| Hemangioblastoma | |
|---|---|
 | |
| Micrograph of a cerebellar hemangioblastoma. HPS stain. | |
| Specialty | Oncology |
Hemangioblastomas, or haemangioblastomas, are vascular tumors of the central nervous system that originate from the vascular system, usually during middle age. Sometimes, these tumors occur in other sites such as the spinal cord and retina. They may be associated with other diseases such as polycythemia (increased blood cell count), pancreatic cysts and Von Hippel–Lindau syndrome (VHL syndrome). Hemangioblastomas are most commonly composed of stromal cells in small blood vessels and usually occur in the cerebellum, brainstem or spinal cord. They are classed as grade I tumors under the World Health Organization's classification system.
Presentation
Complications
Hemangioblastomas can cause an abnormally high number of red blood cells in the bloodstream due to ectopic production of the hormone erythropoietin as a paraneoplastic syndrome.
Pathogenesis
Hemangioblastomas are composed of endothelial cells, pericytes and stromal cells. In VHL syndrome the von Hippel-Lindau protein (pVHL) is dysfunctional, usually due to mutation and/or gene silencing. In normal circumstances, pVHL is involved in the inhibition of hypoxia-inducible factor 1 α (HIF-1α) by ubiquitin mediated proteosomal degradation. In these dysfunctional cells pVHL cannot degrade HIF-1α, causing it to accumulate. HIF-1α causes the production of vascular endothelial growth factor, platelet derived growth factor B, erythropoietin and transforming growth factor alpha, which act to stimulate growth of cells within the tumor.
Diagnosis

The primary diagnosis is made with a computed tomography scan (CT scan). On a scan, hemangioblastoma shows as a well-defined, low attenuation region in the posterior fossa with an enhancing nodule on the wall. Sometimes multiple lesions are present.
Treatment
The treatment for hemangioblastoma is surgical excision of the tumor. Although usually straightforward to carry out, recurrence of the tumor or more tumors at a different site develop in approximately 20% of patients. Gamma Knife Radiosurgery as well as LINAC have also been employed to successfully treat recurrence and control tumor growth of cerebellar hemangioblastomas.
Prognosis
The outcome for hemangioblastoma is very good if surgical extraction of the tumor can be achieved; excision is possible in most cases and permanent neurologic deficit is uncommon and can be avoided altogether if the tumor is diagnosed and treated early. Persons with VHL syndrome have a bleaker prognosis than those who have sporadic tumors since those with VHL syndrome usually have more than one lesion.
Epidemiology
Hemangioblastoma are among the rarest central nervous system tumors, accounting for less than 2%. Hemangioblastomas usually occur in adults, yet tumors may appear in VHL syndrome at much younger ages. Men and women are approximately at the same risk. Although they can occur in any section of the central nervous system, they usually occur in either side of the cerebellum, the brain stem or the spinal cord.
Additional images
-
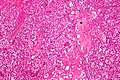 Micrograph of cerebellar hemangioblastoma. HPS stain.
Micrograph of cerebellar hemangioblastoma. HPS stain.
-
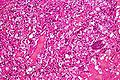 Micrograph of cerebellar hemangioblastoma. HPS stain.
Micrograph of cerebellar hemangioblastoma. HPS stain.
References
- ^ Lindsay, Kenneth W; Ian Bone; Robin Callander; J. van Gijn (1991). Neurology and Neurosurgery Illustrated. United States: Churchill Livingstone. ISBN 0-443-04345-0.
- ^ Louis, David N (1991). WHO Classification of Tumors of the Central Nervous System. IARC. ISBN 92-832-2430-2.
- Farrukh, HM (February 1996). "Cerebellar hemangioblastoma presenting as secondary erythrocytosis and aspiration pneumonia". The Western Journal of Medicine. 164 (2): 169–71. PMC 1303396. PMID 8775737.
- Kaelin, William G (2005). "von Hippel–Lindau-associated malignancies: Mechanisms and therapeutic opportunities". Drug Discovery Today: Disease Mechanisms. 2 (2): 225–231. doi:10.1016/j.ddmec.2005.04.003.
- "Hemangioblastoma". The Lecturio Medical Concept Library. Retrieved 24 July 2021.
- Silva, Danilo; Grabowski, Mathew M.; Juthani, Rupa; Sharma, Mayur; Angelov, Lilyana; Vogelbaum, Michael A.; Chao, Samuel; Suh, John; Mohammadi, Alireza; Barnett, Gene H. (September 2016). "Gamma Knife radiosurgery for intracranial hemangioblastoma". Journal of Clinical Neuroscience. 31: 147–151. doi:10.1016/j.jocn.2016.03.008. PMID 27422585. S2CID 19652430.
- Richard S, Campello C, Taillandier L, Parker F, Resche F (1998). "Haemangioblastoma of the central nervous system in von Hippel-Lindau disease. French VHL Study Group". J. Intern. Med. 243 (6): 547–53. doi:10.1046/j.1365-2796.1998.00337.x. PMID 9681857. S2CID 20823909.
External links
| Classification | D |
|---|---|
| External resources |
| Tumours of the nervous system | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Endocrine |
| ||||||||||||||||||||||
| CNS |
| ||||||||||||||||||||||
| PNS: | |||||||||||||||||||||||
| Other | |||||||||||||||||||||||
| Note: Not all brain tumors are of nervous tissue, and not all nervous tissue tumors are in the brain (see brain metastasis). | |||||||||||||||||||||||