This article is about a genus of bacteria. For the species causing atypical pneumonia, see Mycoplasma pneumoniae. Not to be confused with Mycobacteria.
| It has been suggested that anything not having to do with the current Mycoplasma, i.e. everything except the two Phylogeny trees and the infobox be split out into another article titled Mollicutes. (Discuss) (November 2023) |
| Mycoplasma | |
|---|---|
| |
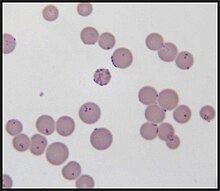
| Mycoplasma haemofelis | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Mycoplasmatota |
| Class: | Mollicutes |
| Order: | Mycoplasmatales |
| Family: | Mycoplasmataceae |
| Genus: | Mycoplasma J.Nowak 1929 |
| Type species | |
| Mycoplasma mycoides (Borrel et al. 1910) Freundt 1955 (Approved Lists 1980) | |
| Species | |
|
See text | |
| Synonyms | |
| |
| Mycoplasmosis | |
|---|---|
| Specialty | Infectious disease |
Mycoplasma is a genus of bacteria that, like the other members of the class Mollicutes, lack a cell wall, and its peptidoglycan, around their cell membrane. The absence of peptidoglycan makes them naturally resistant to antibiotics such as the beta-lactam antibiotics that target cell wall synthesis. They can be parasitic or saprotrophic. Several species are pathogenic in humans, including M. pneumoniae, which is an important cause of "walking" pneumonia and other respiratory disorders, and M. genitalium, which is believed to be involved in pelvic inflammatory diseases. Mycoplasma species (like the other species of the class Mollicutes) are among the smallest organisms yet discovered, can survive without oxygen, and come in various shapes. For example, M. genitalium is flask-shaped (about 300 x 600 nm), while M. pneumoniae is more elongated (about 100 x 1000 nm), many Mycoplasma species are coccoid. Hundreds of Mycoplasma species infect animals.
In casual speech, the name "mycoplasma" (plural mycoplasmas or mycoplasms) generally refers to all members of the class Mollicutes. In formal scientific classification, the designation Mycoplasma refers exclusively to the genus, a member of the Mycoplasmataceae, the only family in the order Mycoplasmatales (see "scientific classification").
Etymology
The term "mycoplasma", from the Greek μύκης, mykes (fungus) and πλάσμα, plasma (formed), was first used by Albert Bernhard Frank in 1889 to describe an altered state of plant cell cytoplasm resulting from infiltration by fungus-like microorganisms. Julian Nowak later proposed the name mycoplasma for certain filamentous microorganisms imagined to have both cellular and acellular stages in their lifecycles, which could explain how they were visible with a microscope, but passed through filters impermeable to other bacteria. Later, the name for these mycoplasmas was pleuropneumonia-like organisms (PPLO), broadly referring to organisms similar in colonial morphology and filterability to the causative agent (a Mycoplasma species) of contagious bovine pleuropneumonia. At present, all these organisms are classified as Mollicutes, and the term Mycoplasma solely refers to the genus.
Species which infect humans
Species of Mycoplasma, other than those listed below, have been recovered from humans, but are assumed to have been contracted from a non-human host. The following species use humans as the primary host:
- M. amphoriforme
- M. buccale
- M. faucium
- M. fermentans
- M. genitalium
- M. hominis
- M. incognitus
- M. lipophilum
- M. orale
- M. penetrans
- M. pirum
- M. pneumoniae
- M. primatum
- M. salivarium
- M. spermatophilum
Characteristics
Over 100 species have been included in the genus Mycoplasma, a member of the class Mollicutes. They are parasites or commensals of humans, animals, and plants. The genus Mycoplasma uses vertebrate and arthropod hosts. Dietary nitrogen availability has been shown to alter codon bias and genome evolution in Mycoplasma and the plant parasites Phytoplasma.
Mycoplasma species are among the smallest free-living organisms (about 0.2 - 0.3 μm in diameter). They have been found in the pleural cavities of cattle suffering from pleuropneumonia. These organisms are often called MLO (mycoplasma-like organisms) or, formerly, PPLO (pleuropneumonia-like organisms).
Important characteristics
- Cell wall is absent and plasma membrane forms the outer boundary of the cell.
- Due to the absence of cell walls these organisms can change their shape and leads to pleomorphism.
- Lack of nucleus and other membrane-bound organelles.
- Genetic material is a single DNA duplex and is naked.
- Ribosomes are 70S type.
- Possess a replicating disc at one end which assists replication process and also the separation of the genetic materials.
- Heterotrophic nutrition. Some live as saprophytes but the majority are parasites of plants and animals. The parasitic nature is due to the inability of mycoplasmal bacteria to synthesise the required growth factor.
Cell and colony morphology
Due to the lack of a rigid cell wall, Mycoplasma species (like all Mollicutes) can contort into a broad range of shapes, from round to oblong. They are pleomorphic and therefore cannot be identified as rods, cocci or spirochetes.

Colonies show the typical "fried egg" appearance (about 0.5 mm in diameter).
Reproduction
In 1954, using phase-contrast microscopy, continual observations of live cells have shown that Mycoplasma species ("mycoplasmas", formerly called pleuropneumonia-like organisms, PPLO, now classified as Mollicutes) and L-form bacteria (previously also called L-phase bacteria) do not proliferate by binary fission, but by a uni- or multi-polar budding mechanism. Microphotograph series of growing microcultures of different strains of PPLOs, L-form bacteria and, as a control, a Micrococcus species (dividing by binary fission) have been presented. Additionally, electron microscopic studies have been performed.
Taxonomy
History of taxonomy
Previously, Mycoplasma species (often commonly called "mycoplasmas", now classified as Mollicutes) were sometimes considered stable L-form bacteria or even viruses, but phylogenetic analysis has identified them as bacteria that have lost their cell walls in the course of evolution.
The medical and agricultural importance of members of the genus Mycoplasma and related genera have led to the extensive cataloging of many of these organisms by culture, serology, and small sub-unit rRNA gene and whole-genome sequencing. A recent focus in the sub-discipline of molecular phylogenetics has both clarified and confused certain aspects of the organization of the class Mollicutes.
Originally, the trivial name "mycoplasmas" commonly denoted all members of the class Mollicutes (from Latin mollis "soft" and cutis "skin"), which lack cell walls due to their genetic inability to synthesize peptidoglycan.
Taxonomists once classified Mycoplasma and relatives in the phylum Firmicutes, consisting of low G+C Gram-positive bacteria such as Clostridium, Lactobacillus, and Streptococcus; but modern polyphasic analyses situate them in the phylum Tenericutes.
Historically, the description of a bacterium lacking a cell wall was sufficient to classify it to the genus Mycoplasma and as such it is the oldest and largest genus of the class with about half of the class' species (107 validly described), each usually limited to a specific host and with many hosts harboring more than one species, some pathogenic and some commensal. In later studies, many of these species were found to be phylogenetically distributed among at least three separate orders. A limiting criterion for inclusion within the genus Mycoplasma was that the organism has a vertebrate host.
By the 1990s, it had become readily apparent that this approach was problematic: the type species, M. mycoides, along with other significant mycoplasma species like M. capricolum, is evolutionarily more closely related to the genus Spiroplasma in the order Entomoplasmatales than to the other members of the genus Mycoplasma. As a result, if the group was to be rearranged to match phylogeny, a number of medically important species (e.g. M. pneumoniae, M. genitalium) would have to be put in a different genus, causing widespread confusion in medical and agricultural communities. The genus was discussed multiple times by the International Committee on Systematic Bacteriology's (ICSB) subcommittee on Mollicutes between 1992 and 2011, to no effect.
Regardless of taxonomy, by 2007 it was solidly known that Molicutes could be divided into four nontaxonomic lineages.
- An "Acholeplasma" group consisting of Acholeplasmatales. This group is non-problematic, as it contains no species classified in what was then "Mycoplasma".
- A "Spiroplasma" or mycoides group containing M. mycoides and the aforementioned closely-related species in "Spiroplasma" and Entomoplasmatales.
- A pneumoniae group containing M. pneumoniae and closely-related species (M. muris, M. fastidiosum, U. urealyticum), the currently unculturable haemotrophic mollicutes, informally referred to as haemoplasmas (recently transferred from the genera Haemobartonella and Eperythrozoon), and Ureaplasma. This medically important group contains M. alvi (bovine), M. amphoriforme (human), M. gallisepticum (avian), M. genitalium (human), M. imitans (avian), M. pirum (uncertain/human), M. testudinis (tortoises), and M. pneumoniae (human). Most, if not all, of these species share some otherwise unique characteristics including an attachment organelle, homologs of the M. pneumoniae cytadherence-accessory proteins, and specialized modifications of the cell division apparatus.
- A hominis group containing M. hominis, M. bovis, and M. pulmonis among others.
As of 2018
In 2018, Gupta et al. re-circumscribed the genus Mycoplasma around M. mycoides. A total of 78 species were removed from Mycoplasma, creating five new genera and a number of higher taxonomic levels. Under this new scheme, a new family Mycoplasmoidaceae was created to correspond to the "pneumoniae" group, with M. pneumoniae and related species transferred to a new genus Mycoplasmoides. Another new family Metamycoplasmataceae was created to correspond to the "hominis" group. Both families belong to a new order Mycoplasmoitales, distinct from the Mycoplasmatales of Mycoplasma. The taxonomy was accepted by the ICSB with validation list 184 in 2018 and became the correct name. Both List of Prokaryotic names with Standing in Nomenclature (LPSN) and National Center for Biotechnology Information (NCBI) now use the new nomenclature.
Gupta's proposed taxonomy, as expected, moved the medically important "pneumoniae" group out of Mycoplasma into its own genus. As a result, a number of mycoplasmologists petitioned to the ICSB to reject the name in 2019. They argue that although Gupta's phylogenetic methods were likely solid, the proposed name changes are too sweeping to be practically adopted, citing some principles of the Code such as "name stability". Gupta and Oren wrote a rebuttal in 2020, further detailing the pre-existing taxonomic problems. In 2022, the ICSP's Judicial Opinion 122 ruled in favor of the name changes proposed by Gupta, meaning they remain valid under the Prokaryotic Code (and for the purpose of the LPSN, they remain the "correct names"). However, the older names also remain valid; their use remains acceptable under the Code.
Gupta et al. 2019 performed some uncontroversial sorting of the order Mycoplasmatales.
| 16S rRNA based LTP_08_2023 | 120 marker proteins based GTDB 08-RS214 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
Unassigned species:
- "Ca. M. aoti" Barker et al. 2011
- "M. bradburyae" Ramírez et al. 2023
- "Ca. M. corallicola" Neulinger et al. 2009
- "Ca. M. coregoni" corrig. Rasmussen et al. 2021
- "Ca. M. didelphidis" corrig. Pontarolo et al. 2021
- "Ca. M. erythrocervae" Watanabe et al. 2010
- "Ca. M. haematocervi" corrig. Watanabe et al. 2010
- "Ca. M. haematodidelphidis" corrig. Messick et al. 2002
- "Ca. M. haematohydrochoeri" corrig. Vieira et al. 2021
- "Ca. M. haematomacacae" corrig. Maggi et al. 2013
- "Ca. M. haematominiopteri" corrig. Millán et al. 2015
- "M. haematomyotis" Volokhov et al. 2023
- "M. haematophyllostomi" Volokhov et al. 2023
- "Ca. M. haematonasuae" corrig. Collere et al. 2021
- "Ca. M. haematoparvum" Sykes et al. 2005
- "Ca. M. haematosphigguri" corrig. Valente et al. 2021
- "Ca. M. haematotapirus" Mongruel et al. 2022
- "Ca. M. haematoterrestris" Mongruel et al. 2022
- "Ca. M. haematovis" corrig. Hornok et al. 2009
- "Ca. M. haemoalbiventris" Pontarolo et al. 2021
- "Ca. M. haemobovis" Meli et al. 2010
- "Ca. M. haemomeles" Harasawa, Orusa & Giangaspero 2014
- "Ca. M. haemomuris" (Mayer 1921) Neimark et al. 2002
- "Ca. M. haemoparvum" Kenny et al. 2004
- M. hafezii Ziegler et al. 2019
- "M. incognitus" Lo et al. 1989
- "M. insons" May et al. 2007
- "Ca. M. kahanei" Neimark et al. 2002
- "Ca. M. mahonii" Aroh, Liles & Halanych 2023
- "M. monodon" Ghadersohi & Owens 1998
- M. phocimorsus Skafte-Holm et al. 2023
- "M. pneumophila" Lyerova et al. 2008
- "Ca. M. ravipulmonis" Neimark, Mitchelmore & Leach 1998
- "Ca. M. salmoniarum" corrig. Rasmussen et al. 2021
- M. seminis Fischer et al. 2021
- "M. sphenisci" Frasca et al. 2005
- "M. timone" Greub & Raoult 2001
- "Ca. M. tructae" Sanchez et al. 2020
- "Ca. M. turicense" corrig. Willi et al. 2006
- "M. volis" Dillehay et al. 1995
- "M. vulturii" Oaks et al. 2004
Laboratory contaminant
Mycoplasma species are often found in research laboratories as contaminants in cell culture. Mycoplasmal cell culture contamination occurs due to contamination from individuals or contaminated cell culture medium ingredients. Mycoplasma cells are physically small – less than 1 μm, so are difficult to detect with a conventional microscope.
Mycoplasmae may induce cellular changes, including chromosome aberrations, changes in metabolism and cell growth. Severe Mycoplasma infections may destroy a cell line. Detection techniques include DNA probe, enzyme immunoassays, PCR, plating on sensitive agar and staining with a DNA stain including DAPI or Hoechst.
An estimated 11 to 15% of U.S. laboratory cell cultures are contaminated with mycoplasma. A Corning study showed that half of U.S. scientists did not test for Mycoplasma contamination in their cell cultures. The study also stated that, in former Czechoslovakia, 100% of cell cultures that were not routinely tested were contaminated while only 2% of those routinely tested were contaminated (study p. 6). Since the U.S. contamination rate was based on a study of companies that routinely checked for Mycoplasma, the actual contamination rate may be higher. European contamination rates are higher and that of other countries are higher still (up to 80% of Japanese cell cultures). About 1% of published Gene Expression Omnibus data may have been compromised. Several antibiotic-containing formulations of antimycoplasmal reagents have been developed over the years.
Synthetic mycoplasma genome
A chemically synthesized genome of a mycoplasmal cell based entirely on synthetic DNA which can self-replicate has been referred to as Mycoplasma laboratorium.
Pathogenicity
Several Mycoplasma species can cause disease, including M. pneumoniae, which is an important cause of atypical pneumonia (formerly known as "walking pneumonia"), and M. genitalium, which has been associated with pelvic inflammatory diseases. Mycoplasma infections in humans are associated with skin eruptions in 17% of cases.
P1 antigen
The P1 antigen is the primary virulence factor of mycoplasma, specifically the Pneumoniae group. P1 is a membrane associated protein that allows adhesion to epithelial cells. The P1 receptor is also expressed on erythrocytes which can lead to autoantibody agglutination from mycobacteria infection.
Sexually transmitted infections
Mycoplasma and Ureaplasma species are not part of the normal vaginal flora. Some Mollicutes species are spread through sexual contact. These species have a negative effect on fertility. Mollicutes species colonizing the human genital tract are:
- U. urealyticum
- M. hominis
- M. genitalium
- M. penetrans
- M. primatum (considered nonpathogenic)
- M. spermatophilum (considered nonpathogenic)
M. hominis causes male sterility/Genitals inflammation in humans.
Mycoplasma species have been isolated from women with bacterial vaginosis. M. genitalium is found in women with pelvic inflammatory disease. In addition, infection is associated with increased risk of cervicitis, infertility, preterm birth and spontaneous abortion. Mycoplasma genitalium has developed resistance to some antibiotics.
Infant disease
Low birth-weight, preterm infants are susceptible to Mycoplasma and Ureaplasma infections. Mycoplasma species are associated with infant respiratory distress syndrome, bronchopulmonary dysplasia, and intraventricular hemorrhage in preterm infants.
Links to cancer
Several species of Mycoplasma are frequently detected in different types of cancer cells. These species are:
The majority of these Mycoplasma species have shown a strong correlation to malignant transformation in mammalian cells in vitro.
infection and host cell transformation
The presence of Mycoplasma was first reported in samples of cancer tissue in the 1960s. Since then, several studies tried to find and prove the connection between Mycoplasma and cancer, as well as how the bacterium might be involved in the formation of cancer. Several studies have shown that cells that are chronically infected with the bacteria go through a multistep transformation. The changes caused by chronic mycoplasmal infections occur gradually and are both morphological and genetic. The first visual sign of infection is when the cells gradually shift from their normal form to sickle-shaped. They also become hyperchromatic due to an increase of DNA in the nucleus of the cells. In later stages, the cells lose the need for solid support to grow and proliferate, as well as the normal contact-dependent inhibition cells.
Possible intracellular mechanisms
Karyotypic changes related to infections
Cells infected with Mycoplasma for an extended period of time show significant chromosomal abnormalities. These include the addition of chromosomes, the loss of entire chromosomes, partial loss of chromosomes, and chromosomal translocation. All of these genetic abnormalities may contribute to the process of malignant transformation. Chromosomal translocation and extra chromosomes help create abnormally high activity of certain proto-oncogenes, which caused by these genetic abnormalities and include those encoding c-myc, HRAS, and vav. The activity of proto-oncogenes is not the only cellular function that is affected; tumour suppressor genes are affected by the chromosomal changes induced by mycoplasma, as well. Partial or complete loss of chromosomes causes the loss of important genes involved in the regulation of cell proliferation. Two genes whose activities are markedly decreased during chronic infections with mycoplasma are the Rb and the p53 tumour suppressor genes. Another possible mechanism of carcinogenesis is RAC1 activation by a small GTPase-like protein fragment of Mycoplasma. A major feature that differentiates mycoplasmas from other carcinogenic pathogens is that the mycoplasmas do not cause the cellular changes by insertion of their own genetic material into the host cell. The exact mechanism by which the bacterium causes the changes is not yet known.
Partial reversibility of malignant transformations
The malignant transformation induced by Mycoplasma species is also different from that caused by other pathogens in that the process is reversible. The state of reversal is, however, only possible up to a certain point during the infection. The window of time when reversibility is possible varies greatly; it depends primarily on the Mycoplasma involved. In the case of M. fermentans, the transformation is reversible until around week 11 of infection and starts to become irreversible between weeks 11 and 18. If the bacteria are killed using antibiotics (i.e. ciprofloxacin or Clarithromycin) before the irreversible stage, the infected cells should return to normal.
Connections to cancer in vivo and future research
Epidemiologic, genetic, and molecular studies suggest infection and inflammation initiate certain cancers, including those of the prostate. M. genitalium and M. hyorhinis induce malignant phenotype in benign human prostate cells (BPH-1) that were not tumorigenic after 19 weeks of exposure.
Types of cancer associated
Colon cancer: In a study to understand the effects of Mycoplasma contamination on the quality of cultured human colon cancer cells, a positive correlation was found between the number of M. hyorhinis cells present in the sample and the percentage of CD133-positive cells (a glycoprotein with an unknown function).
Gastric cancer: Strong evidence indicates the infection of M. hyorhinis contributes to the development of cancer within the stomach and increases the likelihood of malignant cancer cell development.
Lung cancer: Studies on lung cancer have supported the belief that more than a coincidental positive correlation exists between the appearance of Mycoplasma strains in patients and the infection with tumorigenesis.
Prostate cancer: p37, a protein encoded for by M. hyorhinis, has been found to promote the invasiveness of prostate cancer cells. The protein also causes the growth, morphology, and gene expression of the cells to change, causing them to become a more aggressive phenotype.
Renal cancer: Patients with renal cell carcinoma (RCC) exhibited a significantly high amount of Mycoplasma sp. compared with the healthy control group. This suggests Mycoplasma may play a role in the development of RCC.
See also
- International Organization for Mycoplasmology (IOM)
- Sexually transmitted disease
- Vaginal flora
- Vaginal infection
- Vaginal disease
- Vaginal health
- Phytoplasma
- Smallest organisms
- List of bacterial orders
- List of bacteria genera
- Mycoplasma alligatori
References
- Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 409–12. ISBN 978-0-8385-8529-0.
- Richard L. Sweet, Ronald S. Gibbs (1985). Infectious Diseases of the Female Genital Tract. Lippincott Williams & Wilkins, 2009. ISBN 978-0-683-08038-4.
- ^ Larsen B, Hwang J (2010). "Mycoplasma, Ureaplasma, and Adverse Pregnancy Outcomes: A Fresh Look". Infectious Diseases in Obstetrics and Gynecology. 2010: 1–7. doi:10.1155/2010/521921. ISSN 1064-7449. PMC 2913664. PMID 20706675.
- Frank B (1889). "Ueber der Pilzsymbiose der Leguminosen" [On fungal symbioses of legumes]. Berichte der Deutschen Botanischen Gesellschaft (in German). 7: 332–346.
From p. 335: "Die durch die Infection entstandene veränderte Art des Plasmas in den Rindenzellen will ich, da sie offenbar durch die Vermischmung mit einem pilzartigen Wesen entstanden ist, als Mycoplasma bezeichnen." obviously arose by mixing with a fungal organism.]
- Krass CJ, Gardner MW (January 1973). "Etymology of the Term Mycoplasma". Int. J. Syst. Evol. Microbiol. 23 (1): 62–64. doi:10.1099/00207713-23-1-62.
- Browning G, Citti C, eds. (2014). Mollicutes Molecular Biology and Pathogenesis (1st ed.). Caister Academic Press. pp. 1–14. ISBN 978-1-908230-30-0.
- ^ Edward DG, Freundt EA (February 1956). "The classification and nomenclature of organisms of the pleuropneumonia group" (PDF). J. Gen. Microbiol. 14 (1): 197–207. doi:10.1099/00221287-14-1-197. PMID 13306904.
- ^ Waites KB, Katz B, Schelonka RL (2005). "Mycoplasmas and Ureaplasmas as Neonatal Pathogens". Clinical Microbiology Reviews. 18 (4): 757–789. CiteSeerX 10.1.1.336.7047. doi:10.1128/CMR.18.4.757-789.2005. ISSN 0893-8512. PMC 1265909. PMID 16223956.
- Maggi RG, Compton SM, Trull CL, Mascarelli PE, Mozayeni BR, Breitschwerdt EB (1 October 2013). "Infection with Hemotropic Mycoplasma Species in Patients with or without Extensive Arthropod or Animal Contact". Journal of Clinical Microbiology. 51 (10): 3237–3241. doi:10.1128/JCM.01125-13. PMC 3811635. PMID 23863574.
- Seward E, Kelly S (2016). "Dietary nitrogen alters codon bias and genome composition in parasitic microorganisms". Genome Biology. 17 (226): 3–15. doi:10.1186/s13059-016-1087-9. PMC 5109750. PMID 27842572.
- "Mycoplasma". The Lecturio Medical Concept Library. Retrieved 8 July 2021.
- ^ Kandler G, Kandler O (1954). "Untersuchungen über die Morphologie und die Vermehrung der pleuropneumonie-ähnlichen Organismen und der L-Phase der Bakterien. I. Lichtmikroskopische Untersuchungen" [Studies on morphology and multiplication of pleuropneumonia-like organisms and on bacterial L-phase, I. Light microscopy (now mycoplasmas and L-form bacteria)] (PDF). Archiv für Mikrobiologie (in German). 21 (2). (Article in English available): 178–201. Bibcode:1954ArMic..21..178K. doi:10.1007/BF01816378. PMID 14350641. S2CID 21257985.
- Gladwin M, Trattler W, Mahan CS (2014). Clinical Microbiology made ridiculously simple. Miami, Fl: MedMaster, Inc. p. 156. ISBN 978-1-935660-15-6.
- Kandler G, Kandler O, Huber O (1954). "Untersuchungen über die Morphologie und die Vermehrung der pleuropneumonie-ähnlichen Organismen und der L-Phase der Bakterien. II. Elektronenmikroskopische Untersuchungen" [Studies on morphology and multiplication of pleuropneumonia-like organisms and on bacterial L-phase, II. Electron microscopy (now mycoplasmas and L-form bacteria)] (PDF). Archiv für Mikrobiologie (in German). 21 (2). (Article in English available): 202–216. Bibcode:1954ArMic..21..202K. doi:10.1007/BF01816379. PMID 14350642. S2CID 45546531.
- Woese CR, Maniloff J, Zablen L (1980). "Phylogenetic analysis of the mycoplasmas" (PDF). Proceedings of the National Academy of Sciences of the United States of America. 77 (1): 494–498. Bibcode:1980PNAS...77..494W. doi:10.1073/pnas.77.1.494. PMID 692864.
- Johansson K-E, Pettersson B (2002). "Taxonomy of Mollicutes". Molecular Biology and Pathogenicity of Mycoplasmas (Razin S, Herrmann R, eds.). New York: Kluwer Academic/Plenum. pp. 1–30. ISBN 0-306-47287-2.
- Brown DR (2011). "Phylum XVI. Tenericutes Murray 1984a, 356VP". Bergey's Manual of Systematic Bacteriology, Second Edition, Vol. 4, (Krieg NR, Staley JT, Brown DR, et al., eds.). New York: Springer. pp. 567–568. ISBN 978-0-387-95042-6.
- ^ A.C. Parte, et al. "Mycoplasma". List of Prokaryotic names with Standing in Nomenclature (LPSN). Retrieved 9 September 2022.
- Oshima K, Nishida H (September 2007). "Phylogenetic relationships among mycoplasmas based on the whole genomic information". J. Mol. Evol. 65 (3): 249–58. Bibcode:2007JMolE..65..249O. doi:10.1007/s00239-007-9010-3. PMID 17687503.
- ^ Gupta R, Sawnani S, Adeolu M, Alnajar S, Oren A (2018). "Phylogenetic framework for the phylum Tenericutes based on genome sequence data: proposal for the creation of a new order Mycoplasmoidales ord. nov., containing two new families Mycoplasmoidaceae fam. nov. and Metamycoplasmataceae fam. nov. harbouring Eperythrozoon, Ureaplasma and five novel genera". Antonie van Leeuwenhoek. 111 (9): 1583–1630. doi:10.1007/s10482-018-1047-3. PMID 29556819. S2CID 254226604.
- Sayers, et al. "Mycoplasma". National Center for Biotechnology Information (NCBI) taxonomy database. Retrieved 9 September 2022.
- Balish M, Bertaccini A, Blanchard A, Brown D, Browning G, Chalker V, Frey J, Gasparich G, Hoelzle L, Knight T, Knox C, Chih-Horng K, Manso-Silván L, May M, Pollack J, Ramírez A, Spergser J, Taylor-Robinson D, Volokhov D, Zhao Y (2019). "Recommended rejection of the names Malacoplasma gen. nov., Mesomycoplasma gen. nov., Metamycoplasma gen. nov., Metamycoplasmataceae fam. nov., Mycoplasmoidaceae fam. nov., Mycoplasmoidales ord. nov., Mycoplasmoides gen. nov., Mycoplasmopsis gen. nov. [Gupta, Sawnani, Adeolu, Alnajar and Oren 2018] and all proposed species comb. nov. placed therein". International Journal of Systematic and Evolutionary Microbiology. 69 (11): 3650–3653. doi:10.1099/ijsem.0.003632. hdl:11585/720151. PMID 31385780.
- Gupta RS, Oren A (1 February 2020). "Necessity and rationale for the proposed name changes in the classification of Mollicutes species. Reply to: 'Recommended rejection of the names Malacoplasma gen. nov., Mesomycoplasma gen. nov., Metamycoplasma gen. nov., Metamycoplasmataceae fam. nov., Mycoplasmoidaceae fam. nov., Mycoplasmoidales ord. nov., Mycoplasmoides gen. nov., Mycoplasmopsis gen. nov. [Gupta, Sawnani, Adeolu, Alnajar and Oren 2018] and all proposed species comb. nov. placed therein', by M. Balish et al. (Int J Syst Evol Microbiol, 2019;69:3650–3653)". International Journal of Systematic and Evolutionary Microbiology. 70 (2): 1431–1438. doi:10.1099/ijsem.0.003869. PMID 31971499.
- ^ "Genus: Mycoplasmoides". lpsn.dsmz.de.; see also LPSN FAQ on correct name
- ^ Arahal DR, Busse HJ, Bull CT, Christensen H, Chuvochina M, Dedysh SN, Fournier PE, Konstantinidis KT, Parker CT, Rossello-Mora R, Ventosa A, Göker M (10 August 2022). "Judicial Opinions 112–122". International Journal of Systematic and Evolutionary Microbiology. 72 (8). doi:10.1099/ijsem.0.005481. PMID 35947640.
- Gupta RS, Son J, Oren A (April 2019). "A phylogenomic and molecular markers based taxonomic framework for members of the order Entomoplasmatales: proposal for an emended order Mycoplasmatales containing the family Spiroplasmataceae and emended family Mycoplasmataceae comprising six genera". Antonie van Leeuwenhoek. 112 (4): 561–588. doi:10.1007/s10482-018-1188-4. PMID 30392177.
- "The LTP". Retrieved 20 November 2023.
- "LTP_all tree in newick format". Retrieved 20 November 2023.
- "LTP_08_2023 Release Notes" (PDF). Retrieved 20 November 2023.
- "GTDB release 08-RS214". Genome Taxonomy Database. Retrieved 10 May 2023.
- "bac120_r214.sp_label". Genome Taxonomy Database. Retrieved 10 May 2023.
- "Taxon History". Genome Taxonomy Database. Retrieved 10 May 2023.
- LPSN lpsn.dsmz.de
- Drexler HG, Uphoff CC (2002). "Mycoplasma contamination of cell cultures: Incidence, sources, effects, detection, elimination, prevention". Cytotechnology. 39 (2): 75–90. doi:10.1023/A:1022913015916. PMC 3463982. PMID 19003295.
- Razin S (2001). Mycoplasmas. The University of Texas Medical Branch at Galveston. ISBN 978-0-9631172-1-2. PMID 21413254. Retrieved 8 July 2021 – via National Center for Biotechnology Information, U.S. National Library of Medicine.
- John Ryan (2008). "Understanding and Managing Cell Culture Contamination" (PDF). Corning Incorporated. p. 24. Archived from the original (PDF) on 8 July 2011. Retrieved 4 August 2010.
- Aldecoa-Otalora E, Langdon W, Cunningham P, Arno MJ (December 2009). "Unexpected presence of mycoplasma probes on human microarrays". BioTechniques. 47 (6): 1013–5. doi:10.2144/000113271. PMID 20047202.
- Link Archived 30 March 2012 at the Wayback Machine into RNAnet showing contamination of GEO. Press plot and drag blue crosshairs to expose links to description of experiments on human RNA samples
- BM-Cyclin Archived 2 February 2013 at archive.today by Roche, MRA by ICN, Plasmocin by Invivogen and more recently De-Plasma Archived 9 April 2013 at the Wayback Machine by TOKU-E.
- Gibson DG, Glass JI, Lartigue C, Noskov VN, Chuang RY, Algire MA, Benders GA, Montague MG, Ma L, Moodie MM, Merryman C, Vashee S, Krishnakumar R, Assad-Garcia N, Andrews-Pfannkoch C, Denisova EA, Young L, Qi ZQ, Segall-Shapiro TH, Calvey CH, Parmar PP, Hutchison CA, Smith HO, Venter JC (July 2010). "Creation of a bacterial cell controlled by a chemically synthesized genome". Science. 329 (5987): 52–6. Bibcode:2010Sci...329...52G. doi:10.1126/science.1190719. PMID 20488990.
- James, William D., Berger, Timothy G., et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- Parija SC (2014). Textbook of Microbiology & Immunology. Elsevier Health Sciences. ISBN 978-81-312-3624-6.
- ^ Ljubin-Sternak S, Mestrovic T (2014). "Review: Chlamydia trachonmatis and Genital Mycoplasmias: Pathogens with an Impact on Human Reproductive Health". Journal of Pathogens. 2014 (183167): 183167. doi:10.1155/2014/183167. PMC 4295611. PMID 25614838.
The term "mycoplasma" is often used to refer to any members of the class Mollicutes (for the purposes of this review as well), irrespective of the fact whether they truly belong to the genus Mycoplasma
- Wiesenfeld HC, Manhart LE (15 July 2017). "Mycoplasma genitalium in Women: Current Knowledge and Research Priorities for This Recently Emerged Pathogen". The Journal of Infectious Diseases. 216 (suppl_2): S389 – S395. doi:10.1093/infdis/jix198. ISSN 1537-6613. PMC 5853983. PMID 28838078.
- Lis R, Rowhani-Rahbar A, Manhart LE (2015). "Mycoplasma genitalium Infection and Female Reproductive Tract Disease: A Meta-Analysis". Clinical Infectious Diseases. 61 (3): 418–426. doi:10.1093/cid/civ312. hdl:1773/26479. ISSN 1058-4838. PMID 25900174.
- Mitjà O, Asiedu K, Mabey D (13 February 2013). "2013 Yaws Seminar" (PDF). Lancet. 381 (9868). The Lancet: 763–73. doi:10.1016/S0140-6736(12)62130-8. PMID 23415015. S2CID 208791874. Retrieved 28 March 2020 – via World Health Organization.
- ^ Huang S, Li JY, Wu J, Meng L, Shou CC (April 2001). "Mycoplasma infections and different human carcinomas". World Journal of Gastroenterology. 7 (2): 266–269. doi:10.3748/wjg.v7.i2.266. PMC 4723534. PMID 11819772.
- ^ Sinkovics JG (February 2012). "Molecular biology of oncogenic inflammatory processes. I. Non-oncogenic and oncogenic pathogens, intrinsic inflammatory reactions without pathogens, and microRNA/DNA interactions (Review)". International Journal of Oncology. 40 (2): 305–349. doi:10.3892/ijo.2011.1248. PMID 22076306.
- ^ Tsai S, Wear DJ, Shih JW, Lo SC (October 1995). "Mycoplasmas and oncogenesis: Persistent infection and multistage malignant transformation". Proceedings of the National Academy of Sciences of the United States of America. 92 (22): 10197–10201. Bibcode:1995PNAS...9210197T. doi:10.1073/pnas.92.22.10197. PMC 40763. PMID 7479753.
- ^ Cimolai N (August 2001). "Do mycoplasmas cause human cancer?". Canadian Journal of Microbiology. 47 (8): 691–697. doi:10.1139/w01-053. PMID 11575494.
- Jiang S, Zhang S, Langenfeld J, Lo SC, Rogers MB (May 2008). "Mycoplasma infection transforms normal lung cells and induces bone morphogenetic protein 2 expression by post-transcriptional mechanisms". Journal of Cellular Biochemistry. 104 (2): 580–594. doi:10.1002/jcb.21647. PMID 18059017. S2CID 23871175.
- ^ Zhang S, Tsai S, Lo SC (May 2006). "Alteration of gene expression profiles during mycoplasma-induced malignant cell transformation". BMC Cancer. 6: 116. doi:10.1186/1471-2407-6-116. PMC 1559712. PMID 16674811.
- ^ Namiki K, Goodison S, Porvasnik S, Allan RW, Iczkowski KA, Urbanek C, Reyes L, Sakamoto N, Rosser CJ (September 2009). "Persistent exposure to mycoplasma induces malignant transformation of human prostate cells". PLOS ONE. 4 (9): e6872. Bibcode:2009PLoSO...4.6872N. doi:10.1371/journal.pone.0006872. PMC 2730529. PMID 19721714.
- Chan PJ, Seraj IM, Kalugdan TH, King A (November 1996). "Prevalence of mycoplasma conserved DNA in malignant ovarian cancer detected using sensitive PCR–ELISA". Gynecologic Oncology. 63 (2): 258–260. doi:10.1006/gyno.1996.0316. PMID 8910637.
- Xiaolei C, Taot H, Zongli S, Hongying Y (2014). "The role of ureaplasma urealyticum infection in cervical intraepithelial neoplasia and cervical cancer". European Journal of Gynaecological Oncology. 35 (5): 571–5. PMID 25423707.
- Lopes BR, Ribeiro AG, Silva TF, Barbosa LV, Jesus TI, Matsuda BK, Costa MF, Toledo KA (February 2021). "Diagnosis and treatment of HEp-2 cells contaminated with mycoplasma". Brazilian Journal of Biology. 81 (1): 37–43. doi:10.1590/1519-6984.215721. hdl:11449/205878. ISSN 1678-4375. PMID 32321065.
- Hu X, Yu J, Zhou X, Li Z, Xia Y, Luo Z, Wu Y (January 2014). "A small GTPase-like protein fragment of Mycoplasma promotes tumor cell migration and proliferation in vitro via interaction with Rac1 and Stat3". Mol Med Rep. 9 (1): 173–179. doi:10.3892/mmr.2013.1766. PMID 24172987.
- ^ Pehlivan M, Pehlivan S, Onay H, Koyuncuoglu M, Kirkali Z (February 2005). "Can mycoplasma-mediated oncogenesis be responsible for formation of conventional renal cell carcinoma?". Urology. 65 (2): 411–414. doi:10.1016/j.urology.2004.10.015. PMID 15708077.
- Mariotti E, Gemei M, Mirabelli P, D'Alessio F, Di Noto R, Fortunato G, Del Vecchio L (March 2010). "The percentage of CD133+ cells in human colorectal cancer cell lines is influenced by Mycoplasma hyorhinis infection". BMC Cancer. 10: 120–125. doi:10.1186/1471-2407-10-120. PMC 2854114. PMID 20353562.
- Yang H, Qu L, Ma H, Chen L, Liu W, Liu C, Meng L, Wu J, Shou C (November 2010). "Mycoplasma hyorhinis infection in gastric carcinoma and its effects on the malignant phenotypes of gastric cancer cells". BMC Gastroenterology. 10: 132–140. doi:10.1186/1471-230X-10-132. PMC 2993648. PMID 21062494.
- Apostolou P, Tsantsaridou A, Papasotiriou I, Toloudi M, Chatziioannou M, Giamouzis G (October 2011). "Bacterial and fungal microflora in surgically removed lung cancer samples". Journal of Cardiothoracic Surgery. 6: 137. doi:10.1186/1749-8090-6-137. PMC 3212932. PMID 21999143.
- Urbanek C, Goodison S, Chang M, Porvasnik S, Sakamoto N, Li CZ, Boehlein SK, Rosser CJ (June 2011). "Detection of antibodies directed at M. hyorhinis p37 in the serum of men with newly diagnosed prostate cancer". BMC Cancer. 11 (1): 233–238. doi:10.1186/1471-2407-11-233. PMC 3129326. PMID 21663671.
External links
| Classification | D |
|---|
| Prokaryotes: Bacteria classification | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Terrabacteria BV1, BV3, BV5 |
| ||||||||||||||||||
| CPR group |
| ||||||||||||||||||
| Thermotogida |
| ||||||||||||||||||
| Fusobacterida |
| ||||||||||||||||||
| Hydrobacteria BV2, BV4 |
| ||||||||||||||||||
| others |
| ||||||||||||||||||
| |||||||||||||||||||
| Taxon identifiers | |
|---|---|
| Mycoplasma | |