine D2 receptors. Implications for atypical antipsychotic action". Journal of Psychiatry & Neuroscience. 25 (2): 161–166. PMC 1408069. PMID 10740989.
- Carboni L, Negri M, Michielin F, Bertani S, Fratte SD, Oliosi B, Cavanni P (June 2012). "Slow dissociation of partial agonists from the D₂ receptor is linked to reduced prolactin release". The International Journal of Neuropsychopharmacology. 15 (5): 645–656. doi:10.1017/S1461145711000824. PMID 21733233. S2CID 31885144.
- Klein Herenbrink C, Sykes DA, Donthamsetti P, Canals M, Coudrat T, Shonberg J, et al. (February 2016). "The role of kinetic context in apparent biased agonism at GPCRs". Nature Communications. 7: 10842. Bibcode:2016NatCo...710842K. doi:10.1038/ncomms10842. PMC 4770093. PMID 26905976.
- Parent M, Toussaint C, Gilson H (1983). "Long-term treatment of chronic psychotics with bromperidol decanoate: clinical and pharmacokinetic evaluation". Current Therapeutic Research. 34 (1): 1–6.
- ^ Jørgensen A, Overø KF (1980). "Clopenthixol and flupenthixol depot preparations in outpatient schizophrenics. III. Serum levels". Acta Psychiatrica Scandinavica. Supplementum. 279: 41–54. doi:10.1111/j.1600-0447.1980.tb07082.x. PMID 6931472.
- ^ Reynolds JE (1993). "Anxiolytic sedatives, hypnotics and neuroleptics.". Martindale: The Extra Pharmacopoeia (30th ed.). London: Pharmaceutical Press. pp. 364–623.
- Ereshefsky L, Saklad SR, Jann MW, Davis CM, Richards A, Seidel DR (May 1984). "Future of depot neuroleptic therapy: pharmacokinetic and pharmacodynamic approaches". The Journal of Clinical Psychiatry. 45 (5 Pt 2): 50–9. PMID 6143748.
- ^ Curry SH, Whelpton R, de Schepper PJ, Vranckx S, Schiff AA (April 1979). "Kinetics of fluphenazine after fluphenazine dihydrochloride, enanthate and decanoate administration to man". British Journal of Clinical Pharmacology. 7 (4): 325–31. doi:10.1111/j.1365-2125.1979.tb00941.x. PMC 1429660. PMID 444352.
- Young D, Ereshefsky L, Saklad SR, Jann MW, Garcia N (1984). Explaining the pharmacokinetics of fluphenazine through computer simulations. (Abstract.). 19th Annual Midyear Clinical Meeting of the American Society of Hospital Pharmacists. Dallas, Texas.
- Janssen PA, Niemegeers CJ, Schellekens KH, Lenaerts FM, Verbruggen FJ, van Nueten JM, Marsboom RH, Hérin VV, Schaper WK (November 1970). "The pharmacology of fluspirilene (R 6218), a potent, long-acting and injectable neuroleptic drug". Arzneimittel-Forschung. 20 (11): 1689–98. PMID 4992598.
- Beresford R, Ward A (January 1987). "Haloperidol decanoate. A preliminary review of its pharmacodynamic and pharmacokinetic properties and therapeutic use in psychosis". Drugs. 33 (1): 31–49. doi:10.2165/00003495-198733010-00002. PMID 3545764.
- Reyntigens AJ, Heykants JJ, Woestenborghs RJ, Gelders YG, Aerts TJ (1982). "Pharmacokinetics of haloperidol decanoate. A 2-year follow-up". International Pharmacopsychiatry. 17 (4): 238–46. doi:10.1159/000468580. PMID 7185768.
- Larsson M, Axelsson R, Forsman A (1984). "On the pharmacokinetics of perphenazine: a clinical study of perphenazine enanthate and decanoate". Current Therapeutic Research. 36 (6): 1071–88.
- Gross H, Kaltenbäck E (1965). "Flupenthixol (Fluanxol®), ein Neues Neuroleptikum aus der Thiaxanthenreihe (Klinische Erfahrungen bei Einem Psychiatrischen Krankengut)". Acta Psychiatrica Scandinavica. 41: 42–56. doi:10.1111/j.1600-0447.1965.tb04969.x. S2CID 145021607.
- Gottfries CG, Green L (1974). "Flupenthixol decanoate--in treatment of out-patients". Acta Psychiatrica Scandinavica. Supplementum. 255: 15–24. doi:10.1111/j.1600-0447.1974.tb08890.x. PMID 4533707. S2CID 42657501.
| Anxiolytics (N05B) | |
|---|---|
| 5-HT1ARTooltip 5-HT1A receptor agonists | |
| GABAARTooltip GABAA receptor PAMsTooltip positive allosteric modulators |
|
| Hypnotics | |
| Gabapentinoids (α2δ VDCC blockers) | |
| Antidepressants |
|
| Antipsychotics | |
| Sympatholytics (Antiadrenergics) |
|
| Others | |
| |
| Pharmacodynamics | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Tricyclics | |
|---|---|
| Classes | |
| Antidepressants (Tricyclic antidepressants (TCAs)) |
|
| Antihistamines |
|
| Antipsychotics |
|
| Anticonvulsants | |
| Anticholinergics | |
| Others | |