This is an old revision of this page, as edited by Daveswenson (talk | contribs) at 01:33, 8 December 2007. The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 01:33, 8 December 2007 by Daveswenson (talk | contribs)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff) Pharmaceutical compound | |
 | |
| Clinical data | |
|---|---|
| Pregnancy category |
|
| Routes of administration | Usually oral; intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 25% (oral) |
| Metabolism | 95%, mainly Hepatic, also in blood and tissues |
| Elimination half-life | 30 - 60 minutes |
| Excretion | 5%, renal |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.218.519 |
| Chemical and physical data | |
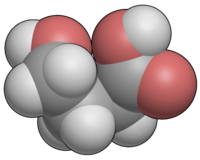
| Formula | C4H8O3 |
| Molar mass | 104.10 g/mol (GHB) 126.09 g/mol (sodium salt) 142.19 g/mol (potassium salt) g·mol |
| 3D model (JSmol) | |
SMILES
| |
Gamma-Hydroxybutyric acid (4-hydroxybutanoic acid, C4H8O3), commonly abbreviated GHB, is a neuroprotective therapeutic drug that is illegal in a number of countries, and is a naturally-occurring substance found in the central nervous system, wine, beef, small citrus fruits, and almost all living creatures in small amounts. It is currently regulated in the US and sold by Jazz Pharmaceuticals under the name Xyrem.
In a medical setting, GHB has been used historically as a general anesthetic, to treat conditions such as insomnia, clinical depression, narcolepsy, and alcoholism, and to improve athletic performance. It is also used illegally under the street names Juice, Liquid Ecstasy, Fantasy, "Georgia Homeboy", and simply G, either as an intoxicant or as a date rape drug. GHB is naturally produced in the human body's cells and is structurally related to the ketone body beta-hydroxybutyrate. As a drug, it is used most commonly in the form of a salt. GHB is also produced as a result of fermentation, and so is found in small quantities in some beers and wines.
History
Synthesis of the chemical GHB was first reported in 1874 by A. Saizew, but the first major research into its use in humans was conducted in the early 1960s by Dr. Henri Laborit to use in studying the neurotransmitter GABA. It quickly found a wide range of uses due to its minimal side-effects and short duration of action, the only difficulties being the narrow safe dosage range and the dangers presented by its combination with alcohol and other CNS depressants.
GHB was widely used in France, Italy, and other European countries for several decades as a sleeping agent and an anaesthetic in childbirth, but problems with its abuse potential and development of newer drugs have led to a decrease in legitimate medical use of GHB in recent times. The only common medical applications for GHB now days are in the treatment of narcolepsy and more rarely alcoholism. In the typical scenario, GHB has been synthesized from GBL (gamma-butyrolactone) by adding sodium hydroxide (lye) in ethanol or water. As of late, GBL has become controlled and more circuitous routes have to be taken, such as those starting with THF (tetrahydrofuran).
A popular children's toy, Bindeez (also known as Aqua Dots, in the United States), produced by Melbourne company Moose, was banned in Australia in early November 2007 when it was discovered that 1,4-butanediol, which is metabolised into GHB, had been substituted for the non-toxic plasticiser 1,5-pentanediol in the bead manufacturing process. Three young children were hospitalized as a result of ingesting a large number of the beads, and the toy was recalled.
Pharmacology
GHB has at least two distinct binding sites in the central nervous system, the newly-characterized GHB receptor, which is excitatory, and the GABAB receptor, which is inhibitory. GHB exists endogenously at concentrations high enough to activate the GHB receptor, but not at concentrations high enough to activate the GABAB receptor. This means that endogenous GHB has all the characteristics of an excitatory neurotransmitter.
When taken orally, GABA itself can not cross the Blood-Brain-Barrier nor does a high concentration actually reach the GABA receptors once in the brain. Since GABA is naturally systhesized in the brain, a higher than normal concentration will be quickly neutralized.
However, at pharmacological doses, GHB reaches much higher concentrations in the brain and activates GABAB receptors, which is responsible for its sedative effects. GHB's sedative effects are blocked by GABAB antagonists.
The role of the GHB receptor in the behavioural effects induced by GHB is more complex. GHB receptors are densely expressed in many areas of the brain, including the cortex and hippocampus, and these are the receptors that GHB displays the highest affinity for. There has been somewhat limited research into the GHB receptor - however, there is evidence that activation of the GHB receptor in some brain areas results in the release of glutamate - the principle excitatory neurotransmitter . Drugs which selectively activate the GHB receptor receptor cause absent seizures in high doses, as do GHB and GABA(B) agonists. .
Activation of both the GHB receptor and GABA(B) is responsible for the addictive profile of GHB. GHB's effect on dopamine release is biphasic , low concentrations stimulate dopamine release via the GHB receptor. Higher concentrations inhibit dopamine release - via GABA(B) receptors (as to other GABA(B) agonists - Baclofen, Phenibut) - after the initial phase of inhibition, dopamine release is then increased via the GHB receptor. Both the inhibition and increase of dopamine release by GHB are inhibited by opioid antagonists (Naloxone, Naltrexone). Dynorphin may play a role in the inhibition of dopamine release via Kappa opioid receptor.
This explains the paradoxical mix of sedative and stimulatory properties of GHB, as well as the so-called "rebound" effect, experienced by individuals using GHB as a sleeping agent, where they awake suddenly after several hours of GHB-induced deep sleep. That is to say, that over time, the concentration of GHB in the system decreases below the threshold for significant GABAB receptor activation and activates predominantly the GHB receptor, leading to wakefulness.
Recently, analogs of GHB, such as 4-hydroxy-4-methylpentanoic acid have been synthesised and tested on animals, in order to gain a better understanding of GHB's mode of action. Analogues of GHB such as 3-methyl-GHB, 4-methyl-GHB and 4-phenyl-GHB have been shown to produce similar effects to GHB in some animal studies, but these compounds are even less well researched than GHB itself. Of these analogues, only 4-methyl-GHB (gamma-hydroxyvaleric acid, GHV) and its prodrug form gamma-valerolactone (GVL) have been reported as drugs of abuse in humans, and on the available evidence seem to be less potent but more toxic than GHB, with a particular tendency to cause nausea and vomiting.
Other prodrug ester forms of GHB have also rarely been encountered by law enforcement, including 1,4-diacetoxybutane, methyl-4-acetoxybutanoate and ethyl-4-acetoxybutanoate, but these are generally covered by analogue laws in jurisdictions where GHB is illegal, and little is known about them beyond their presumably delayed onset and longer duration of action. The intermediate compound 4-hydroxybutaldehyde is also a prodrug for GHB, however as with all aldehydes this compound is caustic and is strong-smelling and foul-tasting; actual use of this compound as an intoxicant is likely to be unpleasant and result in severe nausea and vomiting.
Also note that both of the metabolic breakdown pathways shown for GHB can run in either direction, depending on the concentrations of the substances involved, so the body can make its own GHB either from GABA or from succinic semialdehyde. Under normal physiological conditions, the concentration of GHB in the body is rather low, and the pathways would run in the reverse direction to what is shown here to produce endogenous GHB. However, when GHB is consumed for medical or recreational purposes its concentration in the body is much higher than normal, which changes the enzyme kinetics so that these pathways operate to metabolise GHB rather than producing it.
Medical uses
GHB has been used historically as a general anesthetic in the 1960s, as a hypnotic in the treatment of insomnia, to treat depression, and to improve athletic performance. In Italy, under the trade name Alcover (ATC code N07BB), GHB is used in the treatment of alcoholism (50 to 100 milligrams per kilogram per day, in 3 or more divided doses), both for acute alcohol withdrawal and medium to long-term detoxification. In the United States, the Food and Drug Administration permits the use of GHB under the trade name Xyrem to reduce the number of cataplexy attacks in patients with narcolepsy.
When GHB is used in its sodium or potassium salt form, a significant quantity of excess sodium or potassium may be consumed, which should be taken into consideration by people with heart conditions, hypertension or compromised renal function. The bioavailability of sodium GHB is considerably reduced when it is consumed with food, and so it is advised to wait at least two hours after eating before consuming the dose. Because of its strong sedative effects, patients should not drive or operate heavy machinery for at least six hours after taking sodium GHB.
Adverse effects from Xyrem in clinical trials included: headache, nausea, dizziness, nasopharyngitis, somnolence, vomiting, urinary incontinence, confusion, dyspnea, hypoesthesia, paresthesia, tremor, vertigo, and blurred vision. Out of the 717 patients and 182 healthy volunteers who took part in the trials (899 total), two of them died from drug overdoses, although only one of these involved GHB.
Non-medical use
thumb|Dave Swenson: Common purchaser of GHB for underage females GHB is a CNS depressant used as an intoxicant. It has many street names, including Liquid Ecstasy and Liquid X. At recreational doses, GHB can cause a state of euphoria, increased enjoyment of movement and music, increased libido, increased sociability and intoxication. At higher doses, GHB may induce nausea, dizziness, drowsiness, agitation, visual disturbances, depressed breathing, amnesia, unconsciousness, and death. The effects of GHB can last from 1.5 to 3 hours, or even longer if large doses have been consumed or if it is mixed with alcohol.
In general, the doses used recreationally are between 500 mg and 3000 mg, corresponding to approximately 0.5–3 mL of liquid if the concentration is 1 gram / 1 mL (which is not always the case). When used as a recreational drug, GHB may be found as the sodium or potassium salt, which is a white crystalline powder, or as GHB salt dissolved in water to form a clear solution - generally at a concentration of 1 gram / 1 mL and so is twice the strength of the Xyrem solution sold legally for medical use. The sodium salt of GHB has a thin, very salty, chemical taste.
GHB salt dissolved in water is notoriously dangerous, as the concentration of GHB may not be known, and so the actual dose of GHB being consumed can be difficult to judge accurately. Since GHB sold for recreational use is subject to no standardisation it can be impossible to verify the actual concentration of GHB solution bought on the illicit market. Other salt forms such as calcium GHB and magnesium GHB have also been reported, but the sodium salt is by far the most common.
Some chemicals convert to GHB in the stomach and blood. GBL, or gamma-butyrolactone, is one such prodrug. Other prodrugs include 1,4-butanediol. There may be additional toxicity concerns with these precursors. 1,4-B and GBL are normally found as pure liquids, although they may be mixed with other more harmful solvents when intended for industrial use, e.g., as paint stripper or varnish thinner.
GHB can be produced in clandestine labs, and it is claimed that most of the GHB used in the US is illegally manufactured within its borders. While available as a prescription for sleep disorders in some other countries, GHB was banned (in the U.S.) by the FDA in 1990 because of the dangers associated with its use. However, on July 17, 2002 GHB was approved for treatment of cataplexy, often associated with narcolepsy. GHB is "colourless and odorless".
As a club scene or "rave" drug
| This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources in this section. Unsourced material may be challenged and removed. (July 2007) (Learn how and when to remove this message) |
Since the 1970s club scene, club-goers have used a range of drugs to enhance their experience on the dance floor such as amyl nitrite "poppers" and cocaine; in the 1990s, newer "club drugs" became popular, such as ketamine and Ecstasy (MDMA). Like these other "club drugs," GHB is taken because users feel that it enhances the experience of being in a club or at a party; GHB is sometimes referred to as liquid ecstasy due to its tendency to produce euphoria and sociability and its use in the dance party scene.
As a date rape drug
The drug has been referred to in the media as a date rape drug, in much the same way as alcohol and Rohypnol. As it is colourless and odorless, it has been described as "very easy to add to drinks". GHB has been used in many cases of drug-related sexual assault, usually when the victim is vulnerable due to intoxication with a sedative, generally alcohol or more rarely cannabis, and as such are less likely to notice a strange taste to his or her drink. However it is difficult to establish how often GHB is used to facilitate rape as it is difficult to detect in a urine sample after a day, and many victims may not recall the rape until some time after this. GHB produced as a sodium salt (sodium oxybate) may provide a noticeable salty character to the drink, although individual sensitivity to the taste of salt varies. GHB can also be produced as different salts, some of which may not have a taste as distinctive as the sodium salt (e.g., magnesium oxybate), or much less commonly in the unstable free-acid form.
Use by bodybuilders
Some athletes and bodybuilders also use GHB, as GHB has been shown to elevate human growth hormone in vivo. The growth hormone elevating effects of GHB are mediated through muscarinic acetylcholine receptors and can be prevented by prior administration of pirenzepine, a muscarinic acetylcholine receptor blocking agent.
As certain succinate salts have been shown to elevate growth hormone in vitro, being GHB is metabolized into succinate some people have suggested this may play a role in the growth hormone elevations from GHB. There is however currently no evidence to show that succinate plays any role in the growth hormone elevations from GHB.
Endogenous production by the body
Cells produce GHB by reduction of succinic semialdehyde. This enzyme appears to be induced by cAMP levels, meaning substances that elevate cAMP, such as forskolin and vinpocetine, may increase GHB synthesis and release. People with the disorder known as succinic semialdehyde dehydrogenase deficiency, also known as gamma-hydroxybutyric aciduria, have elevated levels of GHB in their urine, blood plasma and cerebrospinal fluid.
The precise function of GHB in the body is not clear. It is known however that the brain expresses a large amount of receptors that are activated by GHB. These receptors are excitatory and not responsible for the sedative effects of GHB - they have been shown to elevate the principle excitatory neurotransmitter - glutamate. The benzamide antipsychotics - amisulpride, sulpiride - have been shown to bind to this receptor in vivo. Other antipsychotics were tested and were not found to have an affinity for this receptor.
It is a precursor to GABA, glutamate and glycine in certain brain areas.
GHB has neuroprotective properties and has been found to protects cells from hypoxia.
As a natural fermentation by-product
GHB is also produced as a result of fermentation and so is found in small quantities in some beers and wines, particularly fruit wines. However, the amount of GHB found in wine is insignificant and not sufficient to produce any effects.
Dangers
As with pure alcohol, the dose-response curve of GHB is very steep, and "proper" dosing of illegal GHB can be difficult since it often comes as a salt dissolved in water, and the actual amount of GHB and/or other additives per "capful" can vary. Legal GHB comes in standardized doses and is free from contaminants, so it is much safer (cf. legal alcohol vs. bathtub gin). Also, like pure alcohol, small doses of GHB are considered safe, but high doses can cause unconsciousness, convulsions, vomiting, suppression of the gag reflex, and respiratory depression. These effects vary between persons and are dose-dependent. Synergy of its sedative effects are seen when combined with other CNS depressants such as alcohol, benzodiazepines (e.g., diazepam), barbiturates, and others.
Another complication is the difference in pharmacokinetics between GHB and its two prodrugs, 1,4-B and GBL. 1,4-butanediol is converted into GHB in the body by two enzymes alcohol dehydrogenase and aldehyde dehydrogenase, which gives it a delayed onset of effects and a longer duration of action. GHB is then further metabolised, again by alcohol dehydrogenase and aldehyde dehydrogenase, into the inactive succinate.
If alcohol has also been consumed this can saturate the dehydrogenase enzymes and so delays the conversion of 1,4-B into GHB, meaning that 1,4-B takes much longer to take effect and people may re-dose thinking it hasn't done anything, leading to an accidental overdose later on once it finally takes effect. 1,4-B itself can also contribute to the enzyme saturation, so, when alcohol and 1,4-B are consumed together, it produces a complex and somewhat unpredictable interaction between the varying levels of alcohol, 1,4-B and GHB present in the body. Alcohol also makes the GHB last longer in the body by competing for dehydrogenase enzymes, and hence delaying the conversion of GHB into succinate.
The other precursor gamma-butyrolactone (GBL) is rapidly converted into GHB by lactamase enzymes found in the blood. GBL is more lipophilic (fat soluble) than GHB, and so is absorbed faster and has higher bioavailability; the paradox is that this can mean that GBL has a faster onset of effects than GHB itself, even though it is a prodrug. The levels of lactamase enzyme can vary between individuals, and GBL is not active in its own right, so people who have never tried GBL before may have delayed or fewer effects than expected; however, once someone has taken GBL a few times, the production of lactamase enzymes is increased and he/she will feel the effects like normal.
Because of these pharmacokinetic differences, 1,4-B tends to be slightly less potent, slower to take effect but longer-acting than GHB, whereas GBL tends to be more potent and faster-acting than GHB, and has around the same duration.
Alcohol worsens both CNS depression and vomiting, so combining alcohol with GHB or its precursors can be particularly dangerous. Another factor to be considered is that people who drink alcohol regularly tend to induce expression of their dehydrogenase enzymes, and thus have higher levels of these enzymes than people that do not drink alcohol regularly; this means that regular alcohol drinkers will both convert 1,4-B into GHB more rapidly and also break down GHB into succinate faster than people that do not drink alcohol. This multitude of different factors can make the interactions between 1,4-B, GHB and alcohol very complicated and highly variable between different individuals.
Death while using GHB is most likely when it is combined with alcohol or other depressant drugs; however, as with all substances, an overdose of GHB alone may be lethal. A review of the details of 194 deaths attributed to or related to GHB over a ten-year period found that most were from respiratory depression caused by interaction with alcohol or other drugs; several were from choking on vomit and asphyxiating; remaining causes of death included motor vehicle and other accidents. The review included 70 cases where high levels of GHB were found post-mortem without concomitant ingestion of other drugs or alcohol.
Determining conclusively whether someone's death was caused by GHB is very difficult because a lab test will always detect the presence of some GHB in the human body, and levels of GHB can vary in the same individual depending on what part of the body is tested. GHB is a naturally-occurring substance that is always present in everyone, but little research has been done on what levels are normal in what parts of the body at what times.
There have been no systematic studies into the effects of GHB if taken chronically in humans, and hence whether prolonged use of GHB causes any bodily harm remains unknown. A UK parliamentary committee commissioned report found the use of GHB to be less dangerous than tobacco and alcohol in social harms, physical harm and addiction.
Treatment of overdose
Overdose of GHB can be difficult to treat because of its multiple effects on the body. GHB tends to cause rapid unconsciousness at doses above 3500 mg, with single doses over 7000 mg often causing life-threatening respiratory depression, and higher doses still can induce bradycardia and consequent heart failure. Because of the faster and more complete absorption of GBL relative to GHB, its dose-response curve is steeper, and overdoses of GBL tend to be more dangerous and problematic than overdoses involving only GHB or 1,4-B.
As well as causing these depressant effects, GHB overdose also often produces twitches or convulsions, especially when combined with stimulants such as amphetamines. Also GHB tends to cause nausea and vomiting, particularly when combined with alcohol; so a patient may be simultaneously unconscious, vomiting, and convulsing.
Overdoses wherein the patient has consumed GHB along with both alcohol and amphetamine-based stimulants are often particularly problematic; the stimulants may cause the patient to slip in and out of consciousness and he/she may be confused and combative, fighting off medical staff while half-awake before lapsing back into unconsciousness again. Care should be taken when attempting to sweep foreign bodies out of the mouth of a patient that presents with a suspected GHB overdose. The patient may bite very hard, and sometimes will not let go.
The most likely risk of death from GHB overdose is inhalation of vomit while unconscious. This risk can be partially prevented by laying the patient down in the recovery position. People are most likely to vomit as they become unconscious, and as they wake up. This is best managed in a hospital setting, but, if the patient is not in a hospital, it is very important that someone stays with the patient until he/she becomes fully unconscious, to keep the patient in the recovery position and to check how deeply unconscious the he/she becomes.
Then someone needs to stay with the patient in order to keep monitoring pulse and breathing rate. Finally, someone must stay with the patient until he fully wakes up. This is important, because people tend to become conscious enough to roll onto their backs just before they start to vomit again, but often while they are still too deeply unconscious to protect their own airway. This makes the period while people are waking up particularly dangerous.
Convulsions from GHB can be treated with diazepam or lorazepam, even though these are also CNS depressants they are GABAA agonists, whereas GHB is primarily a GABAB agonist, so the benzodiazepines do not worsen CNS depression as much as might be expected.
Most stimulants are not effective at counteracting the unconsciousness from GHB, but intravenous injection of cholinergic drugs such as arecoline, neostigmine, and physostigmine can quickly reverse the effects of the GHB and cause rapid awakening; this can be dangerous, however, as these drugs lower the convulsion threshold and so can make convulsions worse. For this reason, these drugs are seldom used in most countries, although, in France and Italy where there is a much longer history of medical use of GHB, physostigmine treatment for GHB overdose is more common.
The best treatment of a more serious GHB overdose is co-administration of lorazepam with physostigmine, and the dose of both drugs must be carefully titrated to avoid worsening either the CNS depression or the convulsions. Overdoses with larger quantities of GHB or more particularly GBL (generally 10,000mg or more) can stop both heart and breathing.
It can be very dangerous to look after someone who is unconscious as a result of drug overdose if the attending party does not have proper medical training. When an individual presents with a suspected GHB overdose and is unconscious, the first priority should be to check their pulse and breathing. If the patient is taking less than 8 breaths per minute, and if his/her pulse is less than 60 a minute (both numbers are for adults), then the appropriate course of action is to start CPR and call an ambulance.
A newer synthetic drug SCH-50911, which acts as a selective GABAB antagonist, quickly reverses GHB overdose in mice. However this treatment has yet to be tried in humans, and it is unlikely that it will be researched for this purpose in humans due to the illegal and unethical nature of clinical trials of GHB, and the lack of medical indemnity coverage inherent in using an untested treatment for a life-threatening overdose.
Addiction
GHB can be physically addictive and may result in psychological addiction. Physical dependence develops when GHB is taken on a regular basis (i.e., every 2-4 hours for multiple consecutive days or weeks). Withdrawal effects may include insomnia, restlessness, anxiety, tremors, sweating, loss of appetite, edginess, tachycardia, chest pain and tightness, muscle and bone aches, sensitivity to external stimuli (sound, light, touch), dysphoria, and mental dullness. These side-effects will subside after 2 - 21 days, depending on frequency of usage and the size of the doses used. In particularly severe cases, withdrawal from GHB may cause symptoms similar to acute withdrawal from alcohol or barbiturates (delirium tremens) and can cause convulsions and hallucinations.
Although there have been reported fatalities due to GHB withdrawal, reports are inconclusive and further research is needed. Unlike alcohol, there is no firm data that chronic use of GHB causes permanent damage to the body. In rats, no organ or brain damage was observed after chronic administration of GBL (a precursor to GHB).
Legal status
In Hong Kong, GHB is regulated under Schedule 1 of Hong Kong's Chapter 134 Dangerous Drugs Ordinance. It can only be used legally by health professionals and for university research purposes. The substance can be given by pharmacists under a prescription. Anyone who supplies the substance without prescription can be fined $10000 (HKD). The penalty for trafficking or manufacturing the substance is a $5,000,000 (HKD) fine and life imprisonment. Possession of the substance for consumption without license from the Department of Health is illegal with a $1,000,000 (HKD) fine and/or 7 years of jail time.
In the United States it was placed on Schedule I of the Controlled Substances Act in March 2000 although when sold as Xyrem it is considered Schedule III, making it the only drug to simultaneously occupy two different schedules. On March 20, 2001, the Commission on Narcotic Drugs placed GHB in Schedule IV of the 1971 Convention on Psychotropic Substances. In the UK it was made a class C drug in June 2003.
In New Zealand and Australia, GHB, 1,4-B and GBL are all Class B illegal drugs, along with any possible esters, ethers and aldehydes. GABA itself is also listed as an illegal drug in these jurisdictions which seems unusual given its failure to cross the blood-brain barrier, but there was a perception among legislators that all known analogues should be covered as far as this was possible. Attempts to circumvent the illegal status of GHB have led to the sale of derivatives such as 4-methyl-GHB (gamma-hydroxyvaleric acid, GHV) and its prodrug form gamma-valerolactone (GVL), but these are also covered under the law by virtue of their being "substantially similar" to GHB or GBL and; so importation, sale, possession and use of these compounds is also considered to be illegal.
GHB in popular culture
| This article contains a list of miscellaneous information. Please relocate any relevant information into other sections or articles. (December 2007) |
In the "Murder In A Flash" episode of CSI: Miami, one of the victims, an 18-year-old boy, is found to have died from GHB intoxication. GHB is also named as "the date-rape drug" by one of the investigators, who also relates the information that males often take the drug to get high. In the matter of the GHB-related death, however, the victim had received the GHB without noticing it.
In the NCIS episode "Twisted Sister" GHB was used to drug Sarah McGee, Special Agent Timothy McGee's sister, into thinking that she committed a murder as a cover-up. A classmate, whom she despises, drugged her by adding it to her peanut butter.
In the pilot episode of Veronica Mars, Veronica tells us she was raped at a party when she was sixteen. At the end of episode 20, "M.A.D.", of season 1, Veronica discovers that she had been given GHB at the party and investigates that night in the following episode, "A Trip to the Dentist". This party is referenced throughout season one and is a major conflict for the character, which was revisited in the final episode of season 2 when she finally learned exactly who she was raped by that night.
The current season 3 of Veronica Mars centers around the main character's freshman year at Hearst College, where she investigates a string of GHB-related rapes on campus. An episode of Law and Order: Special Victims Unit involves a woman who is drugged with GHB by a vengeful colleague in hopes that the woman will be raped. In the Law & Order episode "Fools for Love," one of the victim's deaths is attributed to choking on vomit from a GHB overdose administered by her rapist/killer.
The television series The West Wing featured GHB in a multi-episode story during the conclusion of season 4 and the beginning of season 5. The president's daughter consumes GHB that had been slipped into an alcoholic beverage without her knowledge, and, as she feels the effects of the drug, her boyfriend implies that she has consumed ecstasy. Later, she is kidnapped from a nightclub bathroom while barely or not conscious, setting off a massive manhunt. The president is told later by an FBI agent that the drug is created by mixing degreasing solvent and drain cleaner, and he finishes the agent's sentence by acknowledging he is aware the drug is known as a date-rape drug.
The French activist and psychoanalytic theorist Félix Guattari used GHB recreationally in the early 1970s, see The Anti-Oedipus Papers (2006:308,326)
Near the end of the second season of the television series Everwood, leading character Amy Abbott is pressured into consuming a low dose of GHB dissolved in water with her then-boyfriend, allegedly-recovered addict Tommy Callahan. In a misguided effort to keep her from accidentally overdosing, he consumes most of the drugs before giving her the remainder, thus overdosing himself. Upon realizing he was unresponsive, Amy called her doctor father to come to his rescue, and, while they succeeded in saving Tommy's life, this encounter with the controlled substance ended their relationship.
An episode of the fifth series of Spooks shows Ros using a refined form of the drug to incapacitate targets for intelligence gathering.
In the third episode of the American version of "Queer as Folk," the character Ted falls into a coma after being given a large dose of GHB by a date he brings home.
In the popular funk song "Party Song" by Brady's Bunch, GHB is referenced in a clever line: "A to the B to the C to the D to the E to the F to the GHB." The song also references "Hangin' out with my Georgia Homeboy."
In the song "What's Going On" by Zebrahead, found on their album Playmate of the Year (2000), GHB is referenced as a date rape drug: She takes another sip/ But has no clue of the spike from the G to the H to the B/ She wakes up in the morning/ bruised and raped in the street. GHB is referred to in the song Shores of California by The Dresden Dolls: And that is why the girl is called a tease / and that is why the guy is called a sleaze / and that's why God made escort agencies / one life to live and mace and GHB.
On the Billy Idol album 'Cyberpunk' (1993), on the song 'Then the Night Comes', GHB is mentioned at 2:30 into the song, as follows...'I take some GHB, I feel love, joy, And wonderful ringing music, Now, I just got to be me'. Following the album's release, he (Idol) almost died of a GHB overdose in 1994.
In The Anniversary, by Amy Gutman, GHB is referenced as a date rape drug.
References
- ^ http://erowid.org/chemicals/ghb/ghb_law.shtml
- http://stocks.us.reuters.com/stocks/fullDescription.asp?rpc=66&symbol=JAZZ.O
- ^ Theodore I Benzer (January 8, 2007). "Toxicity, Gamma-Hydroxybutyrate". eMedicine.
{{cite web}}: Check date values in:|date=(help) - e.g., sodium gamma-hydroxybutyrate (Na.GHB, sodium oxybate) or potassium gamma-hydroxybutyrate (K.GHB)
- 1874 Saizew,A. JLACBF Justus Liebigs Ann. Chem. 171 274.
- Michael Perry, James Pomfret, Roger Crabb (Nov 7, 2007). "Australia bans China-made toy on toxic drug risk". Reuter.
{{cite news}}: CS1 maint: multiple names: authors list (link) - http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=15567424&ordinalpos=25&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.bio.net/bionet/mm/neur-sci/1999-May/038337.html
- http://www.ncbi.nlm.nih.gov/sites/entrez?db=pubmed&uid=16129424&cmd=showdetailview
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=14535954&ordinalpos=2&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=7791129&ordinalpos=5&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=1847191&ordinalpos=4&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=2173754&ordinalpos=9&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=8549640&ordinalpos=15&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=2691926&ordinalpos=2&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://jpet.aspetjournals.org/cgi/content/full/305/2/675
- An author/scientist Gian Luigi Gessa has been researching alcoholism and the effects of various drugs to persons afflicted with said disease for the past ten years. His studies in 1998 note that GHB, as a pharmaceutical aid, can be much less toxic and much more effective than the leading pharmaceutical compound (disulfiram).
- In clinical trials Xyrem significantly reduced cataplexy attacks at a dose of 6000–9000mg per night. This is around three times the dose used recreationally, but almost all narcolepsy patients in the clinical trials were already stabilized on CNS stimulants such as modafinil; in patients not prescribed modafinil, this dosage could be dangerous and should be reduced appropriately. Also the prescribing information for Xyrem states that patients should take the dose immediately before going to bed, and then a second dose 3–4 hours later. The maximum dose taken at one time should not exceed 4500 mg. Patients with hepatic insufficiency (compromised liver function) have slower clearance of GHB and require reduced doses, typically half the normal dose. Xyrem oral solution is standardised to 500 mg Na.GHB / 1 mL water, buffered to pH 7.5 with malic acid.
- Xyrem drug data sheet
- ^ Jones, C. Suspicious death related to gamma-hydroxybutyrate (GHB) toxicity (2001), Journal of Clinical Forensic Medicine Volume 8, Issue 2, June 2001, Pages 74-76.
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=10369321&ordinalpos=27&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.udel.edu/wellspring/SOS/drugs.htm
- http://www.ajcn.org/cgi/content/abstract/35/3/510
- http://www.blackwell-synergy.com/doi/abs/10.1111/j.1556-4029.2006.00074.x?journalCode=jfo
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=9373886&ordinalpos=1&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVAbstractPlus
- "Muscarinic cholinergic mediation of the GH response to gamma-hydroxybutyric acid: neuroendocrine evidence in normal and parkinsonian subjects".
- http://www.nature.com/npp/journal/v11/n4/abs/1380135a.html
- http://lib.bioinfo.pl/pmid:9692734
- Rarediseases.org
- http://www.fasebj.org/cgi/content/full/17/12/1691
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=14535954&ordinalpos=2&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7914168&dopt=Abstract
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=10381791&ordinalpos=13&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=12965243&ordinalpos=3&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
- Elliott S, Burgess V. The presence of gamma-hydroxybutyric acid (GHB) and gamma-butyrolactone (GBL) in alcoholic and non-alcoholic beverages. Forensic Science International. 2005 July 16;151(2-3):289-92.
- Zvosec et al. American Academy of Forensic Science in Seattle, 2006
- Science and Technology Committee Report (page 176), 2006).
- Allen, L. (2006-04-01). "Gammahydroxybutyrate overdose and physostigmine". Emergency Medicine Journal. 23 (4): 300. doi:10.1136/emj.2006.035139.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Michael, H. (2005-01-01). "Endotracheal intubation in γ-hydroxybutyric acid intoxication and overdose". Emergency Medicine Journal. 22 (1): 43. doi:10.1136/emj.2004.021154.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Carai, M.A.M. (2005). "Resuscitative Effect of a γ-Aminobutyric Acid B Receptor Antagonist on γ-Hydroxybutyric Acid Mortality in Mice". Annals of Emergency Medicine. 45 (6): 614–619. doi:10.1016/j.annemergmed.2004.12.013.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - National Toxicology Program (March 1992), "Toxicology and Carcinogenesis Studies of g-Butyrolactone (CAS No. 96-48-0) in F344/N Rats and B6C3F1 Mice (Gavage Studies)", NTP Study Reports, Department of Health and Human Services, NIH
{{citation}}: CS1 maint: year (link) - ProjectGHB.org
- Whitehousedrugpolicy.org
External links
- GHB fact sheet
- EMCDDA Report on the risk assessment of GHB in the framework of the joint action on new synthetic drugs
- Articles from Steven Fowkes MD
- The Truth
- streetdrugs.com
- Erowid GHB Vault (contains also information about addiction and dangers)
- InfoFacts - Rohypnol and GHB (National Institute on Drug Abuse)
- GHB alternatives
- Pubmed/Medline search on sodium oxybate and alcohol-related disorders