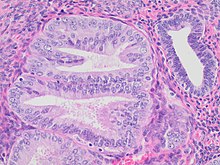
- Architectural gland crowding
- Altered cytology relative to background glands
- Minimum size of 1 mm
- Exclusion of adenocarcinoma
- Exclusion of mimics
Mitoses should also preferably be seen. Compare to normal endometrial gland at right.
Endometrial intraepithelial neoplasia (EIN) is a premalignant lesion of the uterine lining that predisposes to endometrioid endometrial adenocarcinoma. It is composed of a collection of abnormal endometrial cells, arising from the glands that line the uterus, which have a tendency over time to progress to the most common form of uterine cancer—endometrial adenocarcinoma, endometrioid type.
History
EIN lesions have been discovered by a combination of molecular, histologic, and clinical outcome studies beginning in the 1990s which provide a multifaceted characterization of this disease. They are a subset of a larger mixed group of lesions previously called "endometrial hyperplasia". The EIN diagnostic schema is intended to replace the previous "endometrial hyperplasia" classification as defined by the World Health Organization in 1994, which have been separated into benign (benign endometrial hyperplasia) and premalignant (EIN) classes in accordance with their behavior and clinical management.
EIN should not be confused with an unrelated entity, serous intraepithelial carcinoma ("serous EIC"), which is an early stage of a different tumor type known as papillary serous adenocarcinoma that also occurs in the same location within the uterus.
Clinical aspects
The average age at time of EIN diagnosis is approximately 52 years, compared to approximately 61 years for carcinoma. The timeframe and likelihood of EIN progression to cancer, however, is not constant amongst all women. Some cases of EIN are first detected as residual premalignant disease in women who already have carcinoma, whereas other EIN lesions disappear entirely and never lead to cancer. For this reason, treatment benefits and risks must be individualized for each patient under the guidance of an experienced physician.
Risk factors for development of EIN and the endometrioid type of endometrial carcinoma include exposure to estrogens without opposing progestins, obesity, diabetes, and rare hereditary conditions such as hereditary nonpolyposis colorectal cancer. Protective factors include use of combined oral contraceptive pills (low dose estrogen and progestin), and prior use of a contraceptive intrauterine device.
Biology
EIN lesions demonstrate all of the behaviors and characteristics of a premalignant, or precancerous, lesion.
Precancer Features of EIN (Table I). The cells of an EIN lesion are genetically different than normal and malignant tissues, and have a distinctive appearance under the light microscope. EIN cells are already neoplastic, demonstrating a monoclonal growth pattern and clonally distributed mutations. Progression of EIN to carcinoma, effectively a conversion from a benign neoplasm to a malignant neoplasm, is accomplished through acquisition of additional mutations and accompanied by a change in behavior characterized by the ability to invade local tissues and metastasize to regional and distant sites.
Table I: Precancer Characteristics of EIN
| Precancer Characteristics | EIN Evidence |
|---|---|
| Precancers differ from normal tissue |
|
| Precancers share some, but not all, features of cancer |
|
| Precancers increase risk for carcinoma |
|
| Precancers can be diagnosed |
|
| Cancer must arise from cells within the precancer |
|
EIN Biomarkers. (Figure 1). There are no single biomarkers which are completely informative in recognition of EIN. The tumour suppressor gene PTEN is frequently inactivated in EIN, being abnormally turned off in approximately 2/3 of all EIN lesions. This can be seen with special tissue stains applied to histological sections known as PTEN immunohistochemistry, in which the brown PTEN protein is seen to be absent in the crowded tubular glands that make up an EIN lesion.
Diagnosis
Diagnosis of EIN lesions is of clinical importance because of the increased risk of coexisting (39% of women with EIN will be diagnosed with carcinoma within one year) or future (the long term endometrial cancer risk is 45 times greater for a woman with EIN compared to one with only a benign endometrial histology) endometrial cancer. Diagnostic terminology is that used by pathologists, physicians who diagnose human disease by examination of histologic preparations of excised tissues. Critical distinctions in EIN diagnosis are separation from benign conditions such as benign endometrial hyperplasia (a field effect in endometrial tissue caused by excessive stimulation by the hormone estrogen), and cancer.
The spectrum of disease which must be distinguished from EIN (Table II) includes benign endometrial hyperplasia and carcinoma:
Table II: Disease classes that need to be distinguished from EIN.
| Disease Class |
Endometrial Topography |
Functional Category |
Treatment |
|---|---|---|---|
| Benign endometrial hyperplasia |
Diffuse | Hormone (estrogen) Effect |
Hormonal therapy |
| EIN, Endometrial Intraepithelial Neoplasia |
Focal progressing to diffuse (clonal) |
Precancer | Hormonal or surgical |
| Endometrial Adenocarcinoma |
Focal progressing to diffuse (clonal) |
Cancer | Surgical stage-based |
EIN may be diagnosed by a trained pathologist by examination of tissue sections of the endometrium. All of the following diagnostic criteria must be met in a single area of one tissue fragment to make the diagnosis (Table III).
Table III: EIN diagnosis.
| EIN Criterion | Comments | |
|---|---|---|
| 1 | Architecture | Gland area exceeds that of stroma, usually in a localized region. |
| 2 | Cytological Alterations |
Cytology differs between architecturally crowded focus and background. |
| 3 | Size greater than 1mm | Minimum linear dimension should exceed 1mm. Smaller lesions have unknown natural history. |
| 4 | Exclude mimics | Basalis, normal secretory, polyps, repair, lower uterine segment, cystic atrophy, tangential sections, menstrual collapse, disruption artifact, etc. |
| 5 | Exclude Cancer | Carcinoma should be diagnosed if: glands are mazelike and rambling, there are solid areas of epithelial growth, or there are significant bridges or cribriform areas. |
See also
References
- Owings, Richard A.; Quick, Charles M. (2014). "Endometrial Intraepithelial Neoplasia". Archives of Pathology & Laboratory Medicine. 138 (4): 484–491. doi:10.5858/arpa.2012-0709-RA. ISSN 1543-2165.
- Mutter GL, Duska L, Crum CP (2005). "Endometrial Intraepithelial Neoplasia". In Crum CP, Lee K (eds.). Diagnostic Gynecologic and Obstetric Pathology. Philadelphia PA: Saunders. pp. 493–518.
- ^ Silverberg SG, Mutter GL, Kurman RJ, Kubik-Huch RA, Nogales F, Tavassoli FA (2003). "Tumors of the uterine corpus: epithelial tumors and related lesions". In Tavassoli FA, Stratton MR (eds.). WHO Classification of Tumors: Pathology and Genetics of Tumors of the Breast and Female Genital Organs. Lyon, France: IARC Press. pp. 221–232.
- ^ Mutter GL, Baak JP, Crum CP, Richart RM, Ferenczy A, Faquin WC (March 2000). "Endometrial precancer diagnosis by histopathology, clonal analysis, and computerized morphometry". J. Pathol. 190 (4): 462–9. doi:10.1002/(SICI)1096-9896(200003)190:4<462::AID-PATH590>3.0.CO;2-D. PMID 10699996. S2CID 30636750.
- Jovanovic AS, Boynton KA, Mutter GL (April 1996). "Uteri of women with endometrial carcinoma contain a histopathological spectrum of monoclonal putative precancers, some with microsatellite instability". Cancer Res. 56 (8): 1917–21. PMID 8620514.
- ^ Mutter GL, Chaponot ML, Fletcher JA (February 1995). "A polymerase chain reaction assay for non-random X chromosome inactivation identifies monoclonal endometrial cancers and precancers". Am. J. Pathol. 146 (2): 501–8. PMC 1869842. PMID 7856759.
- ^ Esteller M, García A, Martínez-Palones JM, Xercavins J, Reventós J (January 1997). "Detection of clonality and genetic alterations in endometrial pipelle biopsy and its surgical specimen counterpart". Lab. Invest. 76 (1): 109–16. PMID 9010454.
- Mutter GL, Boynton KA (November 1995). "X chromosome inactivation in the normal female genital tract: implications for identification of neoplasia". Cancer Res. 55 (21): 5080–4. PMID 7585555.
- ^ Esteller M, Catasus L, Matias-Guiu X, et al. (November 1999). "hMLH1 promoter hypermethylation is an early event in human endometrial tumorigenesis". Am. J. Pathol. 155 (5): 1767–72. doi:10.1016/S0002-9440(10)65492-2. PMC 1866976. PMID 10550333.
- ^ Pontzer CH, Bazer FW, Johnson HM (October 1991). "Antiproliferative activity of a pregnancy recognition hormone, ovine trophoblast protein-1". Cancer Res. 51 (19): 5304–7. PMID 1913653.
- ^ Mutter GL, Wada H, Faquin WC, Enomoto T (October 1999). "K-ras mutations appear in the premalignant phase of both microsatellite stable and unstable endometrial carcinogenesis". Mol. Pathol. 52 (5): 257–62. doi:10.1136/mp.52.5.257. PMC 395707. PMID 10748874.
- ^ Maxwell GL, Risinger JI, Gumbs C, et al. (June 1998). "Mutation of the PTEN tumor suppressor gene in endometrial hyperplasias". Cancer Res. 58 (12): 2500–3. PMID 9635567.
- ^ Sasaki H, Nishii H, Takahashi H, et al. (April 1993). "Mutation of the Ki-ras protooncogene in human endometrial hyperplasia and carcinoma". Cancer Res. 53 (8): 1906–10. PMID 8467512.
- ^ Levine RL, Cargile CB, Blazes MS, van Rees B, Kurman RJ, Ellenson LH (August 1998). "PTEN mutations and microsatellite instability in complex atypical hyperplasia, a precursor lesion to uterine endometrioid carcinoma". Cancer Res. 58 (15): 3254–8. PMID 9699651.
- ^ Mutter GL, Boynton KA, Faquin WC, Ruiz RE, Jovanovic AS (October 1996). "Allelotype mapping of unstable microsatellites establishes direct lineage continuity between endometrial precancers and cancer". Cancer Res. 56 (19): 4483–6. PMID 8813144.
- ^ Mutter GL, Lin MC, Fitzgerald JT, et al. (June 2000). "Altered PTEN expression as a diagnostic marker for the earliest endometrial precancers". J. Natl. Cancer Inst. 92 (11): 924–30. doi:10.1093/jnci/92.11.924. PMID 10841828.
- ^ Duggan BD, Felix JC, Muderspach LI, Tsao JL, Shibata DK (March 1994). "Early mutational activation of the c-Ki-ras oncogene in endometrial carcinoma". Cancer Res. 54 (6): 1604–7. PMID 8137266.
- ^ Esteller M, Levine R, Baylin SB, Ellenson LH, Herman JG (November 1998). "MLH1 promoter hypermethylation is associated with the microsatellite instability phenotype in sporadic endometrial carcinomas". Oncogene. 17 (18): 2413–7. doi:10.1038/sj.onc.1202178. PMID 9811473.
- Doherty T, Connell J, Stoerker J, Markham N, Shroyer AL, Shroyer KR (September 1995). "Analysis of clonality by polymerase chain reaction for phosphoglycerate kinase-1. Heteroduplex generator". Diagn. Mol. Pathol. 4 (3): 182–90. doi:10.1097/00019606-199509000-00005. PMID 7493137.
- Shroyer KR, Gudlaugsson EG (March 1994). "Analysis of clonality in archival tissues by polymerase chain reaction amplification of PGK-1". Hum. Pathol. 25 (3): 287–92. doi:10.1016/0046-8177(94)90201-1. PMID 8150459.
- ^ Baak JP, Mutter GL, Robboy S, et al. (June 2005). "The molecular genetics and morphometry-based endometrial intraepithelial neoplasia classification system predicts disease progression in endometrial hyperplasia more accurately than the 1994 World Health Organization classification system". Cancer. 103 (11): 2304–12. doi:10.1002/cncr.21058. PMC 2600877. PMID 15856484.
- Mutter GL. Endometrial Precancer Type Collection . http://www.endometrium.org 2000.
- Mutter GL (March 2000). "Endometrial intraepithelial neoplasia (EIN): will it bring order to chaos? The Endometrial Collaborative Group". Gynecol. Oncol. 76 (3): 287–90. doi:10.1006/gyno.1999.5580. PMID 10684697.
- Mutter GL (October 2000). "Histopathology of genetically defined endometrial precancers". Int. J. Gynecol. Pathol. 19 (4): 301–9. doi:10.1097/00004347-200010000-00002. PMID 11109157.
- Hecht JL, Ince TA, Baak JP, Baker HE, Ogden MW, Mutter GL (March 2005). "Prediction of endometrial carcinoma by subjective endometrial intraepithelial neoplasia diagnosis". Mod. Pathol. 18 (3): 324–30. doi:10.1038/modpathol.3800328. PMC 2573865. PMID 15529181.
External links
- American Cancer Society
- OncoLink an educational site from the U. of Pennsylvania
- www.endometrium.org a pathology site focusing on endometrial disease
PTEN Gene
- Cancer Genetics Web PTEN entry
- PTEN and the Endometrium at PubMed
- Entrez Gene PTEN entry