| Revision as of 20:52, 4 September 2021 editPrcc27 (talk | contribs)Extended confirmed users, Pending changes reviewers13,052 edits →Recommendations: Add info about VMMC being done in response to WHO 2007 recommendations.← Previous edit | Revision as of 03:04, 27 September 2021 edit undoMichael Glass (talk | contribs)Extended confirmed users11,667 edits →Efficacy: Regional differences (as per discussion)Next edit → | ||
| Line 17: | Line 17: | ||
| === Men who have sex with men === | === Men who have sex with men === | ||
| A 2008 meta-analysis of gay and bisexual men found that HIV infection was reduced by 23% in circumcised males.<ref name="Millett">{{cite journal | vauthors = Yuan T, Fitzpatrick T, Ko NY, Cai Y, Chen Y, Zhao J, Li L, Xu J, Gu J, Li J, Hao C, Yang Z, Cai W, Cheng CY, Luo Z, Zhang K, Wu G, Meng X, Grulich AE, Hao Y, Zou H | display-authors = 6 | title = Circumcision to prevent HIV and other sexually transmitted infections in men who have sex with men: a systematic review and meta-analysis of global data | journal = The Lancet. Global Health | volume = 7 | issue = 4 | pages = e436–e447 | date = April 2019 | pmid = 30879508 | doi = 10.1016/S2214-109X(18)30567-9 | pmc = 7779827 | doi-access = free }}</ref> The ] does not recommend circumcision as protection against male to male HIV transmission, as evidence is lacking in regards to receptive anal intercourse. The WHO also states that ] (MSM) should not be excluded from circumcision services in countries in eastern and southern Africa, and that circumcision may be effective at limiting the spread of HIV for MSM if they also engage in vaginal sex with women.<ref name="WHO-PrevHIV"/> | A 2008 meta-analysis of gay and bisexual men found that HIV infection was reduced by 23% in circumcised males.<ref name="Millett">{{cite journal | vauthors = Yuan T, Fitzpatrick T, Ko NY, Cai Y, Chen Y, Zhao J, Li L, Xu J, Gu J, Li J, Hao C, Yang Z, Cai W, Cheng CY, Luo Z, Zhang K, Wu G, Meng X, Grulich AE, Hao Y, Zou H | display-authors = 6 | title = Circumcision to prevent HIV and other sexually transmitted infections in men who have sex with men: a systematic review and meta-analysis of global data | journal = The Lancet. Global Health | volume = 7 | issue = 4 | pages = e436–e447 | date = April 2019 | pmid = 30879508 | doi = 10.1016/S2214-109X(18)30567-9 | pmc = 7779827 | doi-access = free }}</ref> The ] does not recommend circumcision as protection against male to male HIV transmission, as evidence is lacking in regards to receptive anal intercourse. The WHO also states that ] (MSM) should not be excluded from circumcision services in countries in eastern and southern Africa, and that circumcision may be effective at limiting the spread of HIV for MSM if they also engage in vaginal sex with women.<ref name="WHO-PrevHIV"/> | ||
| ===Regional differences=== | |||
| It is not known whether the effect of male circumcision differs by HIV-1 variant. The predominant subtype of HIV-1 in the ] is subtype B, and in Africa, the predominant subtypes are A, C, and D.<ref>https://afju.springeropen.com/articles/10.1186/s12301-019-0005-2</ref> | |||
| A September 2021 study, with 569,950 males from Ontario, Canada, found that there was no independent link between circumcision status and HIV risk among males in Ontario.<ref> https://pubmed.ncbi.nlm.nih.gov/34551593/ </ref> | |||
| ==Recommendations== | ==Recommendations== | ||
Revision as of 03:04, 27 September 2021
This article is about male circumcision and HIV. For female circumcision and HIV, see Female genital mutilation § HIV.
In the context of high risk populations, male circumcision has been shown to reduce the risk of human immunodeficiency virus (HIV) transmission from HIV+ women to men. In 2020, the World Health Organization (WHO) reiterated that male circumcision is an efficacious intervention for HIV prevention if carried out by medical professionals under safe conditions. Circumcision reduces the risk that a man will acquire HIV and other sexually transmitted infections (STIs) from an infected female partner through vaginal sex.
Efficacy
Heterosexual men
As of 2020, past research has found strong evidence that circumcision reduces the risk of HIV infection in heterosexual men, although these studies have had limitations.
The WHO Expert Group on Models To Inform Fast Tracking Voluntary Medical Male Circumcision In HIV Combination Prevention in 2016 found "large benefits" of circumcision in settings with high HIV prevalence and low circumcision prevalence. The Group estimated male circumcision is cost-saving in almost all high priority countries. Furthermore, WHO stated that: "While circumcision reduces a man’s individual lifetime HIV risk, the indirect effect of preventing further HIV transmissions to women, their babies (vertical transmission) and from women to other men has an even greater impact on the population incidence, particularly for circumcisions performed at younger ages (under age 25 years)."
Newly-circumcised HIV infected men who have not had antiretroviral therapy can shed the HIV virus from the circumcision wound, thus increasing the immediate risk of HIV transmission to female partners. This risk of post-operative transmission presents a challenge, although in the long-term it is likely the circumcision of HIV-infected men helps lessen heterosexual HIV transmission overall. Such viral shedding can be mitigated by the use of antiretroviral drugs.
Men who have sex with men
A 2008 meta-analysis of gay and bisexual men found that HIV infection was reduced by 23% in circumcised males. The WHO does not recommend circumcision as protection against male to male HIV transmission, as evidence is lacking in regards to receptive anal intercourse. The WHO also states that men who have sex with men (MSM) should not be excluded from circumcision services in countries in eastern and southern Africa, and that circumcision may be effective at limiting the spread of HIV for MSM if they also engage in vaginal sex with women.
Regional differences
It is not known whether the effect of male circumcision differs by HIV-1 variant. The predominant subtype of HIV-1 in the United States is subtype B, and in Africa, the predominant subtypes are A, C, and D. A September 2021 study, with 569,950 males from Ontario, Canada, found that there was no independent link between circumcision status and HIV risk among males in Ontario.
Recommendations
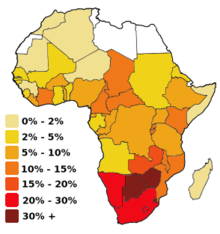
The most recent WHO review of the evidence confirmed prior estimates of the impact of male circumcision on HIV incidence rates. In 2020, they again concluded that male circumcision is an efficacious intervention for HIV prevention and that the promotion of male circumcision is an essential strategy, in addition to other preventive measures, for the prevention of heterosexually acquired HIV infection in men. Eastern and southern Africa had a particularly low prevalence of circumcised males. This region has a disproportionately high HIV infection rate, with a significant number of those infections stemming from heterosexual transmission. As a result, voluntary medical male circumcision (VMMC) has been a priority intervention in that region since the WHO's 2007 recommendations.
Although these results demonstrate that male circumcision reduces the risk of men becoming infected with HIV, the UN agencies emphasize that it does not provide complete protection against HIV infection. Circumcised men can still become infected with the virus and, if HIV-positive, can infect their sexual partners. Male circumcision should never replace other known effective prevention methods and should always be considered as part of a comprehensive prevention package, which includes correct and consistent use of male or female condoms, reduction in the number of sexual partners, delaying the onset of sexual relations, and HIV testing and counselling.
— World Health Organization, Joint WHO/UNAIDS Statement made in 2007.
Because the evidence that circumcision prevents HIV mainly comes from studies conducted in Africa, the Royal Dutch Medical Association (KNMG) in 2010 questioned the applicability of those studies to developed countries. Circumcision has not been included in their HIV prevention recommendations. The KNMG viewpoint document said that the relationship between HIV transmission and circumcision was unclear, and that behavioral factors seemed to have more of an effect on HIV prevention than circumcision. The KNMG also said that the choice of circumcision should be put off until an age when a possible HIV risk reduction would be relevant, so that boys could decide for themselves whether to undergo the procedure or choose other prevention alternatives. This KNMG circumcision policy statement was endorsed by several Dutch medical associations.
In the United States, the American Academy of Pediatrics (AAP) led a 2012 task force which included the American Academy of Family Physicians (AAFP), the American College of Obstetricians and Gynecologists (ACOG), and the Centers for Disease Control (CDC). The task force concluded that circumcision may be helpful for the prevention of HIV in the United States. In line with the AAP task force, the CDC 2018 position on circumcision and HIV recommended that circumcision should continue to be offered to parents who are informed of the benefits and risks, including a potential reduction in risk of HIV transmission. Circumcision conducted after sexual debut can result in missed opportunities for HIV prevention.
Mechanism of action
While the biological mechanism of action is not known, a 2020 meta-analysis stated "the consistent protective effect suggests that the reasons for the heterogeneity lie in concomitant individual social and medical factors, such as presence of STIs, rather than a different biological impact of circumcision." The inner foreskin harbours an increased density of CD4 T-cells and releases increased levels of pro-inflammatory cytokines. Hence the sub-preputial space displays a pro-inflammatory environment, conducive to HIV infection.
Experimental evidence supports the theory that Langerhans cells (part of the human immune system) in foreskin may be a source of entry for the HIV virus. Excising the foreskin removes what is thought to be a main entry point for the HIV virus.
History
Valiere Alcena, in a 1986 letter to the New York State Journal of Medicine, noted that low rates of circumcision in parts of Africa had been linked to the high rate of HIV infection. Aaron J. Fink several months later also proposed that circumcision could have a preventive role when the New England Journal of Medicine published his letter, "A possible explanation for heterosexual male infection with AIDS," in October, 1986. By 2000, over 40 epidemiological studies had been conducted to investigate the relationship between circumcision and HIV infection. A meta-analysis conducted by researchers at the London School of Hygiene & Tropical Medicine examined 27 studies of circumcision and HIV in sub-Saharan Africa and concluded that these showed circumcision to be "associated with a significantly reduced risk of HIV infection" that could form part of a useful public health strategy.
A 2005 review of 37 observational studies expressed reservations about the conclusion because of possible confounding factors, since all studies to date had been observational as opposed to randomized controlled trials. The authors stated that three randomized controlled trials then underway in Africa would provide "essential evidence" about the effects of circumcision on preventing HIV.
In 2009, a Cochrane review which included the results of the three 2000s trials found "strong" evidence that the acquisition of HIV by a man during sex with a woman was decreased by 38% and 66% over 24 months if the man was circumcised. The review also found a low incidence of adverse effects from circumcision in the trials reviewed. WHO assessed these as "gold standard" studies and found "strong and consistent" evidence from later studies that confirmed the results. In 2020, a review including post-study follow up from the three randomized controlled trials, as well as newer observational studies, found a 59% reduction in HIV incidence across the three randomized controlled trials, as well as continued protection for up to 6 years after the studies began.
Society and culture
The WHO recommends VMMC, as opposed to traditional circumcision. There is some evidence that traditionally circumcised men (i.e. who have been circumcised by a person who is not medically trained) use condoms less often and have higher numbers of sexual partners, increasing their risk of contracting HIV. Newly circumcised men must refrain from sexual activity until the wounds are fully healed.
The prevalence of circumcision varies across Africa. Studies were conducted to assess the acceptability of promoting circumcision; in 2007, country consultations and planning to scale up male circumcision programmes took place in Botswana, Eswatini, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Uganda, Tanzania, Zambia and Zimbabwe.
Programs
In 2011, UNAIDS prioritized 15 high HIV prevalence countries in eastern and southern Africa, with a goal of circumcising 80% of men (20.8 million) by the end of 2016. As of 2020, WHO estimated that 250,000 HIV infections have been averted by the 23 million circumcisions conducted in the 15 priority countries of eastern and southern Africa.
See also
References
- ^ "Preventing HIV Through Safe Voluntary Medical Male Circumcision For Adolescent Boys And Men In Generalized HIV Epidemics". World Health Organization. 2020. Retrieved 2021-05-24.
{{cite web}}: CS1 maint: url-status (link) - ^ Information for providers counseling male patients and parents regarding male circumcision and the prevention of HIV infection, STIs, and other health outcomes (Report). Centers for Disease Control and Prevention. August 22, 2018. Archived from the original on 2021-05-06. Retrieved 2021-05-26.
- ^ Farley TM, Samuelson J, Grabowski MK, Ameyan W, Gray RH, Baggaley R (June 2020). "Impact of male circumcision on risk of HIV infection in men in a changing epidemic context - systematic review and meta-analysis". J Int AIDS Soc (Review). 23 (6): e25490. doi:10.1002/jia2.25490. PMC 7303540. PMID 32558344.
- "Models To Inform Fast Tracking Voluntary Medical Male Circumcision In HIV Combination Prevention" (PDF). World Health Organization. March 2016. Archived (PDF) from the original on 2020-09-23. Retrieved 2021-05-26.
- Tobian AA, Adamu T, Reed JB, Kiggundu V, Yazdi Y, Njeuhmeli E (December 2015). "Voluntary medical male circumcision in resource-constrained settings". Nat Rev Urol (Review). 12 (12): 661–70. doi:10.1038/nrurol.2015.253. PMID 26526758. S2CID 10432723.
- Yuan T, Fitzpatrick T, Ko NY, Cai Y, Chen Y, Zhao J, et al. (April 2019). "Circumcision to prevent HIV and other sexually transmitted infections in men who have sex with men: a systematic review and meta-analysis of global data". The Lancet. Global Health. 7 (4): e436–e447. doi:10.1016/S2214-109X(18)30567-9. PMC 7779827. PMID 30879508.
- https://afju.springeropen.com/articles/10.1186/s12301-019-0005-2
- https://pubmed.ncbi.nlm.nih.gov/34551593/
- "WHO and UNAIDS Secretariat welcome corroborating findings of trials assessing impact of male circumcision on HIV risk" (Press release). World Health Organization. February 23, 2007. Archived from the original on 2007-02-26. Retrieved 2007-02-23.
- "Non-therapeutic circumcision of male minors KNMG viewpoint". www.knmg.nl. 27 May 2010.
{{cite web}}: CS1 maint: url-status (link) - American Academy of Pediatrics Task Force on Circumcision (2012). "Technical Report". Pediatrics. 130 (3): e756–e785. doi:10.1542/peds.2012-1990. ISSN 0031-4005. PMID 22926175. Archived from the original on 2012-09-20.
- Prodger, Jessica L. (September 2017). "The biology of how circumcision reduces HIV susceptibility: broader implications for the prevention field". AIDS Research and Therapy. 14 (1): 49. doi:10.1186/s12981-017-0167-6. PMC 5594533. PMID 28893286.
- Weiss HA, Dickson KE, Agot K, Hankins CA (October 2010). "Male circumcision for HIV prevention: current research and programmatic issues". AIDS (Randomized controlled trial). 24 Suppl 4 (Suppl 4): S61-9. doi:10.1097/01.aids.0000390708.66136.f4. PMC 4233247. PMID 21042054.
- Szabo R, Short RV (June 2000). "How does male circumcision protect against HIV infection?". BMJ (Review). 320 (7249): 1592–4. doi:10.1136/bmj.320.7249.1592. PMC 1127372. PMID 10845974.
- Alcena V (19 October 2006). "AIDS in Third World countries". PLOS Medicine (Comment). 86 (8): 446. PMID 3463895. Archived from the original on 10 January 2014. Retrieved 10 January 2014.
- Alcena V (August 1986). "AIDS in Third World countries". New York State Journal of Medicine (Letter). 86 (8): 446. PMID 3463895. Archived from the original on 2014-01-10. Retrieved 2014-01-10.
- Fink AJ (October 1986). "A possible explanation for heterosexual male infection with AIDS". The New England Journal of Medicine (Letter). 315 (18): 1167. doi:10.1056/nejm198610303151818. PMID 3762636.
- Szabo R, Short RV (June 2000). "How does male circumcision protect against HIV infection?". BMJ (Review). 320 (7249): 1592–4. doi:10.1136/bmj.320.7249.1592. PMC 1127372. PMID 10845974.
- Weiss HA, Quigley MA, Hayes RJ (October 2000). "Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis". AIDS (Meta-analysis). 14 (15): 2361–70. doi:10.1097/00002030-200010200-00018. PMID 11089625. S2CID 21857086. Archived from the original (PDF) on 2014-01-10.
- Siegfried N, Muller M, Deeks J, Volmink J, Egger M, Low N, et al. (March 2005). "HIV and male circumcision--a systematic review with assessment of the quality of studies". The Lancet. Infectious Diseases (Review). 5 (3): 165–73. doi:10.1016/S1473-3099(05)01309-5. PMID 15766651.
- Siegfried, Nandi; Muller, Martie; Deeks, Jonathan J; Volmink, Jimmy (15 April 2009). "Male circumcision for prevention of heterosexual acquisition of HIV in men". Cochrane Database of Systematic Reviews (2): CD003362. doi:10.1002/14651858.CD003362.pub2. PMID 19370585.
- Farley, Timothy MM; Samuelson, Julia; Grabowski, M Kate; Ameyan, Wole; Gray, Ronald H; Baggaley, Rachel (June 2020). "Impact of male circumcision on risk of HIV infection in men in a changing epidemic context – systematic review and meta‐analysis". Journal of the International AIDS Society. 23 (6): e25490. doi:10.1002/jia2.25490. PMC 7303540. PMID 32558344.
- Marck J (1997). "Aspects of male circumcision in sub-equatorial African culture history" (PDF). Health Transition Review (Review). 7 Suppl (Suppl): 337–60. PMID 10173099. Archived from the original (PDF) on 2008-09-06. Retrieved 2009-03-23.
- "Male circumcision: global trends and determinants of prevalence, safety and acceptability" (PDF). Who/Unaids. 2007. Archived (PDF) from the original on 2015-07-15. Retrieved 2008-10-16.
- "Towards Universal access: Scaling up priority HIV/AIDS interventions in the health sector" (PDF). Who/Unaids/Unicef: 75. 2008. Archived (PDF) from the original on 2008-10-18. Retrieved 2008-10-16.
- Joint strategic action framework to accelerate the scale-up of voluntary medical male circumcision for HIV prevention in Eastern and Southern Africa, 2012-2016. Archived 2017-07-29 at the Wayback Machine WHO. 2014.
| Circumcision | |
|---|---|
| Medical aspects | |
| History and prevalence | |
| Religious aspects | |
| Ethical and legal aspects | |
| Category | |
