| Revision as of 12:16, 20 November 2013 view source71.212.115.137 (talk) Who was editing this page before? It was accurate, then all of these errors and typographical errors appeared.← Previous edit | Revision as of 15:23, 20 November 2013 view source Dala11a (talk | contribs)Extended confirmed users3,181 edits The term "medical" is claimedNext edit → | ||
| Line 9: | Line 9: | ||
| '''Medical cannabis''' refers to the parts of the herb ] used as a form of medicine or ], or to synthetic forms of specific ] such as ] (delta-9-tetrahydrocannabinol) as a form of medicine. The ] has been used as a medicine over an extensive period of time.<ref name="Amar2006">{{cite journal |doi=10.1016/j.jep.2006.02.001 |title=Cannabinoids in medicine: A review of their therapeutic potential |year=2006 |last1=Ben Amar |first1=Mohamed |journal=Journal of Ethnopharmacology |volume=105 |pages=1–25 |pmid=16540272 |issue=1–2}}</ref> Cannabis is one of the ] of ],<ref name="Wong">{{Cite book|last=Wong |first=Ming |year=1976 |title=La Médecine chinoise par les plantes |publisher=Tchou |location=Paris |oclc=2646789}}{{Page needed|date=August 2010}}</ref> and is prescribed for a broad range of indications. | '''Medical cannabis''' refers to the parts of the herb ] used as a form of medicine or ], or to synthetic forms of specific ] such as ] (delta-9-tetrahydrocannabinol) as a form of medicine. The ] has been used as a medicine over an extensive period of time.<ref name="Amar2006">{{cite journal |doi=10.1016/j.jep.2006.02.001 |title=Cannabinoids in medicine: A review of their therapeutic potential |year=2006 |last1=Ben Amar |first1=Mohamed |journal=Journal of Ethnopharmacology |volume=105 |pages=1–25 |pmid=16540272 |issue=1–2}}</ref> Cannabis is one of the ] of ],<ref name="Wong">{{Cite book|last=Wong |first=Ming |year=1976 |title=La Médecine chinoise par les plantes |publisher=Tchou |location=Paris |oclc=2646789}}{{Page needed|date=August 2010}}</ref> and is prescribed for a broad range of indications. | ||
| However, organizations such as the ] dismiss the concept of medical cannabis because the plant in question fails to meet its standard requirements for approved medicines, as well as those of the United States (US) ] and similar agencies in other countries ; that is, cannabis is associated with numerous harmful health effects, and significant aspects such as content, production, and supply are not regulated.<ref></ref><ref></ref> | |||
| <!-- | <!-- | ||
| = INTRO NOTE ON FDA ========================= | = INTRO NOTE ON FDA ========================= | ||
| Line 20: | Line 20: | ||
| | | | | ||
| = Thank you! ================================ | = Thank you! ================================ | ||
| -->== Strains ==<!-- linked to Template:Cannabis --> | -->== Strains ==<!-- linked to Template:Cannabis --> | ||
| ] | ] | ||
Revision as of 15:23, 20 November 2013
This article is about the medical uses of cannabis. For general drug information, see Cannabis (drug). For other uses, see Cannabis (disambiguation).This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these messages)
|


Medical cannabis refers to the parts of the herb cannabis used as a form of medicine or herbal therapy, or to synthetic forms of specific cannabinoids such as THC (delta-9-tetrahydrocannabinol) as a form of medicine. The Cannabis plant has been used as a medicine over an extensive period of time. Cannabis is one of the 50 "fundamental" herbs of traditional Chinese medicine, and is prescribed for a broad range of indications.
However, organizations such as the American Society of Addiction Medicine dismiss the concept of medical cannabis because the plant in question fails to meet its standard requirements for approved medicines, as well as those of the United States (US) Food and Drug Administration (FDA) and similar agencies in other countries ; that is, cannabis is associated with numerous harmful health effects, and significant aspects such as content, production, and supply are not regulated.
Strains
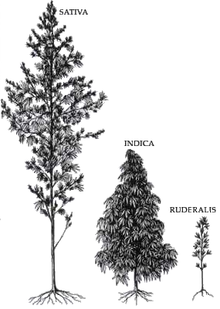
The genus Cannabis contains two species which produce useful amounts of psychoactive cannabinoids. Cannabis indica produces a higher level of Cannabidiol (abbreviated CBD) relative to THC (the primary psychoactive component in medical and recreational cannabis). Cannabis sativa, on the other hand, produces a higher level of THC relative to CBD.
Medical use of sativa is associated with a cerebral high, and many patients experience stimulating effects. For this reason, sativa is often used for daytime treatment. It may cause more of a euphoric, "high" sensation, and tends to stimulate hunger, making it potentially useful to patients with eating disorders or anorexia. Sativa also exhibits a higher tendency to induce anxiety and paranoia, so patients prone to these effects may limit treatment with pure sativa, or choose hybrid strains.
Cannabis indica is associated with sedative effects and is often preferred for night time use, including for treatment of insomnia. Indica is also associated with a more "stoned" or meditative sensation than the euphoric, stimulating effects of sativa, possibly because of a higher CBD-to-THC ratio.
Many strains of cannabis are currently cultivated for medical use, including strains of both species in varying potencies, as well as hybrid strains designed to incorporate the benefits of both species. Hybrids commonly available can be heavily dominated by either Cannabis sativa or Cannabis indica, or relatively balanced, such as so-called "50/50" strains.
Cannabis strains with relatively high CBD-to-THC ratios, usually indica-dominant strains, are less likely to induce anxiety. This may be due to CBD's receptor antagonistic effects at the cannabinoid receptor, compared to THC's partial agonist effect. CBD is also a 5-HT1A receptor agonist, which may also contribute to an anxiolytic effect. This likely means the high concentrations of CBD found in Cannabis indica mitigate the anxiogenic effect of THC significantly.
Use
Medical marijuana is typically classified as an illegal drug in most countries and the US Food and Drug Agency (FDA) applies the schedule VI category from the Controlled Substances Act (FDA.gov). However, a number of governments, including the U.S. Federal Government, allow treatment with one or more specific low doses of synthetic cannabinoids for one or more disorders. In addition to the potential for negative effects, medical marijuana can be used to treat people that are suffering from cancer, AIDS, and chronic pain. Research studies show that medical marijuana is helpful to people who experience chronic non-cancer pain, vomiting and nausea caused by chemotherapy. The drug can also help with treating symptoms of AIDS patients and muscle spasms related to multiple sclerosis. As of 2011, the use of medical marijuana is legalized in 16 U.S. states but still illegal by federal law.

Studies have shown several well-documented beneficial effects of cannabis. Among these are: The amelioration of nausea and vomiting, stimulation of hunger in chemotherapy and AIDS patients, lowered intraocular eye pressure (shown to be effective for treating glaucoma), as well as gastrointestinal illness. The drug also produces antibacterial effects and is one of the best known expectorants. On the National Cancer Institute website, the National Institutes of Health (NIH) stated that cannabinoids found in marijuana appear to have significant analgesic and anti-inflammatory effects, antitumor effects, and anticancer effects, including the treatment of breast and lung cancer. The anti-cancer effect is due to the presence of cannabidiol (CBD) in the plant, an anti-cancer agent that does not cause euphoria.
Sanjay Gupta, a neurosurgeon and chief medical correspondent for the CNN media network, published an essay on the CNN website in August 2013 in which he apologizes for his previous hardline stance against cannabis. In 2009 Gupta wrote a Time magazine article entitled "Why I would Vote No to Pot" but stated in his 2013 piece that "... I was too dismissive of the loud chorus of patients whose symptoms improved on cannabis." His CNN article is entitled "Why I changed my mind on weed" and was written after an extensive period of research. Gupta explains that cannabis has "very legitimate medical applications" and is sometimes "the only thing that works," and, as part of his apology, states, "We have been terribly and systematically misled for nearly 70 years in the United States, and I apologize for my own role in that."
There are several methods for administration of dosage, including vaporizing or smoking dried buds, drinking, or eating extracts, and taking capsules. The comparable efficacy of these methods was the subject of an investigative study conducted by the National Institutes of Health.
While utilizing cannabis for recreational purposes is illegal in many parts of the world, many countries are beginning to consider varying levels of decriminalization for medical usage, including Canada, Austria, Germany, Switzerland, the Netherlands, Czech Republic, Spain, Israel, Italy, Finland, and Portugal. Synthetic cannabinoids are available as prescription drugs in some countries. Examples are Marinol (The United States and Canada) and Cesamet (Canada, Mexico, the United Kingdom, and the United States).
In the U.S., federal legislation outlaws the use of all herb parts from cannabis; states that have approved use of medical cannabis are in conflict with federal law. The United States Supreme Court ruled in United States v. Oakland Cannabis Buyers' Coop and Gonzales v. Raich that the federal government has a right to regulate and criminalize cannabis, even for medical purposes. A person can therefore be prosecuted for a cannabis-related crime even if it is legal medical use according to state laws. The U.S. federal government, through the National Institute on Drug Abuse (NIDA), continues to provide medical cannabis to four patients who participated in the Compassionate Investigational New Drug Program. NIDA claims this is done for "compassionate purposes" and the U.S. federal government still maintains that medical marijuana is not an effective or desirable treatment for any medical condition, despite significant contrary evidence.
Clinical applications

A 2002 review of medical literature by Franjo Grotenhermen states that medical cannabis has established effects in the treatment of nausea, vomiting, premenstrual syndrome, unintentional weight loss, insomnia, and lack of appetite. Other "relatively well-confirmed" effects were in the treatment of "spasticity, painful conditions, especially neurogenic pain, movement disorders, asthma, glaucoma".
Preliminary findings indicate that cannabis-based drugs could prove useful in treating adrenal disease, inflammatory bowel disease, migraines, fibromyalgia, and related conditions.
Medical cannabis has also been found to relieve certain symptoms of multiple sclerosis and spinal cord injuries by exhibiting antispasmodic and muscle-relaxant properties as well as stimulating appetite.
Other studies state that cannabis or cannabinoids may be useful in treating alcohol abuse, amyotrophic lateral sclerosis, collagen-induced arthritis, asthma, atherosclerosis, bipolar disorder, colorectal cancer, HIV-associated sensory neuropathy, depression, dystonia, epilepsy, digestive diseases, gliomas, hepatitis C, Huntington's disease, leukemia, skin tumors, methicillin-resistant Staphylococcus aureus (MRSA), Parkinson's disease, pruritus, posttraumatic stress disorder (PTSD), psoriasis, sickle-cell disease, sleep apnea, and anorexia nervosa. Controlled research on treating Tourette syndrome with a synthetic version of THC called (Marinol), showed the patients taking the pill had a beneficial response without serious adverse effects; other studies have shown that cannabis "has no effects on tics and increases the individuals inner tension". Case reports found that cannabis helped reduce tics, but validation of these results requires longer, controlled studies on larger samples.
A study done by Craig Reinarman surveyed people in California who used cannabis found they did so for many reasons. Reported uses were for pain relief, muscle spasms, headaches, anxiety, nausea, vomiting, depression, cramps, panic attacks, diarrhea, and itching. Others used cannabis to improve sleep, relaxation, appetite, concentration or focus, and energy. Some patients used it to prevent medication side effects, anger, involuntary movements, and seizures, while others used it as a substitute for other prescription medications and alcohol.
Studies
Safety of cannabis
Main article: Long-term effects of cannabisFrom The Lancet, "There are no confirmed published cases worldwide of human deaths from cannabis poisoning, and the dose of THC required to produce 50% mortality in rodents is extremely high compared with other commonly used drugs".
According to Associate Professor Emeritus of Psychiatry at Harvard Medical School Lester Grinspoon, "When cannabis regains its place in the US Pharmacopeia, a status it lost after the passage of the Marijuana Tax Act of 1937, it will be seen as one of the safest drugs in that compendium".
There are medical reports of occasional infarction, stroke and other cardiovascular side effects. Marijuana's cardiovascular effects are not associated with serious health problems for most young, healthy users. Researchers have reported in the International Journal of Cardiology, "Marijuana use by older people, particularly those with some degree of coronary artery or cerebrovascular disease, poses greater risks due to the resulting increase in catecholamines, cardiac workload, and carboxyhemoglobin levels, and concurrent episodes of profound postural hypotension. Indeed, marijuana may be a much more common cause of myocardial infarction than is generally recognized. In day-to-day practice, a history of marijuana use is often not sought by many practitioners, and even when sought, the patient's response is not always truthful. Thus, clinicians should be more vigilant in inquiring about use of marijuana in their patients, particularly among the younger adults who may present with cardiac events in the absence of cardiovascular disease or other obvious risk factors."
A 2012 study published in JAMA and funded by the NIH looked at a population of over 5,115 American men and women to see whether smoked cannabis has effects on the pulmonary system similar to those from smoking tobacco. The researchers found "Occasional and low cumulative marijuana use was not associated with adverse effects on pulmonary function." Smoking an average of one joint a day for seven years, they found, did not worsen pulmonary health.
Cannabis smoke contains thousands of organic and inorganic chemical compounds. This tar is chemically similar to that found in tobacco smoke or cigars. Over fifty known carcinogens have been identified in cannabis smoke. These include nitrosamines, reactive aldehydes, and polycylic hydrocarbons, including benzpyrene. Marijuana smoke was listed as a cancer agent in California in 2009.
A 2006 study involving 1,212 incident cancer cases and 1,040 cancer-free controls found no causative link to oral, laryngeal, pharyngeal, esophageal or lung cancer when adjusting for several confounding factors including cigarette smoking and alcohol use.
Regarding the relative safety of cannabis, former US DEA chief administrative law judge Judge Francis Young said:
- "There is no record in the extensive medical literature describing a proven, documented cannabis-induced fatality. ... Despite long history of use and the extraordinarily high numbers of social smokers, there are simply no credible medical reports to suggest that consuming marijuana has caused a single death. In practical terms, marijuana cannot induce a lethal response as a result of drug-related toxicity. ... Marijuana's therapeutic ratio is impossible to quantify because it is so high. ... Marijuana, in its natural form, is one of the safest therapeutically active substances known to man."
Pain relief
The effectiveness of cannabis as an analgesic has been the subject of numerous studies. University of Oxford doctors found that the brain on THC showed reduced response to pain, suggesting that the drug may help patients endure pain. Brain scans showed reduced activity in two centers of the brain where pain is registered: The mid-Anterior cingulate cortex and the right Amygdala. However, cannabis did not block the sensation of pain like morphine-based pain killers. The researchers also found a great degree of variation among individual reports of pain relief.
According to Stuart Silverman, M.D., a rheumatologist at Cedars-Sinai Medical Center, "Historically and anecdotally, marijuana has been used as a painkiller". A Canadian study showed cannabis can reduce "nerve pain" from surgical complications or injuries. The study's twenty-one subjects suffered from chronic pain and patients who smoked cannabis with a 9.4% THC content reported less pain than those patients who smoked the placebo. Improved quality of sleep and reduced anxiety were other reported benefits. Igor Grant, psychiatrist and director of the Center for Medicinal Cannabis Research at the University of California San Diego, has stated, "There is good evidence now that cannabinoids may be either an adjunct or a first-line treatment". Grant explained further that not everyone experienced pain relief, but the percentage of people who did was comparable to those who said that they experienced relief from other medications commonly prescribed for neuropathic pain (the subject of his study), such as antidepressants.
A small-scale UCSF study found that patients with chronic pain may experience greater relief if cannabinoids were added to an opiate-only treatment regime. The findings further suggested that combination therapy could result in reduced opiate dosages. The College of Physicians and Surgeons at Columbia University, U.S. published a study in the Neuropsychopharmacology journal in 2013 that is based on research that was conducted with fifteen males and fifteen females who smoked marijuana every day. The study's subjects were exposed to either a placebo, inhaled marijuana, or dronabinol, a pill that contains cannabis' psychoactive ingredient. Participants were monitored to ensure that they had not smoked in the time period immediately prior to the tests and did not have other drugs (including alcohol) in their systems. The researchers concluded that "Dronabinol administration decreased pain sensitivity and increased pain tolerance that peaked later and lasted longer relative to smoked marijuana", thereby providing evidence that the pill form was superior to smoked cannabis in terms of pain relief efficacy. However, the Columbia researchers further stated, "A primary caveat of the current findings is that the study population consisted of daily marijuana smokers; this study limitation should be considered when interpreting the findings and placing them within the context of the potential therapeutic feasibility of cannabinoids ."
Antiemetic
Several studies have established the antiemetic effects of cannabinoids in the treatment of chemotherapy induced nausea and vomiting (CINV). Comparative studies have found cannabinoids to be more effective than some conventional anti emetics such as prochlorperazine, promethazine, and metoclopramide in controlling CINV. Their use is generally limited by the high incidence of side effects, such as dizziness, dysphoria, and hallucinations. Cannabinoids are considered reserve medications in the treatment of nausea and vomiting induced by cytostatics.
Glaucoma

In glaucoma, cannabis and THC have been shown to reduce intra-ocular pressure (IOP) by an average of 24% in people with normal IOP who have visual-field changes. In studies of healthy adults and glaucoma patients, IOP was reduced by an average of 25% after smoking a cannabis "cigarette" that contained approximately 2% THC—a reduction as good as that observed with most other medications available today, according to a review by the Institute of Medicine.
In a separate study, the use of cannabis and glaucoma was tested and found that the duration of smoked or ingested cannabis or other cannabinoids is very short, averaging 3 to 3.5 hours. Their results showed that for cannabis to be a viable therapy, the patient would have to take in cannabis in some form every 3 hours. They said that for ideal glaucoma treatment it would take two times a day at most for compliance purposes from patients. Due to these limitations, the American Glaucoma Society, in a statement in 2009, did not recommend marijuana yet as a viable glaucoma treatment, even if it expressed hope that "marijuana or related compounds could protect the optic nerve not only through IOP lowering but also through a neuroprotective mechanism."
Spasticity in multiple sclerosis

A review of six randomized controlled trials of a combination of THC and CBD extracts for the treatment of multiple sclerosis (MS) related muscle spasticity reported, "Although there was variation in the outcome measures reported in these studies, a trend of reduced spasticity in treated patients was noted." The authors postulated that "cannabinoids may provide neuroprotective and anti-inflammatory benefits in MS." A small study done on whether or not cannabis could be used to control tremors of MS patients was conducted. The study found that there was no noticeable difference of the tremors in the patients. Although there was no difference in the tremors, the patients felt as if their symptoms had lessened and their quality of life had improved. The researchers concluded that the mood enhancing or cognitive effects that cannabis has on the brain could have given the patients the effect that their tremors were getting better.
Alzheimer's disease
Research done by the Scripps Research Institute in California shows that the active ingredient in marijuana, THC, prevents the formation of deposits in the brain associated with Alzheimer's disease. THC was found to prevent an enzyme called acetylcholinesterase from accelerating the formation of "Alzheimer plaques" in the brain more effectively than commercially marketed drugs. THC is also more effective at blocking clumps of protein that can inhibit memory and cognition in Alzheimer's patients, as reported in Molecular Pharmaceutics. Cannabinoids can also potentially prevent or slow the progression of Alzheimer's disease by reducing tau protein phosphorylation, oxidative stress, and neuroinflammation.
According to an article in BBC News, “Marijuana May Block Alzheimer’s”, a 2005 Study conducted by The Alzheimer’s Research Trust, it may be possible to make drugs that act only on CR2 ... they might mimic the positive effects of cannabinoids without the damaging ones of marijuana. The same researchers also stated that this is still a fairly new field of research and it is not east to produce such precise drugs. The Alzheimer’s Research Trust also stated that there is also no evidence yet that cannabinoid-based drugs can slow the decline in human Alzheimer's patients. Medical Marijuana is generally recognized that as well as providing a 'high,' long-term use of marijuana can also lead to depression in many individuals.
A 2012 review from the Philosophical Transactions of a Royal Society B suggested that activating the cannabinoid system may trigger an "anti-oxidant cleanse" in the brain by removing damaged cells and improving the efficiency of the mitochondria. The review found cannabinoids may slow decline in age and disease-related cognitive functioning.
Breast cancer
According to a 2007 and a 2010 study at the California Pacific Medical Center Research Institute, cannabidiol (CBD) stops breast cancer from spreading throughout the body by downregulating a gene called ID1. This may provide a non-toxic alternative to chemotherapy while achieving the same results without the painful and unpleasant side effects. The research team says that CBD works by blocking the activity of a gene called ID1, which is believed to be responsible for a process called metastasis, which is the aggressive spread of cancer cells away from the original tumor site. According to findings released by the team in 2012, when the particularly aggressive "triple-negative" cells (which contain high levels of ID1 and account for 15% of breast cancers) were exposed to CBD, they "not only stopped acting 'crazy' but also returned to a healthy normal state". Human trial models are currently in development. Dr Sean McAllister, study co-leader, commented:
- "The preclinical trial data is very strong, and there's no toxicity. There's really a lot of research to move ahead with and to get people excited".
HIV/AIDS
Investigators at Columbia University published clinical trial data in 2007 showing that HIV/AIDS patients who inhaled cannabis four times daily experienced substantial increases in food intake with little evidence of discomfort and no impairment of cognitive performance. They concluded that smoked cannabis has a clear medical benefit in HIV-positive patients. In another study in 2008, researchers at the University of California, San Diego School of Medicine found that marijuana significantly reduces HIV-related neuropathic pain when added to a patient's already-prescribed pain management regimen and may be an "effective option for pain relief" in those whose pain is not controlled with current medications. Mood disturbance, physical disability, and quality of life all improved significantly during study treatment. Despite management with opioids and other pain modifying therapies, neuropathic pain continues to reduce the quality of life and daily functioning in HIV-infected individuals. Cannabinoid receptors in the central and peripheral nervous systems have been shown to modulate pain perception. No serious adverse effects were reported, according to the study published by the American Academy of Neurology. A study examining the effectiveness of different drugs for HIV associated neuropathic pain found that smoked Cannabis was one of only three drugs that showed evidence of efficacy.
Brain cancer
A study by Complutense University of Madrid found the chemicals in cannabis promote the death of brain cancer cells by essentially helping them feed upon themselves in a process called autophagy. The research team discovered that cannabinoids such as THC had anticancer effects in mice with human brain cancer cells and in people with brain tumors. When mice with the human brain cancer cells received the THC, the tumor shrank. Using electron microscopes to analyze brain tissue taken both before and after a 26-to 30-day THC treatment regimen, the researchers found that THC eliminated cancer cells while leaving healthy cells intact. The patients did not have any toxic effects from the treatment; previous studies of THC for the treatment of cancer have also found the therapy to be well tolerated.
Opioid dependence
Injections of THC eliminate dependence on opiates in stressed rats, according to a research team at the Laboratory for Physiopathology of Diseases of the Central Nervous System (France) in the journal Neuropsychopharmacology. Deprived of their mothers at birth, rats become hypersensitive to the rewarding effect of morphine and heroin (substances belonging to the opiate family), and rapidly become dependent. When these rats were administered THC, they no longer developed typical morphine-dependent behavior. In the striatum, a region of the brain involved in drug dependence, the production of endogenous enkephalins was restored under THC, whereas it diminished in rats stressed from birth which had not received THC. Researchers believe the findings could lead to therapeutic alternatives to existing substitution treatments.
In humans, drug treatment subjects who use cannabis intermittently are found to be more likely to adhere to treatment for opioid dependence. Historically, similar findings were reported by Edward Birch, who, in 1889, reported success in treating opiate and chloral addiction with cannabis.
Controlling ALS symptoms
The potential role of cannabis in treating symptoms of ALS (or Lou Gehrig's Disease) has been the subject of recent research. A survey was conducted on 131 people suffering from ALS. The survey asked if the subjects had used cannabis in the last 12 months to control some of their symptoms. Of the 131 subjects, 13 had used the drug in some form to control symptoms. The survey found that cannabis was moderately effective in reducing symptoms of appetite loss, depression, pain, spasticity, drooling and weakness, and the longest relief reported was for depression. The pattern of symptom relief was consistent with those reported by people with other conditions, including multiple sclerosis (Amtmann et al. 2004).
Crohn's Disease
A study published on May 6, 2013 in the journal Clinical Gastroenterology and Hepatology revealed that subjects with Crohn's Disease experienced benefits from inhaled cannabis use. At the completion of the study's treatment period, ten out of the eleven patients that received cannabis treatment displayed substantial improvements in disease-related symptoms, while five of these patients experienced complete remission. The study's authors wrote: "... all patients in the study group expressed strong satisfaction with their treatment and improvement in their daily function." The study was small, but was designed as a randomized placebo-controlled clinical trial, the gold standard for a clinical trial.
Diabetes
A study published on May 16, 2013 in the Journal of American Medicine revealed that regular marijuana use is associated with better glucose control. They found that current marijuana users had significantly lower fasting insulin and were less likely to be insulin resistant, even after excluding patients with a diagnosis of diabetes mellitus. Participants who reported using marijuana in the past month had lower levels of fasting insulin and HOMA-IR and higher levels of high-density lipoprotein cholesterol (HDL-C). These associations were weaker among those who reported using marijuana at least once, but not in the past thirty days, suggesting that the impact of marijuana use on insulin and insulin resistance exists during periods of recent use. The Study there were al
Medicinal compounds
Cannabis contains 483 compounds. At least 80 of these are cannabinoids, which are the basis for medical and scientific use of cannabis. This presents the research problem of isolating the effect of specific compounds and taking account of the interaction of these compounds. Cannabinoids can serve as appetite stimulants, antiemetics, antispasmodics, and have some analgesic effects. Six important cannabinoids found in the cannabis plant are tetrahydrocannabinol, tetrahydrocannabinolic acid, cannabidiol, cannabinol, β-caryophyllene, and cannabigerol.
Tetrahydrocannabinol
Main article: Tetrahydrocannabinol
Tetrahydrocannabinol (THC) is the primary compound responsible for the psychoactive effects of cannabis. The compound is a mild analgesic, and cellular research has shown the compound has antioxidant activity. THC is believed to interact with parts of the brain normally controlled by the endogenous cannabinoid neurotransmitter, anandamide. Anandamide is believed to play a role in pain sensation, memory, and sleep.
Cannabidiol
Main article: Cannabidiol
Cannabidiol (CBD) is a major constituent of medical cannabis. CBD represents up to 40% of extracts of medical cannabis. Cannabidiol has been shown to relieve convulsion, inflammation, anxiety, cough, congestion and nausea, and it inhibits cancer cell growth. Recent studies have shown cannabidiol to be as effective as atypical antipsychotics in treating schizophrenia and psychosis. Because cannabidiol relieves the aforementioned symptoms, cannabis strains with a high amount of CBD may benefit people with multiple sclerosis, frequent anxiety attacks and Tourette syndrome.
Cannabinol
Main article: Cannabinol
Cannabinol (CBN) is a therapeutic cannabinoid found only in trace amounts in Cannabis sativa and Cannabis indica. It is mostly produced as a metabolite, or a breakdown product, of tetrahydrocannabinol (THC). CBN acts as a weak agonist of the CB1 and CB2 receptors, with lower affinity in comparison to THC.
β-Caryophyllene
Main article: Caryophyllene
Part of the mechanism by which medical cannabis has been shown to reduce tissue inflammation is via the compound β-caryophyllene. A cannabinoid receptor called CB2 plays a vital part in reducing inflammation in humans and other animals. β-Caryophyllene has been shown to be a selective activator of the CB2 receptor. β-Caryophyllene is especially concentrated in cannabis essential oil, which contains about 12–35% β-caryophyllene.
Cannabigerol
Main article: CannabigerolLike cannabidiol, cannabigerol is not psychoactive. Cannabigerol has been shown to relieve intraocular pressure, which may be of benefit in the treatment of glaucoma.
Pharmacologic THC and THC derivatives
In the U.S., the FDA has approved several cannabinoids for use as medical therapies: dronabinol (Marinol) and nabilone. These medicines are taken orally.
These medications are usually used when first line treatments for nausea and vomiting associated with cancer chemotherapy fail to work. In extremely high doses and in rare cases "psychotomimetic" side effects are possible. The other commonly used antiemetic drugs are not associated with these side effects.
Marinol's manufacturer stated on their website: "The most frequently reported side effects in patients with AIDS during clinical studies involved the central nervous system (CNS). These CNS effects (euphoria, dizziness, or thinking abnormalities, for example) were reported by 33% of patients taking MARINOL". Four documented fatalities resulting from Marinol have been reported.
Canasol is a cannabis-based medication for glaucoma that relieves intraocular pressure symptoms associated with late-stage glaucoma.
It was created by an ophthalmologist, Dr. Albert Lockhart and Dr. Manley E. West, and began distribution in 1987. As of 2003, it was still being distributed in the United Kingdom, several U.S. states, and several Caribbean nations.
It is notable for being one of the first cannabis-containing pharmaceuticals to be developed for the modern pharmaceutical market and being one of the few such pharmaceuticals to have ever been legally marketed in the United States.
The prescription drug Sativex, an extract of cannabis administered as a sublingual spray, has been approved in Canada for the adjunctive treatment (use alongside other medicines) of both multiple sclerosis and cancer related pain. Sativex has also been approved in the United Kingdom, New Zealand, and the Czech Republic, and is expected to gain approval in other European countries. William Notcutt is one of the chief researchers that has developed Sativex, and he has been working with GW and founder Geoffrey Guy since the company's inception in 1998. Notcutt states that the use of MS as the disease to study "had everything to do with politics."
| Medication | Approval | Country | Licensed indications | Cost |
|---|---|---|---|---|
| Nabilone | 1985 | U.S., Canada | Nausea of cancer chemotherapy that has failed to respond adequately to other antiemetics | US$4000.00 for a year's supply (in Canada) |
| Canasol | 1987 | U.S., Canada, several Caribbean nations | Introcular pressure associated with late-stage Glaucoma | |
| Marinol | 1985 | U.S., Canada (1992) |
Nausea and vomiting associated with cancer chemotherapy in patients who have failed to respond adequately to conventional treatments |
US$652 for 30 doses @ 10 mg online |
| 1992 | U.S. | Anorexia associated with AIDS–related weight loss | ||
| Sativex | 1995 | Canada | Adjunctive treatment for the symptomatic relief of neuropathic pain in multiple sclerosis in adults |
C$ 9,351 per year |
| 1997 | Canada | Pain due to cancer |
Criticism
One of the major criticisms of cannabis as medicine is opposition to smoking as a method of consumption. However, smoking is not necessary due to alternative methods of ingestion. Medicinal cannabis patients can use vaporizers, where the essential cannabis compounds are extracted and inhaled. In addition, edible cannabis, which is produced in various baked goods, is also available, and has demonstrated longer lasting effects.
The United States Food and Drug Administration (FDA) issued an advisory against smoked medical cannabis stating that, "marijuana has a high potential for abuse, has no currently accepted medical use in treatment in the United States, and has a lack of accepted safety for use under medical supervision." The National Institute on Drug Abuse NIDA state that "Marijuana itself is an unlikely medication candidate for several reasons: (1) it is an unpurified plant containing numerous chemicals with unknown health effects; (2) it is typically consumed by smoking further contributing to potential adverse effects; and (3) its cognitive impairing effects may limit its utility".
The Institute of Medicine, run by the United States National Academy of Sciences, conducted a comprehensive study in 1999 to assess the potential health benefits of cannabis and its constituent cannabinoids. The study concluded that smoking cannabis is not recommended for the treatment of any disease condition, but did conclude that nausea, appetite loss, pain and anxiety can all be mitigated by marijuana. While the study expressed reservations about smoked cannabis due to the health risks associated with smoking, the study team concluded that until another mode of ingestion was perfected that could provide the same relief as smoked cannabis, there was no alternative. In addition, the study pointed out the inherent difficulty in marketing a non-patentable herb. Pharmaceutical companies will probably make less investments in product development if the result is not possible to patent. The Institute of Medicine stated that there is little future in smoked cannabis as a medically approved medication. The report also concluded that for certain patients, such as the terminally ill or those with debilitating symptoms, the long-term risks are not of great concern.
Marinol, a synthetic cannabinoid, was less effective than the steroid megestrol in helping cancer patients regain lost appetites. A phase III study found no difference in effects of an oral cannabis extract or THC on appetite and quality of life (QOL) in patients with cancer-related anorexia-cachexia syndrome (CACS) to placebo. "Citing the dangers of cannabis and the lack of clinical research supporting its medicinal value" the American Society of Addiction Medicine in March 2011 issued a white paper recommending a halt to using marijuana as a medicine in U.S. states where it has been declared legal.
Mental disorders
A study of 50,000 Swedish soldiers who had smoked at least once were twice as likely to develop schizophrenia as those who had not smoked. The study concluded that either smoking caused a higher rate of schizophrenia, or that those with schizophrenia were more likely to be drawn to cannabis.
A study by Keele University commissioned by the British government found that between 1996 and 2005 there had been significant reductions in the incidence and prevalence of schizophrenia. From 2000 onwards there were also significant reductions in the prevalence of psychoses. The authors say this data is "not consistent with the hypothesis that increasing cannabis use in earlier decades is associated with increasing schizophrenia or psychoses from the mid-1990s onwards".
A 10-year study on 1,923 individuals from the general population in Germany, aged 14–24, concluded that cannabis use is a risk factor for the development of incident psychotic disorder symptoms, and the continued use might increase the risk. A study conducted by Thomas F. Denson and Mitchell Earleywine found fewer weekly users with symptoms of depression than those that did not use marijuana. They also reported that used marijuana for medical reasons were found to have been more depressed than recreational users, but reported fewer negative symptomatic issues.
However a medical study published in 2009 taken by the Medical Research Council in London, showed there was no significant effect of THC on -raclopride binding. Thus concluding, recreational cannabis users do not release significant amounts of dopamine from an oral THC dose equivalent to a standard cannabis cigarette. This result challenges current models of striatal dopamine release as the mechanism mediating cannabis as risk factor for schizophrenia.
Lung cancer and chronic obstructive pulmonary disease
The evidence to date is conflicting as to whether smoking cannabis increases the risk of developing lung cancer or chronic obstructive pulmonary disease (COPD) among people who do not smoke tobacco. Some of these research results follow below:
- In 2006, Hashibe, Morgenstern, Cui, Tashkin, et al. presented the results from a study involving 2,240 subjects that showed non-tobacco users who smoked marijuana did not exhibit an increased incidence of lung cancer or head-and-neck malignancies. These results were supported even among very long-term, very heavy users of marijuana. Tashkin, a pulmonologist who has studied cannabis for 30 years, commenting in news reports in the lay media on the results of the study he co-authored, suggested, "It's possible that tetrahydrocannabinol (THC) in cannabis smoke may encourage apoptosis, or programmed cell death, causing cells to die off before they have a chance to undergo malignant transformation". He summarized the results found by his study, saying "We hypothesized that there would be a positive association between cannabis use and lung cancer, and that the association would be more positive with heavier use. What we found instead was no association at all, and even a suggestion of some protective effect."
- A case-control study involving 79 cases and 324 controls looked at lung cancer in adults 55 years of age and younger, and found the risk of lung cancer increased 8% (95% confidence interval (CI) 2–15) for each joint-year of cannabis smoking, after adjustment for confounding variables including cigarette smoking, and 7% (95% CI 5–9) for each pack-year of cigarette smoking, after adjustment for confounding variables including cannabis smoking.
- A 2008 study by Hii, Tam, Thompson, and Naughton found that cannabis smoking leads to asymmetrical bullous disease, often in the setting of normal CXR and lung function. In subjects who smoke cannabis, these pathological changes occur at a younger age (approximately 20 years earlier) than in tobacco smokers. However this study involved only 10 patients who also smoked tobacco and had symptoms of the disease prior to the study. There was no control group in the study. The Journal of the Royal Society of Medicine in 2004 found insufficient evidence for a causative link between cannabis smoke and bullous disease.
- Researchers from the University of British Columbia presented a study at the American Thoracic Society 2007 International Conference showing that smoking cannabis and tobacco together more than tripled the risk of developing COPD over just smoking tobacco alone. Similar findings were released in April 2009 by the Vancouver Burden of Obstructive Lung Disease Research Group. The study reported that smoking both tobacco and cannabis synergistically increased the risk of respiratory symptoms and COPD. Smoking only cannabis, however, was not associated with an increased risk of respiratory symptoms of COPD. In a related commentary, pulmonary researcher Donald Tashkin wrote, "... we can be close to concluding that cannabis smoking by itself does not lead to COPD".
Methods of consumption
Any possible harm caused by smoking cannabis can be minimized by the use of a vaporizer or ingesting the drug in an edible form. Vaporizers are devices that heat the active constituents to a temperature below the ignition point of the cannabis, so that the resultant vapors can be inhaled. Combustion of plant material is avoided, thus preventing the formation of carbon monoxide and carcinogens, such as polyaromatic hydrocarbons and benzene. There are pocket-sized forms of vaporizer which use rechargeable batteries, are constructed from wood, and feature removable covers.
A pilot study led by Donald Abrams of UC San Francisco showed that vaporizers eliminate the release of irritants and toxic compounds, while delivering equivalent amounts of THC into the bloodstream.
In order to kill microorganisms, especially the molds A. fumigatus, A. flavus and A. niger, Levitz and Diamond suggested baking marijuana at 150 °C (302 °F) for five minutes. They also found that tetrahydrocannabinol (THC) was not degraded by this process.
Methods of acquisition
The method of obtaining medical cannabis varies by region and by legislation. Currently some of the permitted methods are through regulated marijuana dispensaries (or marijuana clubs) or by self-propagation. Meaning that in some areas it is legal for a person to grow their own marijuana for personal use.
Dispensing machines
A marijuana vending machine is a vending machine for selling or dispensing marijuana. They are currently in use in the United States. In the United States, they are normally located in secure rooms in medical marijuana dispensaries. They are operated by employees after a fingerprint scan is obtained from the patient. In Canada, marijuana vending machines are planned to be used in centres that cultivate the drug.
At least three companies are developing the vending machines. Endexx Corp. (ticker symbol: EDXC) has recently acquired two smaller companies to merge their respective technologies into a marijuana vending machine. The first acquisition, called Cann-Can LLC, was announced by Endexx on April 9, 2013. Cann-Can's founder and developer, David Levine, was brought onto the Endexx board as a specialty consultant. David Levine has extensive vending machine expertise and holds a patent for a vending machine messaging system. The second acquisition, known as Dispense Labs LLC, was finalized and announced by Endexx on October 7, 2013. Dispense Labs has developed an advanced vending machine, known as Autospense, through its partnership with the leader in industrial vending inventory solutions, Autocrib, Inc. The Autospense machines have many built-in benefits and features to improve security, inventory management, profitability, efficiency, accountability and to mitigate risk. Endexx, through its wholly owned subsidiary, Dispense Labs, has secured exclusive worldwide rights for medical marijuana dispensing technology with Autocrib. Together, with M3Hub and the recent acquisition of THCFinder.com, these vending machine acquisitions will enable Endexx to provide a complete seed-to-sale solution to assist dispensaries, and other cannabis-related businesses, to work within the confines of the law. Additionally, it is expected that the THC Finder website will enable marijuana patients to locate the nearest dispensary with an Autospense marijuana vending machine.
Medbox Inc. is the industry leader in medical marijuana dispensing machines. They sell two machines for $50,000, one for edible marijuana products like brownies, and the other for portions of marijuana itself. As of October 2013, Medbox has sold approximately 160 marijuana vending machines to US medical marijuana dispensaries.
Tranzbyte Corp. plans to commence distribution of vending machines that use radio-frequency identification tags.
Pharmaceutical products
- Nabiximols (USAN, trade name Sativex) is an aerosolized mist for oral administration intended for the treatment of pain.
Reclassification in the USA
A number of medical organizations have endorsed reclassification of marijuana to allow for further study. These include, but are not limited to:
- The American Medical Association
- The American College of Physicians – America's second largest physicians group
- Leukemia & Lymphoma Society – America's second largest cancer charity
- American Academy of Family Physicians opposes the use of marijuana except under medical supervision
Other medical organizations recommend a halt to using marijuana as a medicine in U.S.
-
 United States cannabis laws. States with medical cannabis laws States with decriminalization laws States with both State with legalized cannabis
United States cannabis laws. States with medical cannabis laws States with decriminalization laws States with both State with legalized cannabis
History
Ancient China and Taiwan
Cannabis, called má 麻 (meaning "hemp; cannabis; numbness") or dàmá 大麻 (with "big; great") in Chinese, was used in Taiwan for fiber starting about 10,000 years ago. The botanist Li Hui-Lin wrote that in China, "The use of Cannabis in medicine was probably a very early development. Since ancient humans used hemp seed as food, it was quite natural for them to also discover the medicinal properties of the plant." The oldest Chinese pharmacopeia, the (ca. 100 CE) Shennong Bencaojing 神農本草經 ("Shennong's Materia Medica Classic"), describes dama "cannabis".
The flowers when they burst (when the pollen is scattered) are called 麻蕡 or 麻勃 . The best time for gathering is the seventh day of the seventh month. The seeds are gathered in the ninth month. The seeds which have entered the soil are injurious to man. It grows in (in ...). The flowers, the fruit (seed) and the leaves are officinal. The leaves and the fruit are said to be poisonous, but not the flowers and the kernels of the seeds.
Emperor Shen-Nung, who was also a pharmacologist, wrote a book on treatment methods in 2737 that included the medical benefits of cannabis. He recommended the substance for many ailments, including constipation, gout, rheumatism, and absent-mindedness. Hua Tuo lived many years later, yet he is credited with being the first person known to use cannabis as an anesthetic. He reduced the plant to powder and mixed it with wine for administration. In China, the era of Han Western, the 3rd century the great surgeon Hua Tuo conducts operations under anesthesia using Indian hemp. The Chinese term for anesthesia (麻醉: má zui ) is also composed of the ideogram which means hemp, followed by means of intoxication. Elizabeth Wayland Barber says the Chinese evidence "proves a knowledge of the narcotic properties of Cannabis at least from the 1st millennium B.C." when ma was already used in a secondary meaning of "numbness; senseless." "Such a strong drug, however, suggests that the Chinese pharmacists had now obtained from far to the southwest not THC-bearing Cannabis sativa but Cannabis indica, so strong it knocks you out cold.
Cannabis is one of the 50 "fundamental" herbs in traditional Chinese medicine, and is prescribed to treat diverse indications.
Every part of the hemp plant is used in medicine; the dried flowers (勃), the achenia (蕡), the seeds (麻仁), the oil (麻油), the leaves, the stalk, the root, and the juice. The flowers are recommended in the 120 different forms of (風 feng) disease, in menstrual disorders, and in wounds. The achenia, which are considered to be poisonous, stimulate the nervous system, and if used in excess, will produce hallucinations and staggering gait. They are prescribed in nervous disorders, especially those marked by local anaesthesia. The seeds, by which is meant the white kernels of the achenia, are used for a great variety of affections, and are considered to be tonic, demulcent, alterative, laxative, emmenagogue, diuretic, anthelmintic, and corrective. They are made into a congee by boiling with water, mixed with wine by a particular process, made into pills, and beaten into a paste. A very common mode of exhibition, however, is by simply eating the kernels. It is said that their continued use renders the flesh firm and prevents old age. They are prescribed internally in fluxes, post-partum difficulties, aconite poisoning, vermillion poisoning, constipation, and obstinate vomiting. Externally they are used for eruptions, ulcers, favus, wounds, and falling of the hair. The oil is used for falling hair, sulfur poisoning, and dryness of the throat. The leaves are considered to be poisonous, and the freshly expressed juice is used as an anthelmintic, in scorpion stings, to stop the hair from falling out and to prevent it from turning gray. They are especially thought to have antiperiodic properties (prevention of regular recurrence of the symptoms of a disease). The stalk, or its bark, is considered to be diuretic, and is used with other drugs in gravel. The juice of the root is used for similar purposes, and is also thought to have a beneficial action in retained placenta and post-partum hemorrhage. An infusion of hemp (for the preparation of which no directions are given) is used as a demulcent drink for quenching thirst and relieving fluxes.
Ancient Egypt

The Ebers Papyrus (ca. 1550 BCE) from Ancient Egypt describes medical cannabis. Other ancient Egyptian papyri that mention medical cannabis are the Ramesseum III Papyrus (1700 BC), the Berlin Papyrus (1300 BCE) and the Chester Beatty Medical Papyrus VI (1300 BCE). The ancient Egyptians even used hemp (cannabis) in suppositories for relieving the pain of hemorrhoids. Around 2,000 BCE, the ancient Egyptians used cannabis to treat sore eyes. The egyptologist Lise Manniche notes the reference to "plant medical cannabis" in several Egyptian texts, one of which dates back to the eighteenth century BCE.
Ramesseum III Papyrus (1700 BCE)
Main article: Ramesseum medical papyriPapyrus Ramassei III, col. 26:
| |
K.t phr.t: mɜt.t šmšm.t qnqn, sdr n ỉɜd.t, ỉ ỉr.ty n=s ỉm dwɜy
Alia praecepta: parsley, hemp and obey, in the dew of rest, wash eyes in that early in the morning
Ancient India
Cannabis was a major component in religious practices in ancient India as well as in medicinal practices. For many centuries, most parts of life in ancient India incorporated cannabis of some form. Surviving texts from ancient India confirm that cannabis' psychoactive properties were recognized, and doctors used it for treating a variety of illnesses and ailments. These included insomnia, headaches, a whole host of gastrointestinal disorders, and pain: cannabis was frequently used to relieve the pain of childbirth. One Indian philosopher expressed his views on the nature and uses of bhang (a form of cannabis), which combined religious thought with medical practices. "A guardian lives in the bhang leaf. …To see in a dream the leaves, plant, or water of bhang is lucky. …A longing for bhang foretells happiness. It cures dysentry and sunstroke, clears phlegm, quickens digestion, sharpens appetite, makes the tongue of the lisper plain, freshens the intellect and gives alertness to the body and gaiety to the mind. Such are the useful and needful ends for which in His goodness the Almighty made bhang."
Ancient Greece

The Ancient Greeks used cannabis to dress wounds and sores on their horses. In humans, dried leaves of cannabis were used to treat nose bleeds, and cannabis seeds were used to expel tapeworms. The most frequently described use of cannabis in humans was to steep green seeds of cannabis in either water or wine, later taking the seeds out and using the warm extract to treat inflammation and pain resulting from obstruction of the ear.
In the 5th century BCE Herodotus, a Greek historian, described how the Scythians of the Middle East used cannabis in steam baths. These baths drove the people to a frenzied state.
South East Asia
Patani from Asia are primary natural producers of the diuretic, antiemetic, antiepileptic, anti-inflammatory, pain killing and antipyretic properties of Cannabis sativa, and used it extensively for 'Kopi Kapuganja' and 'Pecel Ganja', as recreation food, drinks and relaxing medication for centuries.
Medieval Islamic world
In the medieval Islamic world, Arabic physicians made use of the diuretic, antiemetic, antiepileptic, anti-inflammatory, analgesic and antipyretic properties of Cannabis sativa, and used it extensively as medication from the 8th to 18th centuries.

Modern history

An Irish physician, William Brooke O'Shaughnessy, is credited with introducing the therapeutic use of cannabis to Western medicine. He was Assistant-Surgeon and Professor of Chemistry at the Medical College of Calcutta, and conducted a cannabis experiment in the 1830s, first testing his preparations on animals, then administering them to patients to help treat muscle spasms, stomach cramps or general pain.
Cannabis as a medicine became common throughout much of the Western world by the 19th century. In the 19th century was cannabis one of the secret ingredients in several so called patent medicines. There were at least 2000 cannabis medicines prior to 1937, produced by over 280 manufacturers. Cannabis was used as the primary pain reliever until the invention of aspirin. A Swedish lexicon printed in 1912 describes the cannabis drug and extract as a "deserted" method for medical treatment.
Modern medical and scientific inquiry began with doctors like O'Shaughnessy and Moreau de Tours, who used it to treat melancholia and migraines, and as a sleeping aid, analgesic and anticonvulsant. At the local level authorities introduced various laws that required the mixtures that contained cannabis, that was not sold on prescription, must be marked with warning labels under the so-called poison laws. In 1905 Samuel Hopkins Adams published an exposé entitled "The Great American Fraud" in Collier's Weekly about the patent medicines that led to the passage of the first Pure Food and Drug Act in 1906. This statute did not ban the alcohol, narcotics, and stimulants in the medicines; rather, it required medicinal products to be labeled as such and curbed some of the more misleading, overstated, or fraudulent claims that previously appeared on labels.
The product "Maltos-cannabis" was sold based upon a claim from its manufacturer that it contained maltose sugar from hemp seeds (maltose sugar can also be obtained from the process of softening and germinating grain in water). It is likely that Maltose-cannabis contained a very low percentage of THC.

Later in the century, researchers investigating methods of detecting cannabis intoxication discovered that smoking the drug reduced intraocular pressure. In 1955 the antibacterial effects were described at the Palacký University of Olomouc. Since 1971 Lumír Ondřej Hanuš was growing cannabis for his scientific research on two large fields in authority of the University. The marijuana extracts were then used at the University hospital as a cure for aphthae and haze. In 1973 physician Tod H. Mikuriya reignited the debate concerning cannabis as medicine when he published "Marijuana Medical Papers". High intraocular pressure causes blindness in glaucoma patients, so he hypothesized that using the drug could prevent blindness in patients. Many Vietnam War veterans also found that the drug prevented muscle spasms caused by spinal injuries suffered in battle. Later medical use focused primarily on its role in preventing the wasting syndromes and chronic loss of appetite associated with chemotherapy and AIDS, along with a variety of rare muscular and skeletal disorders.
In 1964, Dr. Albert Lockhart and Manley West began studying the health effects of traditional cannabis use in Jamaican communities. They discovered that Rastafarians had unusually low glaucoma rates and local fishermen were washing their eyes with cannabis extract in the belief that it would improve their sight. Lockhart and West developed, and in 1987 gained permission to market, the pharmaceutical Canasol: one of the first cannabis extracts. They continued to work with cannabis, developing more pharmaceuticals and eventually receiving the Jamaican Order of Merit for their work.
Later, in the 1970s, a synthetic version of THC was produced and approved for use in the United States as the drug Marinol. It was delivered as a capsule, to be swallowed. Patients complained that the violent nausea associated with chemotherapy made swallowing capsules difficult. Further, along with ingested cannabis, capsules are harder to dose-titrate accurately than smoked cannabis because their onset of action is so much slower. Smoking has remained the route of choice for many patients because its onset of action provides almost immediate relief from symptoms and because that fast onset greatly simplifies titration. For these reasons, and because of the difficulties arising from the way cannabinoids are metabolized after being ingested, oral dosing is probably the least satisfactory route for cannabis administration. Relatedly, some studies have indicated that at least some of the beneficial effects that cannabis can provide may derive from synergy among the multiplicity of cannabinoids and other chemicals present in the dried plant material. Such synergy is, by definition, impossible with respect to the use of single-cannabinoid drugs like Marinol.
During the 1970s and 1980s, six U.S. states' health departments performed studies on the use of medical cannabis. These are widely considered some of the most useful and pioneering studies on the subject. Voters in eight states showed their support for cannabis prescriptions or recommendations given by physicians between 1996 and 1999, including Alaska, Arizona, California, Colorado, Maine, Michigan, Nevada, Oregon, and Washington, going against policies of the federal government. In May 2001, "The Chronic Cannabis Use in the Compassionate Investigational New Drug Program: An Examination of Benefits and Adverse Effects of Legal Clinical Cannabis" (Russo, Mathre, Byrne et al.) was completed. This three-day examination of major body functions of four of the five living US federal cannabis patients found "mild pulmonary changes" in two patients.
Among the more than 108,000 persons in Colorado who in 2012 had received a certificate in Colorado of a doctor recommending them to use marijuana for medical purposes stated 94% severe pain be the reason for the requested certificate, 3% cancer and 1% HIV/Aids. The typical card holder was 41 year old man and that is not the normal pattern for patients with pain problems. 12 doctors had issued 50% of the certificates.
National and international regulations
Main article: Legal and medical status of cannabis
Medical use of cannabis or preparation containing THC as the active substance is legalized in Canada, Belgium, Austria, Netherlands, UK, Spain, Israel, Finland and some states in the U.S., although it is still illegal under U.S. federal law.
Cannabis is in Schedule IV of the United Nations' Single Convention on Narcotic Drugs, making it subject to special restrictions. Article 2 provides for the following, in reference to Schedule IV drugs:
A Party shall, if in its opinion the prevailing conditions in its country render it the most appropriate means of protecting the public health and welfare, prohibit the production, manufacture, export and import of, trade in, possession or use of any such drug except for amounts which may be necessary for medical and scientific research only, including clinical trials therewith to be conducted under or subject to the direct supervision and control of the Party.
The convention thus allows countries to outlaw cannabis for all non-research purposes but lets nations choose to allow medical and scientific purposes if they believe total prohibition is not the most appropriate means of protecting health and welfare. The convention requires that states that permit the production or use of medical cannabis must operate a licensing system for all cultivators, manufacturers and distributors and ensure that the total cannabis market of the state shall not exceed that required "for medical and scientific purposes."
African countries
Cannabis has been used in African countries since at least the 15th century. Its use was introduced by Arab traders, somehow connected to India. "In Africa, the plant was used for snake bite, to facilitate childbirth, malaria, fever, blood poisoning, anthrax, asthma, and dysentery." (Zuardi, 2006, 4) Though African governments have tried to limit and stop its use, it still seems to be deeply ingrained, mostly through religious rituals.
Austria
In Austria, both Δ-THC and pharmaceutical preparations containing Δ-THC are listed in annex V of the Narcotics Decree (Suchtgiftverordnung). Compendial formulations are manufactured upon prescription according to the German Neues Rezeptur-Formularium.
On 9 July 2008, the Austrian Parliament approved cannabis cultivation for scientific and medical uses. Cannabis cultivation is controlled by the Austrian Agency for Health and Food Safety (Österreichische Agentur für Gesundheit und Ernährungssicherheit, AGES).
Canada

In Canada, the regulation on access to cannabis for medical purposes, established by Health Canada in February 2000, defines two categories of patients eligible for access to medical cannabis. BC College of Physicians and Surgeons’ recommendation, as well as the CMPA position, is that physicians may prescribe cannabis if they feel comfortable with it. The MMAR forms are a confidential document between Health Canada, the physician and the patient. The information is not shared with the College or with the RCMP. No doctor has ever gone to court or faced prosecution for filling out a form or for prescribing medical cannabis. Category 1 covers any symptoms treated within the context of providing compassionate end-of-life care or the symptoms associated with different medical conditions. Category 2 is for applicants who have debilitating symptom(s) of medical condition(s), other than those described in Category 1. The application of eligible patients must be supported by a medical practitioner.
The cannabis distributed by Health Canada is provided under the brand CannaMed by the company Prairie Plant Systems Inc. In 2006, 420 kg of CannaMed cannabis was sold, representing an increase of 80% over the previous year. However, patients complain of the single strain selection as well as low potency, providing a pre-ground product put through a wood chipper (which deteriorates rapidly) as well as gamma irradation and foul taste and smell.
It is also legal for patients approved by Health Canada to grow their own cannabis for personal consumption, and it's possible to obtain a production license as a person designated by a patient. Designated producers were permitted to grow a cannabis supply for only a single patient. However, that regulation and related restrictions on supply were found unconstitutional by the Federal Court of Canada in January 2008. The court found that these regulations did not allow a sufficient legal supply of medical cannabis, and thus forced many patients to purchase their medicine from unauthorized, black market sources. This was the eighth time in the previous ten years that the courts ruled against Health Canada's regulations restricting the supply of the medicine. On 14 Dec 2012 the Canadian government announced plans to overhaul its rules regarding medical cannabis.
In Canada, there are four forms of medical cannabis. The first one is a cannabis extract called Sativex that contains THC and cannabidiol in a spray form. The second is a synthetic or manmade THC called dronabinol marketed as Marinol. The third also a synthetic version of THC called nabilone that is called Cesamet on the markets. The fourth product is the herbal form of cannabis often referred to as marijuana.
Czech Republic
Medical use of cannabis has been legal and regulated in the Czech Republic since April 1, 2013.
France
As of June 8, 2013, cannabis derivatives can be used in France for the manufacture of medicinal products. The products can only be obtained with a prescription and will only be prescribed when all other medications have failed to effectively relieve suffering. The amended legislation decriminalizes "the production, transport, export, possession, offering, acquisition or use of speciality pharmaceutials that contains one of these (cannabis-derivative) substances”, while all cannabis products must be approved by the National Medical Safety Agency (Agence nationale de sécurité du médicament – ANSM). A Pharmacists' Union spokesperson explained to the media that the change will make it more straightforward to conduct research into cannabinoids.
Germany
In February 2008, seven German patients could legally be treated with medicinal cannabis, distributed by prescription in pharmacies. To regulate therapeutic use, Germany modeled on Dutch neighbor who distributes this way since in 2003 (120 kg in 2008).
In Germany, dronabinol was rescheduled in 1994 from annex I to annex II of the Narcotics Law (Betäubungsmittelgesetz) in order to ease research; in 1998 dronabinol was rescheduled from annex II to annex III and since then has been available by prescription, whereas Δ-THC is still listed in annex I. Manufacturing instructions for dronabinol containing compendial formulations are described in the Neues Rezeptur-Formularium.
Israel

Marijuana for medical use has been permitted in Israel since the early 1990s for cancer patients and those with pain-related illnesses such as Parkinson's, multiple sclerosis, Crohn's Disease, other chronic pain and post-traumatic stress disorder. Patients can smoke the drug, ingest it in liquid form, or apply it to the skin as a balm. The numbers of patients authorized to use marijuana in Israel in 2012 is about 10,000.
There are eight government-sanctioned cannabis growing operations in Israel, which distribute it for medical purposes to patients who have a prescription from a doctor, via either a company's store, or in a medical center.
THC, the psychoactive chemical component in marijuana that causes a high, was first isolated by Israeli scientists Raphael Mechoulam of the Hebrew University in Jerusalem's Center for Research on Pain and Yechiel Gaoni of the Weizmann Institute in 1964.
The Tikkun Olam company has developed a variety of marijuana that is reported to provide the medical benefits of cannabis, but without THC. The cannabis instead contains high quantities of CBD, a substance that is believed to be an anti-inflammatory ingredient, which helps alleviate pain.
Netherlands
Since 2003, the country's pharmacies distribute medicinal cannabis (pharmaceutical form of the natural plant) by prescription, in addition to other drugs containing cannabinoids (dronabinol, Sativex).
Spain
In Spain, since the late 1990s and early 2000s, medical cannabis underwent a process of progressive decriminalization and legalisation. The parliament of the region of Catalonia was the first in Spain to have voted unanimously in 2001 legalizing medical marijuana; it was quickly followed by parliaments of Aragon and the Balearic Islands. The Spanish Penal Code prohibits the sale of cannabis but it does not prohibit consumption (although consumption on the street is fined). Until early 2000, the Penal Code did not distinguish between therapeutic use of cannabis and recreational use, however, several court decisions show that this distinction is increasingly taken into account by judges. From 2006, the sale of seed is legalized, the sale and public consumption remains illegal, and private cultivation and use are permitted to associations.
Several studies have been conducted to study the effects of cannabis on patients suffering from diseases like cancer, AIDS, multiple sclerosis, seizures or asthma. This research was conducted by various Spanish agencies at the Universidad Complutense de Madrid headed by Manuel Guzman, the hospital of La Laguna in Tenerife led neurosurgeon Luis González Feria or the University of Barcelona.
Several cannabis consumption clubs and user associations have been established throughout Spain. These clubs, the first of which was created in 1991, are non-profit associations who grow cannabis and sell it at cost to its members. The legal status of these clubs is uncertain: in 1997, four members of the first club, the Barcelona Ramón Santos Association of Cannabis Studies, were sentenced to 4 months in prison and a 3000 euro fine, while at about the same time, the court of Bilbao ruled that another club was not in violation of the law. The Andalusian regional government also commissioned a study by criminal law professors on the "Therapeutic use of cannabis and the creation of establishments of acquisition and consumption. The study concluded that such clubs are legal as long as they distribute only to a restricted list of legal adults, provide only the amount of drugs necessary for immediate consumption, and not earn a profit. The Andalusian government never formally accepted these guidelines and the legal situation of the clubs remains insecure. In 2006 and 2007, members of these clubs were acquitted in trial for possession and sale of cannabis and the police were ordered to return seized crops.
United Kingdom
In England and Wales, the use of cannabis medicinally is accepted as a mitigating factor under Sentencing Council guidelines, if it is being cultivated or found in possession of someone. However, in the United Kingdom, possession of small quantities of cannabis does not usually warrant an arrest or court appearance (street cautions or fines are often given out instead). Under UK law, certain cannabinoids are permitted medically, but these are strictly controlled with many provisos under the Misuse of Drugs Act 1971 (in the 1985 amendments).
The British Medical Association's official stance is "users of cannabis for medical purposes should be aware of the risks, should enrol for clinical trials, and should talk to their doctors about new alternative treatments; but we do not advise them to stop."
United States
Main article: Medical cannabis in the United States

In the United States, cannabis per se has been criminalized at the Federal level by implementation of the Controlled Substances Act, which classifies cannabis as a Schedule I drug – the strictest classification, on par with heroin, LSD and ecstasy. In 2005, the U.S. Supreme Court ruled in Gonzales v. Raich that the Commerce Clause of the U.S. Constitution allows the government to ban any use of cannabis, including medical use. The United States Food and Drug Administration states "marijuana has a high potential for abuse, has no currently accepted medical use in treatment in the United States, and has a lack of accepted safety for use under medical supervision".
Two American (for-profit) companies, Cannabis Science Inc., and Medical Marijuana, Inc., are working towards getting FDA approval for cannabis based medicines (including smoked cannabis). Cannabis Science Inc. wants to have medical cannabis approved by the FDA so anyone, regardless of state, will have access to the medicine. Also, there is one non-profit organization, the Multidisciplinary Association for Psychedelic Studies (MAPS) working towards getting Cannabis approved by the FDA for PTSD.
Since the medical marijuana movement began, nineteen states and the District of Columbia, starting with California in 1996, have legalized medical cannabis or effectively decriminalized it: Alaska, Arizona, California, Colorado, Connecticut, Delaware, Hawaii, Maine, Massachusetts, Michigan, Montana, Nevada, New Hampshire, New Jersey, New Mexico, Oregon, Rhode Island, Vermont, Washington; Maryland allows for reduced or no penalties if cannabis use has a medical basis. Despite legalization of marijuana in Washington and Colorado, an employee may still be fired if they test positive on a drug test, despite having a doctor's recommendation. California, Colorado, New Mexico, Maine, Rhode Island, Montana, and Michigan are currently the only states to utilize dispensaries to sell medical cannabis; Connecticut and Massachusetts are also planning to do so. During 2008, California's medical cannabis industry took in about $2 billion and generated $100 million in state sales taxes with an estimated 2,100 dispensaries, co-operatives, wellness clinics and taxi delivery services in the sector colloquially known as "cannabusiness".
Though it does not have an established medical registry program, the state of Virginia, does allow for possession under the directive as medicine.
Some individual states such as Oregon choose to issue medical marijuana cards to residents with a doctors recommendation after paying a fee.
In October 2009, the U.S. Deputy Attorney General issued a U.S. Department of Justice memorandum to "All United States Attorneys" providing clarification and guidance to federal prosecutors in states that have enacted medical marijuana laws. The document is intended solely as "a guide to the exercise of investigative and prosecutorial discretion and as guidance on resource allocation and federal priorities." It includes seven criteria to help determine whether a patient's use, or their caregiver's provision, of medical cannabis "represents part of a recommended treatment regiment consistent with applicable state law". The Department advised that it "likely was not an efficient use of federal resources to focus enforcement efforts on seriously ill individuals, or on their individual caregivers. ... Large-scale, for-profit commercial enterprises, on the other , ... continued to be appropriate targets for federal enforcement and prosecution."
The sale and distribution of cannabis remains illegal under federal law, however, as the Food and Drug Administration's position – that marijuana has no accepted value in the treatment of any disease in the United States – remains unchanged.
The National Institutes of Health holds a patent for medical cannabis. The patent, "Cannabinoids as antioxidants and neuroprotectants", issued October 2003 reads:
Cannabinoids have been found to have antioxidant properties, unrelated to NMDA receptor antagonism. This new found property makes cannabinoids useful in the treatment and prophylaxis of wide variety of oxidation associated diseases, such as ischemic, age-related, inflammatory and autoimmune diseases. The cannabinoids are found to have particular application as neuroprotectants, for example in limiting neurological damage following ischemic insults, such as stroke and trauma, or in the treatment of neurodegenerative diseases, such as Alzheimer's disease, Parkinson's disease and HIV dementia... .
In November 2011, in accordance with 35 U.S.C. 209(c)(1) and 37 CFR part 404.7(a)(1)(i), the NIH announced that it is contemplating the grant of an exclusive patent license to practice the invention embodied therein to KannaLife Sciences Inc.. The prospective exclusive license territory may be worldwide, and the field of use may be limited to: The development and sale of cannabinoid(s) and cannabidiol(s) based therapeutics as antioxidants and neuroprotectants for use and delivery in humans, for the treatment of hepatic encephalopathy, as claimed in the Licensed Patent Rights.
See also
References
- ^ Ben Amar, Mohamed (2006). "Cannabinoids in medicine: A review of their therapeutic potential". Journal of Ethnopharmacology. 105 (1–2): 1–25. doi:10.1016/j.jep.2006.02.001. PMID 16540272.
- ^ Wong, Ming (1976). La Médecine chinoise par les plantes. Paris: Tchou. OCLC 2646789.
- American Society of Addiction Medicine: State-Level Proposals to Legalize Marijuana, July 25, 2012
- The Myth of “Medical Marijuana”, Scholastic Inc, 2012
- "What are the differences between Cannabis indica and Cannabis sativa, and how do they vary in their potential medical utility?". ProCon.org.
- Johns, A. (2001). "Psychiatric effects of cannabis". The British Journal of Psychiatry. 178 (2): 116. doi:10.1192/bjp.178.2.116.
- ^ J.E. Joy, S. J. Watson, Jr., and J.A. Benson, Jr, (1999). Marijuana and Medicine: Assessing The Science Base. Washington D.C: National Academy of Sciences Press. ISBN 0-585-05800-8.
{{cite book}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - "Indica? Sativa? What's the difference?". Growery. Retrieved 17 February 2011.
- Clark, Peter A.; Capuzzi, Kevin; Fick, Cameron (2011). "Medical marijuana: Medical necessity versus political agenda". Medical Science Monitor. 17 (12): RA249–61. doi:10.12659/MSM.882116. PMC 3628147. PMID 22129912.
- Aggarwal, SK; Carter, GT; Sullivan, MD; Zumbrunnen, C; Morrill, R; Mayer, JD (2009). "Medicinal use of cannabis in the United States: Historical perspectives, current trends, and future directions". Journal of opioid management. 5 (3): 153–68. PMID 19662925.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - "IACM 5th Conference on Cannabinoids in Medicine" (PDF). International Association for Cannabis as Medicine. Retrieved 28 July 2011.
- Joy, Janet E.; Watson, Stanley J.; Benson, John A., eds. (1999). Marijuana and Medicine: Assessing the Science Base. Washington, D.C.: National Academies Press. p. 13. ISBN 978-0-309-07155-0. OCLC 246585475.
- ^ "Workshop on the Medical Utility of Marijuana". National Institutes of Health. 1997. Retrieved 26 April 2009.
- cannabismd.net. cannabismd.net. Retrieved on 2013-04-17.
- Medical Marijuana | Strains. Canadamedicalmarijuana.com. Retrieved on 2013-04-17.
- "Cannabis and Cannabinoids (PDQ®)". National Cancer Institute at the National Institutes of Health. NIH…Turning Discovery Into Health®. 2 August 2013. Retrieved 24 August 2013.
- Victoria Colliver (18 September 2012). "Pot compound seen as tool against cancer". San Francisco Chronicle. Retrieved 24 August 2013.
- BRADENTON HERALD EDITORIAL (16 August 2013). "CNN's Dr. Sanjay Gupta finds ample evidence of benefits of medical marijuana". Bradenton Herald. Retrieved 24 August 2013.
- Mark Mathew Braunstein (2010). "The Sixth National Clinical Conference on Cannabis Therapeutics: A Report on the 2010 Conference" (PDF) (23, 2010). Treating Yourself.
He is one of only four remaining patients whose cannabis is still provided by the federal government under its now disbanded Investigational New Drug (IND) program.
{{cite journal}}: Cite journal requires|journal=(help) - Grotenhermen, Franjo (2002). "Review of Therapeutic Effects". Cannabis and Cannabinoids: Pharmacology, Toxicology and Therapeutic Potential. New York City: Haworth Press. p. 124. ISBN 978-0-7890-1508-2.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - Russo, EB (2004). "Clinical endocannabinoid deficiency (CECD): Can this concept explain therapeutic benefits of cannabis in migraine, fibromyalgia, irritable bowel syndrome and other treatment-resistant conditions?". Neuro endocrinology letters. 25 (1–2): 31–9. PMID 15159679.
- Zajicek, John; Fox, Patrick; Sanders, Hilary; Wright, David; Vickery, Jane; Nunn, Andrew; Thompson, Alan (2003). "Cannabinoids for treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): Multicentre randomised placebo-controlled trial". The Lancet. 362 (9395): 1517. doi:10.1016/S0140-6736(03)14738-1.
- "Spinal Cord Injury and Disease". Therapeutic Uses of Marijuana. Medical Marijuana Information Resource Centre. Retrieved 9 August 2009.
- Maurer, M.; Henn, V.; Dittrich, A.; Hofmann, A. (1990). "Delta-9-tetrahydrocannabinol shows antispastic and analgesic effects in a single case double-blind trial". European Archives of Psychiatry and Clinical Neuroscience. 240 (1): 1–4. doi:10.1007/BF02190083. PMID 2175265.
- Kogel, Robert W.; Johnson, Paul B.; Chintam, Rani; Robinson, Charles J.; Nemchausky, Bernard A. (1995). "Treatment of Spasticity in Spinal Cord Injury with Dronabinol, A Tetrahydrocannabinol Derivative". American Journal of Therapeutics. 2 (10): 799–805. doi:10.1097/00045391-199510000-00012. PMID 11854790.
- Hagenbach, U; Luz, S; Ghafoor, N; Berger, J M; Grotenhermen, F; Brenneisen, R; Mäder, M (2006). "The treatment of spasticity with Δ9-tetrahydrocannabinol in persons with spinal cord injury". Spinal Cord. 45 (8): 551–62. doi:10.1038/sj.sc.3101982. PMID 17043680.
- ^ Mack, Allyson (2001). Marijuana as Medicine?: The Science Beyond the Controversy. National Academy Press. ISBN 0309065313.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Thanos PK, Dimitrakakis ES, Rice O, Gifford A, Volkow ND (2005). "Ethanol self-administration and ethanol conditioned place preference are reduced in mice lacking cannabinoid CB1 receptors". Behavioural Brain Research. 164 (2): 206–13. doi:10.1016/j.bbr.2005.06.021. PMID 16140402.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Carter GT, Rosen BS (2001). "Marijuana in the management of amyotrophic lateral sclerosis". The American Journal of Hospice & Palliative Care. 18 (4): 264–70. doi:10.1177/104990910101800411. PMID 11467101.
- Weydt P, Hong S, Witting A, Möller T, Stella N, Kliot M (2005). "Cannabinol delays symptom onset in SOD1 (G93A) transgenic mice without affecting survival". Amyotrophic Lateral Sclerosis and Other Motor Neuron Disorders. 6 (3): 182–4. doi:10.1080/14660820510030149. PMID 16183560.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Malfait AM; Gallily R; Sumariwalla PF; Malik, AS; Andreakos, E; Mechoulam, R; Feldmann, M (2000). "The nonpsychoactive cannabis constituent cannabidiol is an oral anti-arthritic therapeutic in murine collagen-induced arthritis". Proceedings of the National Academy of Sciences of the United States of America. 97 (17): 9561–6. Bibcode:2000PNAS...97.9561M. doi:10.1073/pnas.160105897. PMC 16904. PMID 10920191.
- Tashkin DP, Shapiro BJ, Lee YE, Harper CE (1975). "Effects of smoked marijuana in experimentally induced asthma". The American Review of Respiratory Disease. 112 (3): 377–86. PMID 1099949.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Steffens S; Veillard NR; Arnaud C; Pelli, Graziano; Burger, Fabienne; Staub, Christian; Zimmer, Andreas; Frossard, Jean-Louis; Mach, François (16 April 2005). "Cannabis may help keep arteries clear". Nature. 434 (7034): 782–6. Bibcode:2005Natur.434..782S. doi:10.1038/nature03389. PMID 15815632.
{{cite journal}}:|first10=missing|last10=(help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - Grinspoon L, Bakalar JB (1998). "The use of cannabis as a mood stabilizer in bipolar disorder: anecdotal evidence and the need for clinical research". Journal of Psychoactive Drugs. 30 (2): 171–7. doi:10.1080/02791072.1998.10399687. PMID 9692379.
- Ashton CH, Moore PB, Gallagher P, Young AH (2005). "Cannabinoids in bipolar affective disorder: a review and discussion of their therapeutic potential". Journal of Psychopharmacology. 19 (3): 293–300. doi:10.1177/0269881105051541. PMID 15888515.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Patsos HA; Hicks DJ; Dobson RR; Greenhough, A; Woodman, N; Lane, JD; Williams, AC; Paraskeva, C (2005). "The endogenous cannabinoid, anandamide, induces cell death in colorectal carcinoma cells: a possible role for cyclooxygenase 2". Gut. 54 (12): 1741–50. doi:10.1136/gut.2005.073403. PMC 1774787. PMID 16099783.
- Abrams, D.I., MD (2007). "Cannabis in painful HIV-Associated Sensory Neuropathy". Neurology. 68 (7): 515–521. doi:10.1212/01.wnl.0000253187.66183.9c. PMID 17296917. Retrieved 2/3/2011.
{{cite journal}}: Check date values in:|accessdate=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: multiple names: authors list (link) - Bambico FR, Katz N, Debonnel G, Gobbi G (2007). "Cannabinoids elicit antidepressant-like behavior and activate serotonergic neurons through the medial prefrontal cortex". The Journal of Neuroscience. 27 (43): 11700–11. doi:10.1523/JNEUROSCI.1636-07.2007. PMID 17959812.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Denson, Thomas F.; Earleywine, Mitchell (2006). "Decreased depression in marijuana users". Addictive Behaviors. 31 (4): 738–42. doi:10.1016/j.addbeh.2005.05.052. PMID 15964704.
- Jiang, W.; Zhang, Y; Xiao, L; Van Cleemput, J; Ji, SP; Bai, G; Zhang, X (2005). "Cannabinoids promote embryonic and adult hippocampus neurogenesis and produce anxiolytic- and antidepressant-like effects". Journal of Clinical Investigation. 115 (11): 3104–16. doi:10.1172/JCI25509. PMC 1253627. PMID 16224541.
- El-Remessy, Azza B.; Al-Shabrawey, Mohamed; Khalifa, Yousuf; Tsai, Nai-Tse; Caldwell, Ruth B.; Liou, Gregory I. (2006). "Neuroprotective and Blood-Retinal Barrier-Preserving Effects of Cannabidiol in Experimental Diabetes". The American Journal of Pathology. 168 (1): 235–44. doi:10.2353/ajpath.2006.050500. PMC 1592672. PMID 16400026.
- Fox, Susan H.; Kellett, Mark; Moore, A. Peter; Crossman, Alan R.; Brotchie, Jonathan M. (2002). "Randomised, double-blind, placebo-controlled trial to assess the potential of cannabinoid receptor stimulation in the treatment of dystonia". Movement Disorders. 17 (1): 145–9. doi:10.1002/mds.1280. PMID 11835452.
- Gray, Richard (10 April 2011). "Cannabis could be used to treat epilepsy". The Daily Telegraph. Retrieved 20 April 2011.
- Marsicano, G.; Goodenough, S; Monory, K; Hermann, H; Eder, M; Cannich, A; Azad, SC; Cascio, MG; Gutiérrez, SO; Van Der Stelt, M; López-Rodriguez, ML; Casanova, E; Schütz, G; Zieglgänsberger, W; Di Marzo, V; Behl, C; Lutz, B (2003). "CB1 Cannabinoid Receptors and On-Demand Defense Against Excitotoxicity". Science. 302 (5642): 84–8. doi:10.1126/science.1088208. PMID 14526074.
- Bacci A, Huguenard JR, Prince DA (2004). "Long-lasting self-inhibition of neocortical interneurons mediated by endocannabinoids". Nature. 431 (7006): 312–6. Bibcode:2004Natur.431..312B. doi:10.1038/nature02913. PMID 15372034.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - Di Carlo G, Izzo AA (2003). "Cannabinoids for gastrointestinal diseases: potential therapeutic applications". Expert Opinion on Investigational Drugs. 12 (1): 39–49. doi:10.1517/13543784.12.1.39. PMID 12517253.
- Lorente M; Carracedo A; Torres S; Natali, Francesco; Egia, Ainara; Hernández-Tiedra, Sonia; Salazar, María; Blázquez, Cristina; Guzmán, Manuel (2009). "Amphiregulin is a factor for resistance of glioma cells to cannabinoid-induced apoptosis". Glia. 57 (13): 1374–85. doi:10.1002/glia.20856. PMID 19229996.
{{cite journal}}:|first10=missing|last10=(help) - Ramer R, Hinz B (2008). "Inhibition of cancer cell invasion by cannabinoids via increased expression of tissue inhibitor of matrix metalloproteinases-1". Journal of the National Cancer Institute. 100 (1): 59–69. doi:10.1093/jnci/djm268. PMID 18159069.
- Sylvestre DL, Clements BJ, Malibu Y (2006). "Cannabis use improves retention and virological outcomes in patients treated for hepatitis C". European Journal of Gastroenterology & Hepatology. 18 (10): 1057–63. doi:10.1097/01.meg.0000216934.22114.51. PMID 16957511.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Iuvone, T; Esposito, G; De Filippis, D; Scuderi, C; Steardo, L (2009). "Cannabidiol: A promising drug for neurodegenerative disorders?". CNS neuroscience & therapeutics. 15 (1): 65–75. doi:10.1111/j.1755-5949.2008.00065.x. PMID 19228180.
- Scotter, EL; Goodfellow, CE; Graham, ES; Dragunow, M; Glass, M (2010). "Neuroprotective potential of CB1 receptor agonists in an in vitro model of Huntington's disease". British journal of pharmacology. 160 (3): 747–61. doi:10.1111/j.1476-5381.2010.00773.x. PMC 2931573. PMID 20590577.
- Powles T; te Poele R; Shamash J; Chaplin, T; Propper, D; Joel, S; Oliver, T; Liu, WM (2005). "Cannabis-induced cytotoxicity in leukemic cell lines: the role of the cannabinoid receptors and the MAPK pathway". Blood. 105 (3): 1214–21. doi:10.1182/blood-2004-03-1182. PMID 15454482.
- Casanova ML; Blázquez C; Martínez-Palacio J; Villanueva, Concepción; Fernández-Aceñero, M. Jesús; Huffman, John W.; Jorcano, José L.; Guzmán, Manuel (2003). "Inhibition of skin tumor growth and angiogenesis in vivo by activation of cannabinoid receptors". The Journal of Clinical Investigation. 111 (1): 43–50. doi:10.1172/JCI16116. PMC 151833. PMID 12511587.
- Appendino G, Gibbons S, Giana A, Pagani A, Grassi G, Stavri M, Smith E, Rahman MM (2008). "Antibacterial Cannabinoids from Cannabis sativa: A Structure—Activity Study". J Nat Prod. 71 (8): 1427–30. doi:10.1021/np8002673. PMID 18681481.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - Kreitzer AC, Malenka RC (2005). "Endocannabinoid-mediated rescue of striatal LTD and motor deficits in Parkinson's disease models". Nature. 445 (7128): 643–7. doi:10.1038/nature05506. PMID 17287809.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - Szepietowski JC, Szepietowski T, Reich A (2005). "Efficacy and tolerance of the cream containing structured physiological lipids with endocannabinoids in the treatment of uremic pruritus: a preliminary study". Acta Dermatovenerologica Croatica. 13 (2): 97–103. PMID 16324422.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Bergasa NV (2005). "The pruritus of cholestasis". Journal of Hepatology. 43 (6): 1078–88. doi:10.1016/j.jhep.2005.09.004. PMID 16253381.
- Ganon-Elazar E, Akirav I (2009). "Cannabinoid receptor activation in the basolateral amygdala blocks the effects of stress on the conditioning and extinction of inhibitory avoidance". J. Neurosci. 29 (36): 11078–88. doi:10.1523/JNEUROSCI.1223-09.2009. PMID 19741114.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - Wilkinson, JD; Williamson, EM (2007). "Cannabinoids inhibit human keratinocyte proliferation through a non-CB1/CB2 mechanism and have a potential therapeutic value in the treatment of psoriasis". Journal of dermatological science. 45 (2): 87–92. doi:10.1016/j.jdermsci.2006.10.009. PMID 17157480.
- Howard, J; Anie, KA; Holdcroft, A; Korn, S; Davies, SC (2005). "Cannabis use in sickle cell disease: A questionnaire study". British journal of haematology. 131 (1): 123–8. doi:10.1111/j.1365-2141.2005.05723.x. PMID 16173972.
- Carley DW, Paviovic S, Janelidze M, Radulovacki M (2002). "Functional role for cannabinoids in respiratory stability during sleep". Sleep. 25 (4): 391–8. PMID 12071539.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Grotenhermen, Russo (2002) "Review of Therapeutic Effects." Chapter 11, p. 128 in Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential, Routledge, ISBN 0789015080.
- Singer HS (2005). "Tourette's syndrome: from behaviour to biology". Lancet Neurol. 4 (3): 149–59. doi:10.1016/S1474-4422(05)01012-4. PMID 15721825.
- Robertson MM (2000). "Tourette syndrome, associated conditions and the complexities of treatment". Brain: a journal of neurology. 123 (3): 425–62. doi:10.1093/brain/123.3.425. PMID 10686169.
- Sandyk R, Awerbuch G (1988). "Marijuana and Tourette's syndrome". Journal of Clinical Psychopharmacology. 8 (6): 444–5. doi:10.1097/00004714-198812000-00021. PMID 3235704.
- Müller-Vahl KR, Kolbe H, Dengler R (1997). "Gilles de la Tourette syndrome. Effect of nicotine, alcohol and marihuana on clinical symptoms". Der Nervenarzt. 68 (12): 985–9. PMID 9465342.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Reinarman, C; Nunberg, H; Lanthier, F; Heddleston, T (2011). "Who Are Medical Marijuana Patients? Population Characteristics from Nine California Assessment Clinics". Journal of Psychoactive Drugs. 43 (2): 128–135. doi:10.1080/02791072.2011.587700. PMID 21858958.
- Hall, Wayne; Solowij, Nadia (1998). "Adverse effects of cannabis". The Lancet. 352 (9140): 1611. doi:10.1016/S0140-6736(98)05021-1.
- Grinspoon, Lester (23 September 2012). "Grinspoon: Marijuana is here to stay". The MetroWest Daily News. Retrieved 7 January 2013Template:Inconsistent citations
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: postscript (link) - ^ Jones, R T (2002). "Cardiovascular system effects of marijuana". Journal of Clinical Pharmacology. 42 (11): 58–63. Retrieved 31 January 2013.
- Aranya, A (2007). "Marijuana as a trigger of cardiovascular events: Speculation or scientific certainty?". International Journal of Cardiology. 118 (2): 141–147. doi:10.1016/j.ijcard.2006.08.001.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - JAMA Network | JAMA | Association Between Marijuana Exposure and Pulmonary Function Over 20 Years
- Gumbiner, Jann (17 February 2011). "Does Marijuana Cause Cancer?". Psychology Today. Retrieved 9 January 2013.
{{cite journal}}: Cite journal requires|journal=(help) - "Does smoking cannabis cause cancer?". Cancer Research UK. 20 September 2010. Retrieved 9 January 2013.
{{cite journal}}: Cite journal requires|journal=(help) - Tashkin, Donald (1997). "Effects of marijuana on the lung and its immune defenses". UCLA School of Medicine. Retrieved 23 June 2012.
{{cite journal}}: Cite journal requires|journal=(help); Unknown parameter|month=ignored (help) - "Chemicals known to the state to cause cancer or reproductive toxicity" (PDF). ca.gov. 20 July 2012. Retrieved 8 January 2013.
- Hashibe, M; Morgenstern, H; Cui, Y; Tashkin, DP; Zhang, ZF; Cozen, W; Mack, TM; Greenland, S (2006). "Marijuana use and the risk of lung and upper aerodigestive tract cancers: Results of a population-based case-control study". Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 15 (10): 1829–34. doi:10.1158/1055-9965.EPI-06-0330. PMID 17035389.
- Francis L. Young. Druglibrary.org (1988-09-06). Retrieved on 2013-04-17.
- "Marijuana chemical chills out brain's pain threshold". News.discovery.com. 21 December 2012. Retrieved 7 January 2013Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - Pedersen, Traci (29 December 2012). "Marijuana pain relief varies among users". Psychcentral.com. Retrieved 7 January 2013Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - Anne Harding (22 February 2010). "Medical marijuana may help fibromyalgia pain". CNN. Retrieved 7 January 2013Template:Inconsistent citations
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: postscript (link) - Goodwin, Jenifer (3 September 2010). "Marijuana may relieve nerve pain when other drugs don't". USA Today. Retrieved 7 January 2013Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - "Marijuana provides pain relief, new study says". Huffington Post. 18 February 2010. Retrieved 7 January 2013Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - Kim, Leland (6 December 2011). "UCSF study finds medical marijuana could help patients reduce pain with opiates". ucsf.edu. Retrieved 7 January 2013Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - Sunanda Creagh (23). "Study of daily users shows marijuana pills trump smoked marijuana for pain relief". The Conversation Australia. The Conversation Media Group. Retrieved 24 April 2013.
{{cite web}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|month=ignored (help) - ^ Grotenhermen, Franjo; Müller-Vahl, Kirsten (2012). "The Therapeutic Potential of Cannabis and Cannabinoids". Deutsches Ärzteblatt International. 109 (29–30): 495–501. doi:10.3238/arztebl.2012.0495. PMC 3442177. PMID 23008748.
- Bowles, Daniel W.; o’Bryant, Cindy L.; Camidge, D. Ross; Jimeno, Antonio (2012). "The intersection between cannabis and cancer in the United States". Critical Reviews in Oncology/Hematology. 83: 1. doi:10.1016/j.critrevonc.2011.09.008.
- ^ Wang, T.; Collet, J.-P.; Shapiro, S.; Ware, M. A. (2008). "Adverse effects of medical cannabinoids: A systematic review". Canadian Medical Association Journal. 178 (13): 1669–78. doi:10.1503/cmaj.071178. PMC 2413308. PMID 18559804.
- Jordan, K.; Sippel, C.; Schmoll, H.-J. (2007). "Guidelines for Antiemetic Treatment of Chemotherapy-Induced Nausea and Vomiting: Past, Present, and Future Recommendations". The Oncologist. 12 (9): 1143–50. doi:10.1634/theoncologist.12-9-1143. PMID 17914084.
- Joy, Janet E.; Watson, Stanley J.; Benson, John A., eds. (1999). Marijuana and Medicine: Assessing the Science Base. Washington, D.C.: National Academies Press. ISBN 978-0-309-07155-0. OCLC 246585475.
- Kaufman, Paul. (1998). "Marijuana and Glaucoma". Archives of Ophthalmology. 116 (11): 1512–13. doi:10.1001/archopht.116.11.1512.
- Henry Jampel. "POSITION STATEMENT ON Marijuana and the Treatment of Glaucoma". American Glaucoma Society. Retrieved 13 August 2013.
- ^ Lakhan SE, Rowland M (2009). "Whole plant cannabis extracts in the treatment of spasticity in multiple sclerosis: a systematic review". BMC Neurology. 9: 59. doi:10.1186/1471-2377-9-59. PMC 2793241. PMID 19961570.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Green, Anita J; De-Vries, Kay (2010). "Cannabis use in palliative care - an examination of the evidence and the implications for nurses". Journal of Clinical Nursing. 19 (17–18): 2454–62. doi:10.1111/j.1365-2702.2010.03274.x. PMID 20920073.
- ^ AMA meeting: Delegates support review of cannabis's schedule I status; A change could make it easier for researchers to test potential medical uses and develop a drug delivery form safer than smoking. By Kevin B. O'Reilly, American Medical News. 30 November 2009
- Eubanks LM; Rogers CJ; Beuscher AE; Koob, George F.; Olson, Arthur J.; Dickerson, Tobin J.; Janda, Kim D. (2006). "A Molecular Link Between the Active Component of Marijuana and Alzheimer's Disease Pathology". Molecular Pharmaceutics. 3 (6): 773–7. doi:10.1021/mp060066m. PMC 2562334. PMID 17140265.
- Campbell, V A; Gowran, A (2009). "Alzheimer's disease; taking the edge off with cannabinoids?". British Journal of Pharmacology. 152 (5): 655–62. doi:10.1038/sj.bjp.0707446. PMC 2190031. PMID 17828287.
- ^ Alzheimer's Research Trust
- Alzheimer's Society
- Szalavitz, Maia. (2012-10-29) How Cannabinoids May Slow Brain Aging | TIME.com. Healthland.time.com. Retrieved on 2013-04-17.
- The endocannabinoid system in normal and pathological brain ageing. Rstb.royalsocietypublishing.org (2012-12-05). Retrieved on 2013-04-17.
- ^ McAllister SD, Christian RT, Horowitz MP, Garcia A, Desprez PY (2007). "Cannabidiol as a novel inhibitor of Id-1 gene expression in aggressive breast cancer cells". Molecular Cancer Therapeutics. 6 (11): 2921–7. doi:10.1158/1535-7163.MCT-07-0371. PMID 18025276.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ^ McAllister SD, Murase R, Christian RT; et al. (22 September 2010). "Pathways mediating the effects of cannabidiol on the reduction of breast cancer cell proliferation, invasion, and metastasis". Breast Cancer Res Treat. 129 (1): 37–47. doi:10.1007/s10549-010-1177-4. PMC 3410650. PMID 20859676.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Claire Bates (20 September 2012). "Cannabis compound could stop breast cancer from spreading". Daily Mail. Retrieved 25 December 2012Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - Victoria Colliver (18 September 2012). "Pot compound seen as tool against cancer". San Francisco Chronicle. Retrieved 25 December 2012Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - Haney M; Gunderson EW; Rabkin J; Hart, Carl L; Vosburg, Suzanne K; Comer, Sandra D; Foltin, Richard W (2007). "Dronabinol and marijuana in HIV-positive marijuana smokers. Caloric intake, mood, and sleep". Journal of Acquired Immune Deficiency Syndromes. 45 (5): 545–54. doi:10.1097/QAI.0b013e31811ed205. PMID 17589370.
- Abrams DI; Hilton JF; Leiser RJ; Bacchetti, SB; Mccune, TA; Schambelan, FT; Benowitz, NL; Bredt, BM; Kosel, B; Mitchell, TF; Mulligan, K (2003). "Short-term effects of cannabinoids in patients with HIV-1 infection: a randomized, placebo-controlled clinical trial". Annals of Internal Medicine. 139 (4): 258–66. doi:10.7326/0003-4819-139-4-200308190-00008. PMID 12965981.
{{cite journal}}:|first10=missing|last10=(help);|first11=missing|last11=(help);|first14=missing|last14=(help);|first15=missing|last15=(help);|first16=missing|last16=(help) - Ellis RJ; Toperoff W; Vaida F; Van Den Brande, Geoffrey; Gonzales, James; Gouaux, Ben; Bentley, Heather; Atkinson, J Hampton (2009). "Smoked Medicinal Cannabis for Neuropathic Pain in HIV: A Randomized, Crossover Clinical Trial". Neuropsychopharmacology. 34 (3): 672–80. doi:10.1038/npp.2008.120. PMC 3066045. PMID 18688212.
- Abrams DI; Jay CA; Shade SB; Vizoso, H.; Reda, H.; Press, S.; Kelly, M. E.; Rowbotham, M. C.; Petersen, K. L. (2007). "Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial". Neurology. 68 (7): 515–21. doi:10.1212/01.wnl.0000253187.66183.9c. PMID 17296917.
- Phillips TJ, Cherry CL, Cox S, Marshall SJ, Rice AS (2010). Pai, Nitika Pant (ed.). "Pharmacological Treatment of Painful HIV-Associated Sensory Neuropathy: A Systematic Review and Meta-Analysis of Randomised Controlled Trials". PLoS ONE. 5 (12): e14433. Bibcode:2010PLoSO...514433P. doi:10.1371/journal.pone.0014433. PMC 3010990. PMID 21203440.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Salazar M; Carracedo A; Salanueva IJ; Cecconi, Sonia; Pandolfi, Mar; González-Feria, Ainara; Iovanna, Patricia; Guzmán, Cristina; Boya, Sofía; Fimia, GM; Piacentini, M; Velasco, G (2009). "Cannabinoid action induces autophagy-mediated cell death through stimulation of ER stress in human glioma cells". The Journal of Clinical Investigation. 119 (5): 1359–72. doi:10.1172/JCI37948. PMC 2673842. PMID 19425170.
{{cite journal}}:|first10=missing|last10=(help);|first11=missing|last11=(help);|first14=missing|last14=(help);|first15=missing|last15=(help);|first16=missing|last16=(help);|first17=missing|last17=(help);|first18=missing|last18=(help);|first19=missing|last19=(help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - ^ Morel LJ, Giros B, Daugé V (2009). "Adolescent Exposure to Chronic Delta-9-Tetrahydrocannabinol Blocks Opiate Dependence in Maternally Deprived Rats". Neuropsychopharmacology. 34 (11): 2469–76. doi:10.1038/npp.2009.70. PMID 19553915.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - Raby, Wilfrid Noel; Carpenter, Kenneth M.; Rothenberg, Jami; Brooks, Adam C.; Jiang, Huiping; Sullivan, Maria; Bisaga, Adam; Comer, Sandra; Nunes, Edward V. (2009). "Intermittent Marijuana Use Is Associated with Improved Retention in Naltrexone Treatment for Opiate-Dependence". The American Journal on Addictions. 18 (4): 301–8. doi:10.1080/10550490902927785. PMC 2753886. PMID 19444734.
- Mikuriya TH (1969). "Marijuana in medicine: past, present and future". California Medicine. 110 (1): 34–40. PMC 1503422. PMID 4883504.
- TruthOnPot.com (20 May 2013). "Study: Cannabis Helps Manage Symptoms of Crohn's Disease". TruthOnPot.com. TruthOnPot.com. Retrieved 11 June 2013.
- Naftali, Timna (6). "Cannabis Induces a Clinical Response in Patients with Crohn's Disease: a Prospective Placebo-Controlled Study". Clinical Gastroenterology and Hepatology. 11 (10). Elsevier Inc: 1276–1280.e1. doi:10.1016/j.cgh.2013.04.034. PMID 23648372.
{{cite journal}}:|first2=missing|last2=(help);|first3=missing|last3=(help);|first4=missing|last4=(help);|first5=missing|last5=(help);|first6=missing|last6=(help); Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|month=ignored (help) - Penner, Elizabeth A.; Buettner, Hannah; Mittleman, Murray A. (2013). "The Impact of Marijuana Use on Glucose, Insulin, and Insulin Resistance among US Adults". The American Journal of Medicine. 126 (7): 583–9. doi:10.1016/j.amjmed.2013.03.002. PMID 23684393.
- Downer EJ, Campbell VA (2010). "Phytocannabinoids, CNS cells and development: A dead issue?". Drug and Alcohol Review. 29 (1): 91–98. doi:10.1111/j.1465-3362.2009.00102.x. PMID 20078688.
- Burns TL, Ineck JR (2006). "Cannabinoid analgesia as a potential new therapeutic option in the treatment of chronic pain". The Annals of Pharmacotherapy. 40 (2): 251–260. doi:10.1345/aph.1G217. PMID 16449552.
- Kohn, David (5 November 2004). "Researchers buzzing about marijuana-derived medicines". San Francisco Chronicle. Retrieved 26 April 2009.
- Hampson AJ, Grimaldi M, Axelrod J, Wink D. (July 1998). "Cannabidiol and (−)Δ9-tetrahydrocannabinol are neuroprotective antioxidants". PNAS. 95 (14): 8268–73. Bibcode:1998PNAS...95.8268H. doi:10.1073/pnas.95.14.8268. PMC 20965. PMID 9653176. Retrieved 15 May 2011.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, Gibson D, Mandelbaum A, Etinger A, Mechoulam R (1992). "Isolation and structure of a brain constituent that binds to the cannabinoid receptor". Science. 258 (5090): 1946–1949. Bibcode:1992Sci...258.1946D. doi:10.1126/science.1470919. PMID 1470919.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Mechoulam R, Fride E (1995). "The unpaved road to the endogenous brain cannabinoid ligands, the anandamides". In Pertwee RG (ed.). Cannabinoid receptors. Boston: Academic Press. pp. 233–258. ISBN 0-12-551460-3.
- ^ Mechoulam, Raphael; Peters, Maximilian; Murillo-Rodriguez, Eric; Hanuš, Lumír O. (2007). "Cannabidiol – Recent Advances". Chemistry & Biodiversity. 4 (8): 1678. doi:10.1002/cbdv.200790147.
- Grlic, Ljubiša (1976). "A comparative study on some chemical and biological characteristics of various samples of cannabis resin". Bulletin on Narcotics. 14: 37–46.
- Zuardi, A.W.; Crippa, J.A.S.; Hallak, J.E.C.; Moreira, F.A.; Guimarães, F.S. (2006). "Cannabidiol, a Cannabis sativa constituent, as an antipsychotic drug". Brazilian Journal of Medical and Biological Research. 39 (4): 421–9. doi:10.1590/S0100-879X2006000400001. PMID 16612464.
- Campos, AC; Moreira, FA; Gomes, FV; Del Bel, EA; Guimaraes, FS (2012). "Multiple mechanisms involved in the large-spectrum therapeutic potential of cannabidiol in psychiatric disorders". Philosophical transactions of the Royal Society of London. Series B, Biological sciences. 367 (1607): 3364–78. doi:10.1098/rstb.2011.0389. PMC 3481531. PMID 23108553.
- Sandyk, R; Awerbuch, G (1988). "Marijuana and Tourette's syndrome". Journal of clinical psychopharmacology. 8 (6): 444–5. doi:10.1097/00004714-198812000-00021. PMID 3235704.
- Karniol IG, Shirakawa I, Takahashi RN, Knobel E, Musty RE (1975). "Effects of delta-9-tetrahydrocannabinol and cannabinol in man". Pharmacology. 13 (6): 502–12. doi:10.1159/000136944. PMID 1221432.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - McCallum ND, Yagen B, Levy S, Mechoulam R (1975). "Cannabinol: a rapidly formed metabolite of delta-1- and delta-6-tetrahydrocannabinol". Experientia. 31 (5): 520–1. doi:10.1007/BF01932433. PMID 1140243.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Mahadevan A, Siegel C, Martin BR, Abood ME, Beletskaya I, Razdan RK (2000). "Novel cannabinol probes for CB1 and CB2 cannabinoid receptors". Journal of Medicinal Chemistry. 43 (20): 3778–85. doi:10.1021/jm0001572. PMID 11020293.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Petitet F, Jeantaud B, Reibaud M, Imperato A, Dubroeucq MC (1998). "Complex pharmacology of natural cannabinoids: evidence for partial agonist activity of delta-9-tetrahydrocannabinol and antagonist activity of cannabidiol on rat brain cannabinoid receptors". Life Sciences. 63 (1): PL1–6. doi:10.1016/S0024-3205(98)00238-0. PMID 9667767.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gertsch J; Leonti M; Raduner S; Racz, I.; Chen, J.-Z.; Xie, X.-Q.; Altmann, K.-H.; Karsak, M.; Zimmer, A. (2008). "Beta-caryophyllene is a dietary cannabinoid". Proceedings of the National Academy of Sciences of the United States of America. 105 (26): 9099–104. Bibcode:2008PNAS..105.9099G. doi:10.1073/pnas.0803601105. PMC 2449371. PMID 18574142.
- Colasanti, BK (1990). "A comparison of the ocular and central effects of delta 9-tetrahydrocannabinol and cannabigerol". Journal of ocular pharmacology. 6 (4): 259–69. doi:10.1089/jop.1990.6.259. PMID 1965836.
- Colasanti, BK; Craig, CR; Allara, RD (1984). "Intraocular pressure, ocular toxicity and neurotoxicity after administration of cannabinol or cannabigerol". Experimental eye research. 39 (3): 251–9. doi:10.1016/0014-4835(84)90013-7. PMID 6499952.
- "Marijuana vs. Marinol – A side by side comparison". ProCon.org. Retrieved 7 January 2013Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - Marinol. fda.gov (September 2004).
- "Deaths from Marijuana v. 17 FDA-Approved Drugs". ProCon.org. Retrieved 7 January 2013.
- Stepper, H. P., Department of Health and Human Services (24 August 2005) Letter to Mr. Yablan. medicalmarijuana.procon.org
- West, M. E.; Homi, J. (1996). "Cannabis as a medicine". Br. J. Anaesth. 76 (1): 167. doi:10.1093/bja/76.1.167-a.
- ^ Dr Farid F. Youssef. "Cannibis Unmasked: What it is and why it does what it does". UWIToday: June 2010. http://sta.uwi.edu/uwitoday/archive/june_2010/article9.asp
- Evans, T. "Ganja-based eyedrops a hot sell." The Gleaner (Jamaica). 24 August 2003.
- Eulalee Thompson. "Seeing through ganja". The Gleaner (Jamaica). 29 January 2001
- Koch, Wendy (23 June 2005). "Spray alternative to pot on the market in Canada". USA Today. Retrieved 16 August 2009.
- "Sativex – Investigational Cannabis-Based Treatment for Pain and Multiple Sclerosis Drug Development Technology". SPG Media. Retrieved 8 August 2008.
- Cooper, Rachel."GW Pharmaceuticals launches world's first prescription cannabis drug in Britain" The Telegraph. 21 June 2010. Retrieved 15 May 2011.
- "Sativex Approved in New Zealand" GW Pharmaceuticals. 3 Nov.2010. Retrieved 15 May 2011.
- "Sativex Approved in the Czech Republic" GW Pharmaceuticals. 15 April 2011. Retrieved 15 May 2011.
- Greenberg, Gary (2005). "Respectable Reefer". Mother Jones. Retrieved 15 August 2009.
- Skrabek RQ, Galimova L, Ethans K, Perry D (2008). "Nabilone for the treatment of pain in fibromyalgia". The Journal of Pain. 9 (2): 164–73. doi:10.1016/j.jpain.2007.09.002. PMID 17974490.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - "ALL PRICES FOR: Marinol – Brand Version: 10 mg". PharmacyChecker.com. Retrieved 15 August 2009.
- "FDA approves new indication for Dronabinol" (Press release). Food and Drug Administration. 23 December 1992. Archived from the original on 6 May 1997. Retrieved 15 August 2009.
- "Sativex: CEDAC Final Recommendation on Reconsideration and Reasons for Recommendation" (PDF). Canadian Agency for Drugs and Technologies in Health. 27 September 2007. Retrieved 16 August 2009.
- Baltazar, Amanda. "What is Medical Marijuana". About.com. Retrieved 09/30/01.
{{cite web}}: Check date values in:|accessdate=(help) - Group, United Patients. "Ways to Consume Medical Marijuana". Retrieved 10/01/2013.
{{cite web}}:|last=has generic name (help); Check date values in:|accessdate=(help) - "Inter-agency advisory regarding claims that smoked marijuana is a medicine". fda.gov. 2006. Retrieved 24 December 2012Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - "Nida: Marijuana, An update from the National Institute on Drug Abuse". Nida.nih.gov. 2011. Retrieved 23 August 2011.
{{cite web}}: Unknown parameter|month=ignored (help) - "Medical Marijuana Passes House Civil Justice Committee Without Dissent" (Press release). Minnesotans for Compassionate Care. 11 March 2009. Retrieved 10 August 2009.
- Joy, Janet E.; Watson, Stanley J.; Benson, John A., eds. (1999). Marijuana and Medicine: Assessing the Science Base. Washington, D.C.: National Academies Press. ISBN 978-0-309-07155-0. OCLC 246585475.
- "Marinol" (PDF). FDA. Retrieved 10/1/13.
{{cite web}}: Check date values in:|accessdate=(help) - Jatoi A; Windschitl HE; Loprinzi CL; Sloan, JA; Dakhil, SR; Mailliard, JA; Pundaleeka, S; Kardinal, CG; Fitch, TR; Christensen, B (2002). "Dronabinol versus megestrol acetate versus combination therapy for cancer-associated anorexia: a North Central Cancer Treatment Group study". Journal of Clinical Oncology. 20 (2). Alexandria, VA: American Society of Clinical Oncology: 567–73. doi:10.1200/JCO.20.2.567. PMID 11786587.
{{cite journal}}:|first10=missing|last10=(help);|first11=missing|last11=(help);|format=requires|url=(help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - Strasser, F.; Strasser, F; Luftner, D; Possinger, K; Ernst, G; Ruhstaller, T; Meissner, W; Ko, YD; Schnelle, M; Reif, M; Cerny, T (2006). "Comparison of orally administered cannabis extract and delta-9-tetrahydrocannabinol in treating patients with cancer-related anorexia-cachexia syndrome: A multicenter, phase III, randomized, double-blind, placebo-controlled clinical trial from the Cannabis-In-Cachexia-Study-Group". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 24 (21): 3394–400. doi:10.1200/JCO.2005.05.1847. PMID 16849753.
- ^ "American Society of Addiction Medicine Rejects Use of 'Medical Marijuana,' Citing Dangers and Failure To Meet Standards of Patient Care, March 23, 2011". Maryland. PR Newswire. Retrieved 20 April 2011.
- ^ "Medical Marijuana, American Society of Addiction Medicine, 2010". Asam.org. 1 April 2010. Retrieved 20 April 2011.
- "Medical marijuana and the mind. More is known about the psychiatric risks than the benefits". The Harvard mental health letter / from Harvard Medical School. 26 (10): 1–3. 2010. PMID 20499454.
- Frisher, Martin; Crome, Ilana; Martino, Orsolina; Croft, Peter (2009). "Assessing the impact of cannabis use on trends in diagnosed schizophrenia in the United Kingdom from 1996 to 2005". Schizophrenia Research. 113 (2–3): 123–8. doi:10.1016/j.schres.2009.05.031. PMID 19560900.
- Kuepper, R.; Van Os, J.; Lieb, R.; Wittchen, H.-U.; Hofler, M.; Henquet, C. (2011). "Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10 year follow-up cohort study". BMJ. 342: d738. doi:10.1136/bmj.d738. PMC 3047001. PMID 21363868.
- Stokes, PR; Mehta, MA; Curran, HV; Breen, G; Grasby, PM (2009). "Can recreational doses of THC produce significant dopamine release in the human striatum?". NeuroImage. 48 (1): 186–90. doi:10.1016/j.neuroimage.2009.06.029. PMID 19539765.
-
Hashibe M; Morgenstern H; Cui Y; Tashkin D; Zhang, Z.-F.; Cozen, W.; Mack, T. M.; Greenland, S. (2006). "Marijuana use and the risk of lung and upper aerodigestive tract cancers: results of a population-based case-control study". Cancer Epidemiol. Biomarkers Prev. 15 (10): 1829–34. doi:10.1158/1055-9965.EPI-06-0330. PMID 17035389.
{{cite journal}}: Unknown parameter|laysummary=ignored (help) - Osterweil, Neil (24 May 2006). "ATS: Marijuana Smoking Found Non-Carcinogenic". MedPage Today. Retrieved 12 August 2009.
- Kaufman, Marc (26 May 2006). "Study Finds No Cancer-Marijuana Connection". The Washington Post. Retrieved 12 August 2009.
- Aldington S; Harwood M; Cox B; Weatherall, M.; Beckert, L.; Hansell, A.; Pritchard, A.; Robinson, G.; Beasley, R. (2008). "Cannabis use and risk of lung cancer: a case-control study". European Respiratory Journal. 31 (1): 280–6. doi:10.1183/09031936.00065707. PMC 2516340. PMID 18238947.
-
Hii SW, Tam JD, Thompson BR, Naughton MT (2008). "Bullous lung disease due to marijuana". Respirology. 13 (1): 122–7. doi:10.1111/j.1440-1843.2007.01186.x. PMID 18197922.
{{cite journal}}: Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - Tan, Carol; Hatam, N; Treasure, Tom (2006). "Bullous disease of the lung and cannabis smoking: Insufficient evidence for a causative link". Journal of the Royal Society of Medicine. 99 (2): 77–80. doi:10.1258/jrsm.99.2.77. PMC 1360494. PMID 16449781.
- "http://www-archive.thoracic.org/sections/publications/press-releases/conference/articles/2007/press-releases/marijuana-worsens-copd-symptoms-in-current-cigarette-smokers.html" (Press release). American Thoracic Society. 21 May 2007. Retrieved 11 August 2009.
{{cite press release}}: External link in|title= - Tan, W. C.; Lo, C.; Jong, A.; Xing, L.; Fitzgerald, M. J.; Vollmer, W. M.; Buist, S. A.; Sin, D. D.; Vancouver Burden of Obstructive Lung Disease (BOLD) Research Group (2009). "Marijuana and chronic obstructive lung disease: A population-based study". Canadian Medical Association Journal. 180 (8): 814–20. doi:10.1503/cmaj.081040. PMC 2665947. PMID 19364790.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help) - Tashkin, D. P. (2009). "Does smoking marijuana increase the risk of chronic obstructive pulmonary disease?". Canadian Medical Association Journal. 180 (8): 797–8. doi:10.1503/cmaj.090142. PMC 2665954. PMID 19364782.
- "MAPS/CaNORML vaporizer and waterpipe studies". Maps.org. Retrieved 14 November 2009.
- Jeff Winkler (13 September 2013). "Stealth stoner". Aeon Magazine. Aeon Magazine Ltd. Retrieved 14 September 2013.
- Abrams, D I; Vizoso, H P; Shade, S B; Jay, C; Kelly, M E; Benowitz, N L (2007). "Vaporization as a Smokeless Cannabis Delivery System: A Pilot Study". Clinical Pharmacology & Therapeutics. 82 (5): 572. doi:10.1038/sj.clpt.6100200.
- Levitz, SM; Diamond, RD (1991). "Aspergillosis and marijuana". Annals of internal medicine. 115 (7): 578–9. doi:10.7326/0003-4819-115-7-578_2. PMID 1652910.
- Laskow, Sarah (10 June 2013). "Marijuana vending machines are the future of recreational drug use". Grist. Retrieved 19 October 2013.
- "Marijuana vending machines". News.msn.com. Retrieved 19 October 2013.
- ^ "The pot vending machine's first foreign market? Canada, of course, 'a seed for the rest of the world' | National Post". News.nationalpost.com. Retrieved 19 October 2013.
- "Marijuana Vending Machines Popping Up At California Pot Clubs " CBS San Francisco". Sanfrancisco.cbslocal.com. 20 March 2013. Retrieved 19 October 2013.
- Vrankulj, Adam (13 November 2012). "Medbox partners with Canadian medical marijuana R&D lab". BiometricUpdate.com. Retrieved 19 October 2013.
- "Marijuana vending machines coming to a store near you? | Mail Online". Dailymail.co.uk. 10 June 2013. Retrieved 19 October 2013.
- Epstein, Mike (16 November 2012). "Marijuana Vending Machine Maker's Stock Skyrockets and Everybody Freaks Out". Geekosystem. Retrieved 19 October 2013.
- ^ "Marijuana Vending Machines, Stoner Fantasy, May Become Industry Norm". Huffingtonpost.com. Retrieved 19 October 2013.
- "Marijuana vending machines: helfpul or just hype? | Marijuana and Cannabis News". Toke of the Town. 29 March 2013. Retrieved 19 October 2013.
- "Marijuana Vending Machine Investing". Wealthdaily.com. 13 May 2013. Retrieved 19 October 2013.
- "Endexx Acquires Cann-Can LLC". PR Newswire (US).
- "MB Media Brokers To License Vending Messaging System". Vending Market Watch.
- "Endexx closes Acquisition of Dispense Labs LLC". PR Newswire (US).
- "www.Autospense.com".
- "Endexx Secures Exclusive World Wide Rights for Medical Marijuana Dispensing Technology". PR Newswire (US).
- "www.m3hub.com".
- "www.thcfinder.com/".
- "Endexx's M3Hub(TM) Platform Supports State Legalized Marijuana Laws". PR Newswire (US).
- "Endexx's M3Hub Platform Is the Robust "Seed to Sale" Tracking Solution". PR Newswire (US).
- "THCFinder.com Joins the M3Hub(TM)". PR Newswire (US).
- United States Adopted Names Coincil: Statement on a nonproprietary name
- "AMA Urges Reclassifying Marijuana". Americans for Safe Access. Retrieved 10 January 2010.
- "Use of Cannabis for Medicinal Purposes" (PDF). Report 3 of the Council on Science and Public Health (I-09). American Medical Assn. Retrieved 10 January 2010.
- "Supporting Research into the Therapeutic Role of Marijuana" (PDF). The American College of Physicians. 2008. Retrieved 15 August 2009.
- "Medical Marijuana Endorsements and Statements of Support". Marijuana Policy Project. 2007. Archived from the original on 14 March 2008. Retrieved 29 January 2008.
- "Marijuana: Policy & Advocacy". American Academy of Family Physicians. 2009. Retrieved 6 October 2009.
- Abel, Ernest L. (1980). "Cannabis in the Ancient World". Marihuana: the first twelve thousand years. New York City: Plenum Publishers. ISBN 978-0-306-40496-2.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - Li, Hui-Lin (1974). "An Archaeological and Historical Account of Cannabis in China", Economic Botany 28.4:437–448, p. 444.
- Bretschneider, Emil (1895). Botanicon Sinicum: Notes on Chinese Botany from Native and Western Sources. Part III, Botanical Investigations in the Materia Medica of the Ancient Chinese. Kelly & Walsh. p. 378.
- ^ Bloomquist, Edward (1971). Marijuana: The Second Trip. California: Glencoe Press.
- de Crespigny, Rafe (2007). A Biographical Dictionary of Later Han to the Three Kingdoms (23–220 CE). Leiden: Brill Publishers. p. 332. ISBN 978-90-04-15605-0. OCLC 71779118.
- Barber, Elizabeth Wayland. (1992). Prehistoric Textiles: The Development of Cloth in the Neolithic and Bronze Ages with Special Reference to the Aegean. Princeton University Press. p. 38.
- Smith, Frederick Porter (1911). Chinese Materia Medica: Vegetable Kingdom. Shanghai: American Presbyterian Mission Press. pp. 90–91.
- "The Ebers Papyrus The Oldest (confirmed) Written Prescriptions For Medical Marihuana era 1,550 BC". onlinepot.org. Retrieved 10 June 2008.
- "History of Cannabis". reefermadnessmuseum.org. Archived from the original on 25 May 2008. Retrieved 9 July 2008.
- Pain, Stephanie (15 December 2007). "The Pharaoh's pharmacists". New Scientist. Reed Business Information Ltd.
- (Webley, Kayla. "Brief History: Medical Marijuana." Time 21 June 2010.)
- Lise Manniche, An Ancient Egyptian Herbal, University of Texas Press, 1989, ISBN 978-0-292-70415-2
- Touw, Mia (1981). "The Religious and Medicinal Uses ofCannabisin China, India and Tibet". Journal of Psychoactive Drugs. 13 (1): 23–34. doi:10.1080/02791072.1981.10471447. PMID 7024492.
- ^ Butrica, James L. (2002). "The Medical Use of Cannabis Among the Greeks and Romans". Journal of Cannabis Therapeutics. 2 (2): 51. doi:10.1300/J175v02n02_04.
- Lozano, Indalecio (2001). "The Therapeutic Use of Cannabis sativa (L.) in Arabic Medicine". Journal of Cannabis Therapeutics. 1: 63. doi:10.1300/J175v01n01_05.
- The Antique Cannabis Book. antiquecannabisbook.com (16 March 2012). Retrieved 2012-05-19.
- "History of Cannabis". BBC News. 2 November 2001. Retrieved 17 August 2011.
- "Hasjisj in Nordisk Famijebok 1912" (in Swedish). Runeberg.org. Retrieved 15 January 2012.
- "The Newsweekly for Pharmacy". Chemist + Druggist. 28. London, New York City, Melbourne: Benn Brothers: 68, 330. 1886.
- Adams, Samuel Hopkins (1905). The Great American Fraud (4th ed., 1907). Chicago: American Medical Association. Retrieved 30 July 2009.
{{cite book}}: Cite has empty unknown parameter:|coauthors=(help) - Kalmar(Swedish newspaper), 1894-07-07
- "Golden Guide". zauberpilz.com.
- Template:Cz icon "Nad léčivými jointy s Lumírem Hanušem". blisty.cz. Retrieved 3 May 2011.
- Zimmerman, Bill (1998). Is Marijuana the Right Medicine for You?: A Factual Guide to Medical Uses of Marijuana. Keats Publishing. ISBN 0-87983-906-6.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Baker, David; Pryce, Gareth; Giovannoni, Gavin; Thompson, Alan J (2003). "The therapeutic potential of cannabis". The Lancet Neurology. 2 (5): 291. doi:10.1016/S1474-4422(03)00381-8.
- McPartland, John M.; Russo, Ethan B. (2001). "Cannabis and Cannabis Extracts". Journal of Cannabis Therapeutics. 1 (3–4): 103. doi:10.1300/J175v01n03_08.
- Mack,Alison ; Joy, Janet (2001). Marijuana As Medicine. National Academy Press. ISBN 0-309-06531-3.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Russo, Ethan; Mathre, Mary Lynn; Byrne, Al; Velin, Robert; Bach, Paul J.; Sanchez-Ramos, Juan; Kirlin, Kristin A. (2002). "Chronic Cannabis Use in the Compassionate Investigational New Drug Program". Journal of Cannabis Therapeutics. 2: 3. doi:10.1300/J175v02n01_02.
- Medical Marijuana Regulatory System, Part II. Department of Public Health and Environment, Department of Revenue Performance Audit, June 2013
- ^ "Single Convention on Narcotic Drugs, 1961 As amended by the 1972 Protocol" (PDF). International Narcotics Control Board. United Nations. 13 March 1961. pp. 2–3. Retrieved 17 August 2009.
- Template:De icon "Verordnung der Bundesministerin für Arbeit, Gesundheit und Soziales über den Verkehr und die Gebarung mit Suchtgiften – SV". Bundesministerium für Arbeit, Gesundheit und Soziales. 2011. Retrieved 25 March 2011.
- Template:De-icon Valenta, Claudia (2005). "Magistrale Problem-Rezepturen". Österreichische Apothekerzeitung (5). Vienna: Österreichische Apotheker-Verlagsges.m.b.H. Retrieved 30 July 2009.
- ^ Template:De icon ABDA – Bundesvereinigung Deutscher Apothekerverbände (21 April 2008). "Rezepturhinweise: Dronabinol- und Cannabis-Zubereitungen" (PDF). Pharmazeutische Zeitung. Eschborn: Govi-Verlag Pharmazeutischer Verlag GmbH. Retrieved 30 July 2009.
- "AFP: Austria allows cannabis for medical purposes". Google News. Agence France-Presse. Retrieved 21 July 2008.
- Template:De icon Anon (19 December 2008). "Änderung des Suchtmittelgesetzes – SMG" (PDF). Bundesgesetzblatt für die Republik Österreich. Vienna: Österreichischer Bundesverlag. Retrieved 30 July 2009.
- "MMAR FAQ". MMAR FAQ.
- "Frequently Asked Questions – Medical Use of Marihuana". Health Canada. 13 June 2005. Retrieved 23 September 2009.
- "More pot, please: Demand booming for Prairie Plant's marijuana". CBC News. 23 October 2006. Retrieved 23 September 2009.
- Capler, Rielle (2007). "A Review of the Cannabis Cultivation Contract between Health Canada and Prairie Plant Systems" (PDF). British Columbia Compassion Club Society. Retrieved 23 September 2009.
- Kari, Shannon (1 June 2009). "Court challenge aims to legalize all cannabis use; Advocates say previous rule a 'mockery'". National Post. Toronto. p. A.6. ProQuest Newsstand, Document ID: 1739130721.
- http://www.ipolitics.ca/2012/12/14/health-canada-getting-out-of-the-marijuana-trade/
- Zdravotnictví prochází změnou. Léčba konopím je nyní legální | Zprávy z domova. www.lidovky.cz. Retrieved on 2013-04-17.
- Radio Prague – News – 01-04-2013 21:30. Radio.cz. Retrieved on 2013-04-17.
- Ann Törnkvist (10 June 2013). "French law on pot-based medicine takes effect". The Local. Retrieved 12 June 2013.
- "Germany: First Patients to Receive cannabis from the pharmacy". IACM-Bulletin. 15 February 2009.
- Grotenhermen, F. (2002). "The Medical use of Cannabis in Germany". Journal of Drug Issues. 32 (2): 607. doi:10.1177/002204260203200218.
- Template:De icon "Gesetz über den Verkehr mit Betäubungsmitteln (Betäubungsmittelgesetz – BtMG)" (PDF). Bundesministerium der Justiz. 19 January 2009. Retrieved 30 July 2009.
- ^ Bohn, Lauren E. (2 November 2012). "Israel pushing ahead in medical marijuana industry". The Seattle Times.
- ^ Kloosterman, Karin (29 March 2012). "Israeli medicine goes to pot". Israel 21C. Retrieved 4 November 2012.
- News: ISRAELVALLEY SANTE – Les vertus du cannabis – En Israël, le « fournisseur médical » de marijuana du Ministère de la santé, Tikun Olam, prône les bienfaits de la plante controversée pour le traitement du cancer. Israelvalley.com – Site officiel de la Cambre de Commerce France-Israël, CCFI (22 November 2010). Retrieved 2012-05-19.
- Hidalgo, Susana (01-03-2009). "El debate sobre el cannabis no espabila." Público.es
- ^ Pérez-Lanzac C. (12 September 2008) El cannabis pelea por un espacio legal. El País.
- "Drug Offences Definitive Guideline" (PDF). Sentencing Council.
- ^ The Committee Office, House of Lords. "House of Lords – Science and Technology – Ninth Report". Parliament.the-stationery-office.co.uk. Retrieved 20 October 2010.
- ^ US patent 6630507, Aidan J. Hampson; Iulius Axelrod & Maurizio Grimaldi, "Cannabinoids as antioxidants and neuroprotectants", issued 2003-10-07, assigned to The United States of America as represented by the Department of Health and Human Services
- ^ "Inter-Agency Advisory Regarding Claims That Smoked Marijuana Is a Medicine" (Press release). Food and Drug Administration. 20 April 2006. Retrieved 9 August 2009.
- "The DEA Position on Marijuana". Drug Enforcement Administration. 2006. Archived from the original on 28 August 2010. Retrieved 11 August 2009.
- "Cannabis science continues forward with FDA IND process as patients report successful cancer treatments". Cannabis Science. 2 April 2012. Retrieved 24 December 2012.
- "Marijuana Registry". Alaska Health and Social Services. Retrieved 8 October 2009.
- "Arizona Becomes 15th State to Approve Medical Marijuana". The New York Times. Associated Press. 14 November 2010. Retrieved 15 November 2010.
- "Medical Marijuana Program". California Department of Public Health. Retrieved 8 October 2009.
- "Colorado Medical Marijuana Registry". Colorado Department of Public Health and Environment. Retrieved 8 October 2009.
- Zalaznick, Matt. "Connecticut Docs Can Prescribe Medical Marijuana". The Norwalk Daily Voice. Retrieved 26 July 2012.
- "Connecticut Senate Passes Medical Marijuana Bill". ABC News. Retrieved 5 May 2012.
- "Delaware Medical Marijuana Patient Laws". Chronic Resource for Delaware Marijuana. Retrieved 20 January 2012.
- "Delaware legalizes medical marijuana". Reuters. 13 May 2011. Retrieved 20 January 2012.
- "Narcotics Enforcement Division". Hawaii Department of Public Safety. Retrieved 8 October 2009.
- Nemitz, Bill (26 February 2009). "Maine's cannabis contradiction". Portland Press Herald. Archived from the original on 2 May 2009. Retrieved 8 October 2009.
- "Michigan Medical Marijuana Program". Michigan Department of Community Health. Retrieved 8 October 2009.
- "Montana Medical Marijuana Program". Montana Department of Public Health and Human Services. Retrieved 8 October 2009.
- "Medical Marijuana". Nevada Department of Health and Human Services. Retrieved 8 October 2009.
- Kocieniewski, David (11 January 2010). "New Jersey Lawmakers Pass Medical Marijuana Bill". The New York Times. Retrieved 15 May 2010.
- "Medical Cannabis Program". New Mexico Department of Health. Retrieved 8 October 2009.
- "Oregon Medical Marijuana Program (OMMP)". State of Oregon – Department of Human Services. Retrieved 7 October 2009.
- "Medical Marijuana Program (MMP)". Rhode Island Department of Health. Retrieved 8 October 2009.
- "Vermont Marijuana Registry: A Guide for Patients and Physicians". Vermont Criminal Information Center. Retrieved 8 October 2009.
- "Medical Marijuana Frequently Asked Questions". Washington State Department of Health. Retrieved 8 October 2009.
- Accessed: 8/13/2013
- "US medical cannabis policy eased". BBC News. 20 October 2009. Retrieved 30 October 2009.
- NORML – "Maryland Medical Marijuana".
- "BILL INFO-2011 Regular Session-SB 308". mlis.state.md.us.
- "Employers now able to fire medical marijuana users legally in Washington". MedicalMarijuanaBill.com. 13 June 2011. Retrieved 31 July 2011.
- Mitchell, Dan (31 May 2008). "Legitimizing Marijuana". The New York Times. Retrieved 11 August 2009.
- The Times – California dreaming of full marijuana legalisation, The Times, 28 September 2009
- "§ 18.2–251.1. Possession or distribution of marijuana for medical purposes permitted". Virginia Department of Health. Retrieved 30 August 2010.
- "Oregon Medical Marijuana Program". public.health.oregon.gov. 1 October 2011. Retrieved 24 December 2012Template:Inconsistent citations
{{cite web}}: CS1 maint: postscript (link) - "19 October 2009; Office of the Deputy Attorney General, US Dept. of Justice, Washington D.C. 20530. Memorandum for Selected United States Attorneys. Subject: Investigations and Prosecutions in States Authorizing the Medical Use of Marijuana" (PDF). Retrieved 20 October 2010.
- US patent 6630507, Hampson, Aidan J.; Axelrod, Julius; Grimaldi, Maurizio, "Cannabinoids as antioxidants and neuroprotectants", issued 2003-10-07
- Billy, Michael (7 July 2008). "Opinion: US Government Holds Patent For Medical Marijuana, Shows Hipocrisy". DigitalJournal.com. Retrieved 11 August 2009.
- "Federal Register | Prospective Grant of Exclusive License: Development of Cannabinoid(s) and Cannabidiol(s) Based Therapeutics To Treat Hepatic Encephalopathy in Humans". Federalregister.gov. 17 November 2011. Retrieved 13 August 2012.
Further reading
- Iversen, Leslie L. (2000). The Science of Marijuana. Oxford University Press. ISBN 0-19-513123-1.
- 2009 Conference on Cannabinoids in Medicine, International Association for Cannabis as Medicine
- Cabral, Guy A. (2001). "Marijuana and Cannabinoids: Effects on Infections, Immunity, and AIDS". Journal of Cannabis Therapeutics. 1 (3–4): 61–85. doi:10.1300/J175v01n03_06. See also its alternate publication: Cabral, Guy A. (2001). "Marijuana and cannabinoids: effects on infections, immunity, and AIDS". In Ethan Russo (ed.). Cannabis therapeutics in HIV/AIDS. Routledge. pp. 61–85. ISBN 978-0-7890-1699-7.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - Watson, S. J.; Benson Jr, JA; Joy, JE (2000). "Marijuana and Medicine: Assessing the Science Base: A Summary of the 1999 Institute of Medicine Report". Archives of General Psychiatry. 57 (6): 547–52. doi:10.1001/archpsyc.57.6.547. PMID 10839332.
- "References on Multiple Sclerosis and Marijuana". Schaffer Library of Drug Policy.
- Tashkin, Donald P. (2001). "Effects of Smoked Marijuana on the Lung and Its Immune Defenses: Implications for Medicinal Use in HIV-Infected Patients". In Ethan Russo (ed.). Cannabis therapeutics in HIV/AIDS. New York City: Haworth Press. pp. 87–102. ISBN 978-0-7890-1699-7.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - Wujastyk, Dominik (12 September 2001). "Cannabis in Traditional Indian Herbal Medicine" (PDF). Retrieved 23 September 2009.
- Joy, Janet E.; Watson, Stanley J.; Benson, John A., eds. (1999). Marijuana and Medicine: Assessing the Science Base. Washington, D.C.: National Academies Press. ISBN 978-0-309-07155-0. OCLC 246585475.
- Zuardi, Antonio Waldo (2006). "History of cannabis as a medicine: A review". Revista Brasileira de Psiquiatria. 28 (2): 153–7. doi:10.1590/S1516-44462006000200015. PMID 16810401.
- Martinez, Martin (4 August 2008). "History of Medical Cannabis". Retrieved 23 September 2009.
- Aggarwal, SK; Carter, GT; Sullivan, MD; Zumbrunnen, C; Morrill, R; Mayer, JD (2009). "Medicinal use of cannabis in the United States: Historical perspectives, current trends, and future directions". Journal of opioid management. 5 (3): 153–68. PMID 19662925.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help)
External links
- Marijuana: Gateway to Health Book discussion on C-SPAN by Clint Werner
- Template:Dmoz, links to websites about medical cannabis.
- Medical Marijuana: The Supremacy Clause, Federalism, and the Interplay Between State and Federal Laws Congressional Research Service.
- The Center for Medicinal Cannabis Research of the University of California.
- Bibliography on the use of medical cannabis in recent history Advances in the History of Psychology, York University.
- The Forbidden Medicine, an independent site operated by Harvard Medical School faculty members James Bakalar and Lester Grinspoon.
- Cannabis Health Journal Online Medicinal Marijuana magazine based in British Columbia.
- Medical Marijuana in the U.S.
| Cannabis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| General | |||||||||
| Usage |
| ||||||||
| Variants | |||||||||
| Effects |
| ||||||||
| Culture | |||||||||
| Organizations |
| ||||||||
| Demographics | |||||||||
| Politics |
| ||||||||
| Related | |||||||||
| Ancient anaesthesia | |
|---|---|
| Plants / animals |
|
| Preparations | |
| Compounds | |
| People | |
| Recreational drug use | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
| Medicinal herbs and fungi | |
|---|---|
| Herbs |
|
| Fungi | |
| Regional practices | |
| Related subjects | |
| List of plants used in herbalism | |
Categories:

