| Revision as of 15:03, 17 January 2015 editJonesey95 (talk | contribs)Autopatrolled, Extended confirmed users, Page movers, Mass message senders, Template editors370,268 editsm Fixing deprecated month parameter using AutoEd← Previous edit | Revision as of 21:24, 21 February 2015 edit undoBfpage (talk | contribs)Autopatrolled, Extended confirmed users, Pending changes reviewers, Rollbackers19,587 edits →Complications: edited for brevity:added templatesNext edit → | ||
| (29 intermediate revisions by 2 users not shown) | |||
| Line 45: | Line 45: | ||
| ==Complications== | ==Complications== | ||
| PID can cause ] inside the ], which can later cause serious complications, including chronic pelvic pain, ], ] (the leading cause of pregnancy-related deaths in adult females), and other |
PID can cause ] inside the ], which can later cause serious complications, including chronic pelvic pain, ], ] (the leading cause of pregnancy-related deaths in adult females), and other complications of pregnancy. Occasionally, the infection can spread to in the ] causing inflammation and the formation of scar tissue on the external surface of the liver (]).{{cn}} | ||
| Fertility may be restored in women affected by PID |
Fertility may be restored in women affected by PID with ] surgery. In vitro fertilization (]) has been used to bypass tubal problems and has become the main treatment for patients who want to become pregnant.{{cn}} | ||
| ==Treatment== | ==Treatment== | ||
| Treatment depends on the infectious agent and generally involves the use of ] therapy. If there is no improvement within two to three days, the patient is typically advised to seek further medical attention. Hospitalization sometimes becomes necessary if there are other complications. Treating sexual partners for possible STIs can help in treatment and prevention.{{cn|date=February 2015}} | |||
| Treatment depends on the cause and generally involves use of ] therapy. If the patient has not improved within two to three days after beginning treatment with the antibiotics, they should return to the hospital for further treatment. Drugs should also be given orally and/or intravenously to the patient while in the hospital to begin treatment immediately, and to increase the effectiveness of antibiotic treatment. Hospitalization may be necessary if the patient has Tubo-ovarian abscesses; is very ill, immunodeficient, pregnant, or incompetent; or because a life-threatening condition cannot be ruled out. Treating partners for STIs is a very important part of treatment and prevention. Anyone with PID and partners of patients with PID since six months prior to diagnosis should be treated to prevent reinfection. Psychotherapy is highly recommended to women diagnosed with PID as the fear of redeveloping the disease after being cured may exist.{{Citation needed|date=February 2010}} It is important for a patient to communicate any issues and/or uncertainties they may have to a doctor, especially a specialist such as a gynecologist, and in doing so, to seek follow-up care. | |||
| The ] guidelines state that the site route of antibiotic administration affects the short or long-term major outcome of women with mild or moderate disease.<ref name="pmid17342664">{{cite journal |author=Walker CK, Wiesenfeld HC |title=Antibiotic therapy for acute pelvic inflammatory disease: the 2006 Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines |journal=Clin. Infect. Dis. |volume=44 |issue=Suppl 3 |pages=S111–22 |year=2007 |pmid=17342664 |doi=10.1086/511424}}</ref> | |||
| For women with PID of mild to moderate severity, parenteral and oral therapies appear to |
For women with PID of mild to moderate severity, parenteral and oral therapies appear to be efficacious.<ref>Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol 2002;186:929–37.</ref><ref>Ness RB, Hillier SL, Kip KE ea. Bacterial vaginosis and risk of pelvic inflammatory disease. Obstet Gynecol 2004;44 (Supp 3):S111–22.</ref><ref> Smith KJ, Ness RB, Wiesenfeld HC, et al. Cost-effectiveness of alternative outpatient pelvic inflammatory disease treatment strategies. Sex Transm Dis 2007;34:960–6. </ref> Clinical experience should guide decisions regarding transition to oral therapy, which usually can be initiated within 24–48 hours of clinical improvement.<ref>http://www.cdc.gov/std/treatment/2010/references.htm#a390</ref> Typical regimens include ] or ] plus ], and ] plus ].<ref>http://www.cdc.gov/std/treatment/2010/pid.htm#a2</ref> An alternative parenteral regimen is ]/] plus ].<ref>http://www.cdc.gov/std/treatment/2010/pid.htm#a2</ref> Another alternative is to use a parenteral regimen with ] or ] plus ].<ref>http://www.cdc.gov/std/treatment/2010/pid.htm#a2</ref> | ||
| ==Prevention== | ==Prevention== | ||
| The risk of contracting pelvic inflammatory disease can be reduced by the following: | |||
| ⚫ | * |
||
| ⚫ | * |
||
| ⚫ | * Using ] such as ]; see ] for other listings. | ||
| ⚫ | * |
||
| * Seeking medical attention if you are experiencing symptoms of PID. | |||
| * Discussing sexual history with a trusted physician in order to get properly screened for sexually transmitted diseases. | |||
| ⚫ | * Seeking medical attention after learning that a current or former sex partner has, or might have had a sexually transmitted infection. | ||
| * Regularly scheduling ]ing with a physician and discussing which tests will be performed that session. | |||
| ⚫ | * Scheduling regular ] (pelvic) exams with STI testing to screen for symptomless PID and to discuss sexual history.<ref name="pmid17888100">{{cite journal |author=Smith KJ, Cook RL, Roberts MS |title=Time from sexually transmitted infection acquisition to pelvic inflammatory disease development: influence on the cost-effectiveness of different screening intervals |journal=Value Health |volume=10 |issue=5 |pages=358–66 |year=2007 |pmid=17888100 |doi=10.1111/j.1524-4733.2007.00189.x}}</ref> | ||
| * Getting a STI history from your current partner and insisting they be tested and treated before intercourse. | * Getting a STI history from your current partner and insisting they be tested and treated before intercourse. | ||
| * Treating partners to prevent reinfection or spreading the infection to other people. | |||
| * Diligence in avoiding vaginal activity, particularly intercourse, after the end of a pregnancy (delivery, miscarriage, or abortion) or certain gynecological procedures, to ensure that the cervix closes. | * Diligence in avoiding vaginal activity, particularly intercourse, after the end of a pregnancy (delivery, miscarriage, or abortion) or certain gynecological procedures, to ensure that the cervix closes. | ||
| * Abstinence<ref> | |||
| {{cite web | |||
| | title = Prevention - STD Information from CDC | |||
| | publisher = Center For Disease Control | |||
| | url = http://www.cdc.gov/std/prevention/default.htm | |||
| | accessdate = 2015-02-21 | |||
| }} | |||
| </ref> | |||
| ==See also== | ==See also== | ||
| * ], any inflammation of the fallopian tubes | * ], any inflammation of the fallopian tubes | ||
| * ] an ] of the fallopian tube and ovary | |||
| * ] | * ] | ||
| * Pelvic ] | * Pelvic ] | ||
| * ] — withdrawn from the market in 1975 for PID risk | * ] — withdrawn from the market in 1975 for PID risk | ||
| * ] | * ] | ||
| * ] | |||
| * ] | |||
| ==References== | ==References== | ||
Revision as of 21:24, 21 February 2015
Medical condition| Pelvic inflammatory disease | |
|---|---|
| Specialty | Gynaecology |
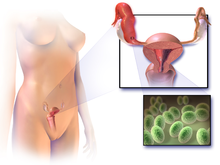
Pelvic inflammatory disease (or disorder) (PID) is a term for inflammation of the uterus, fallopian tubes, and/or ovaries as it progresses to scar formation with adhesions to nearby tissues and organs. This can lead to infertility. PID is a vague term and can refer to viral, fungal, parasitic, though most often bacterial infections. PID should be classified by affected organs, the stage of the infection, and the organism(s) causing it. Although a sexually transmitted infection (STI) is often the cause, many other routes are possible, including lymphatic, postpartum, postabortal (either miscarriage or abortion) or intrauterine device (IUD) related, and hematogenous spread.
Epidemiology
| The examples and perspective in this section may not represent a worldwide view of the subject. You may improve this section, discuss the issue on the talk page, or create a new section, as appropriate. (October 2010) (Learn how and when to remove this message) |
In the United States, more than 750,000 women are affected by PID each year, and the rate is highest with teenagers and first time mothers. PID causes over 100,000 women to become infertile in the US each year. N. gonorrhoea is isolated in 40–60% of women with acute salpingitis. C. trachomatis is estimated to be the cause in about 60% of cases of salpingitis, which may lead to PID. However, not all PID is caused solely by STIs; organisms that are considered normal vaginal flora can be involved, and individual cases of PID can be due to either a single organism or a co-infection of many different species. 10% of women in one study had asymptomatic Chlamydia trachomatis infection and 65% had asymptomatic infection with Neisseria gonorrhoeae. It was noted in one study that 10–40% of untreated women with N. gonorrhoea develop PID and 20–40% of women infected with C. trachomitis developed PID.
Diagnosis
Symptoms in PID range from subclinical (asymptomatic) to severe. If there are symptoms, then fever, cervical motion tenderness, lower abdominal pain, new or different discharge, painful intercourse, or irregular menstrual bleeding may be noted. Laparoscopic identification is helpful in diagnosing tubal disease, 65–90% positive predictive value in patients with presumed PID. Regular Sexually Transmitted Infection (STI) testing is important for prevention. Treatment is usually started empirically because of the serious complications that may result from delayed treatment. Definitive criteria include: histopathologic evidence of endometritis, thickened filled fallopian tubes, or laparoscopic findings. Gram-stain/smear becomes important in identification of rare and possibly more serious organisms. Two thirds of patients with laparoscopic evidence of previous PID were not aware they had PID, however even asymptomatic PID can cause serious harm.
About 96% of people with pelvic inflammatory disease have elevated C-reactive protein (CRP).
Upon gynecologic ultrasound, a potential finding is tubo-ovarian complex, which is edematous and dilated pelvic structures as evidenced by vague margins, but without abscess formation.
Differential diagnosis
Appendicitis, ectopic pregnancy, septic abortion, hemorrhagic or ruptured ovarian cysts or tumors, twisted ovarian cyst, degeneration of a myoma, and acute enteritis must be considered. Pelvic inflammatory disease is more likely to occur when there is a history of pelvic inflammatory disease, recent sexual contact, recent onset of menses, or an IUD (intrauterine device) in place or if the partner has a sexually transmitted infection.
Acute pelvic inflammatory disease is highly unlikely when recent intercourse has not taken place or an IUD is not being used. A sensitive serum pregnancy test should be obtained to rule out ectopic pregnancy. Culdocentesis will differentiate hemoperitoneum (ruptured ectopic pregnancy or hemorrhagic cyst) from pelvic sepsis (salpingitis, ruptured pelvic abscess, or ruptured appendix).
Pelvic and vaginal ultrasounds are helpful in the differential diagnosis of ectopic pregnancy of over six weeks. Laparoscopy is often utilized to diagnose pelvic inflammatory disease, and it is imperative if the diagnosis is not certain or if the patient has not responded to antibiotic therapy after 48 hours.
No single test has adequate sensitivity and specificity to diagnose pelvic inflammatory disease. A large multisite U.S. study found that cervical motion tenderness as a minimum clinical criterion increases the sensitivity of the CDC diagnostic criteria from 83% to 95%. However, even the modified 2002 CDC criteria do not identify women with subclinical disease.
Prognosis
Although the PID infection itself may be cured, effects of the infection may be permanent. This makes early identification by someone who can prescribe appropriate curative treatment very important in the prevention of damage to the reproductive system. Since early gonococcal infection may be asymptomatic, regular screening of individuals at risk for common agents (history of multiple partners, history of any unprotected sex, or people with symptoms) or because of certain procedures (post pelvic operation, postpartum, miscarriage or abortion). Prevention is also very important in maintaining viable reproduction capabilities.
If the initial infection is mostly in the lower tract, after treatment the person may have few difficulties. If the infection is in the fallopian tubes or ovaries, more serious complications are more likely to occur.
Complications
PID can cause scarring inside the reproductive organs, which can later cause serious complications, including chronic pelvic pain, infertility, ectopic pregnancy (the leading cause of pregnancy-related deaths in adult females), and other complications of pregnancy. Occasionally, the infection can spread to in the peritoneum causing inflammation and the formation of scar tissue on the external surface of the liver (Fitz-Hugh-Curtis syndrome).
Fertility may be restored in women affected by PID with tuboplastic surgery. In vitro fertilization (IVF) has been used to bypass tubal problems and has become the main treatment for patients who want to become pregnant.
Treatment
Treatment depends on the infectious agent and generally involves the use of antibiotic therapy. If there is no improvement within two to three days, the patient is typically advised to seek further medical attention. Hospitalization sometimes becomes necessary if there are other complications. Treating sexual partners for possible STIs can help in treatment and prevention.
The CDC guidelines state that the site route of antibiotic administration affects the short or long-term major outcome of women with mild or moderate disease.
For women with PID of mild to moderate severity, parenteral and oral therapies appear to be efficacious. Clinical experience should guide decisions regarding transition to oral therapy, which usually can be initiated within 24–48 hours of clinical improvement. Typical regimens include cefoxitin or cefotetan plus doxycycline, and clindamycin plus gentamicin. An alternative parenteral regimen is ampicillin/sulbactam plus doxycycline. Another alternative is to use a parenteral regimen with ceftriaxone or cefoxitin plus doxycycline.
Prevention
The risk of contracting pelvic inflammatory disease can be reduced by the following:
- Using barrier methods such as condoms; see human sexual behavior for other listings.
- Seeking medical attention if you are experiencing symptoms of PID.
- Seeking medical attention after learning that a current or former sex partner has, or might have had a sexually transmitted infection.
- Scheduling regular gynecological (pelvic) exams with STI testing to screen for symptomless PID and to discuss sexual history.
- Getting a STI history from your current partner and insisting they be tested and treated before intercourse.
- Diligence in avoiding vaginal activity, particularly intercourse, after the end of a pregnancy (delivery, miscarriage, or abortion) or certain gynecological procedures, to ensure that the cervix closes.
- Abstinence
See also
- Salpingitis, any inflammation of the fallopian tubes
- Endometritis
- Pelvic peritonitis
- Dalkon Shield — withdrawn from the market in 1975 for PID risk
- Bacterial Vaginosis
- Chlamydia infection
- Sexually transmitted infection
References
- "STD Facts — Pelvic inflammatory disease (PID)". Retrieved 2007-11-23.
- Sutton MY, Sternberg M, Zaidi A, St Louis ME, Markowitz LE (December 2005). "Trends in pelvic inflammatory disease hospital discharges and ambulatory visits, United States, 1985–2001". Sex Transm Dis. 32 (12): 778–84. doi:10.1097/01.olq.0000175375.60973.cb. PMID 16314776.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lauren Nathan; DeCherney, Alan H.; Pernoll, Martin L. (2003). Current obstetric & gynecologic diagnosis & treatment. New York: Lange Medical Books/McGraw-Hill. ISBN 0-8385-1401-4. OCLC 150148652.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Loscalzo, Joseph; Andreoli, Thomas E.; Cecil, Russell L.; Carpenter, Charles A.; Griggs, Robert C. (2001). Cecil essentials of medicine. Philadelphia: W.B. Saunders. ISBN 0-7216-8179-4. OCLC 43051599.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Reljic M, Gorisek B (February 1998). "C-reactive protein and the treatment of pelvic inflammatory disease". Int J Gynaecol Obstet. 60 (2): 143–50. PMID 9509952.
- Tuboovarian complex by Emily C. Wasco and Gillian Lieberman MD. Beth Israel Deaconess Medical Center. October 17, 2003
- Blenning CE, Muench J, Judkins DZ, Roberts KT (2007). "Clinical inquiries. Which tests are most useful for diagnosing PID?". J Fam Pract. 56 (3): 216–20. PMID 17343812.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Walker CK, Wiesenfeld HC (2007). "Antibiotic therapy for acute pelvic inflammatory disease: the 2006 Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines". Clin. Infect. Dis. 44 (Suppl 3): S111–22. doi:10.1086/511424. PMID 17342664.
- Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol 2002;186:929–37.
- Ness RB, Hillier SL, Kip KE ea. Bacterial vaginosis and risk of pelvic inflammatory disease. Obstet Gynecol 2004;44 (Supp 3):S111–22.
- Smith KJ, Ness RB, Wiesenfeld HC, et al. Cost-effectiveness of alternative outpatient pelvic inflammatory disease treatment strategies. Sex Transm Dis 2007;34:960–6.
- http://www.cdc.gov/std/treatment/2010/references.htm#a390
- http://www.cdc.gov/std/treatment/2010/pid.htm#a2
- http://www.cdc.gov/std/treatment/2010/pid.htm#a2
- http://www.cdc.gov/std/treatment/2010/pid.htm#a2
- Smith KJ, Cook RL, Roberts MS (2007). "Time from sexually transmitted infection acquisition to pelvic inflammatory disease development: influence on the cost-effectiveness of different screening intervals". Value Health. 10 (5): 358–66. doi:10.1111/j.1524-4733.2007.00189.x. PMID 17888100.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Prevention - STD Information from CDC". Center For Disease Control. Retrieved 2015-02-21.
Additional images
External links
| Female diseases of the pelvis and genitals | |||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Internal |
| ||||||||||||||||||||||||||||||||||||
| External |
| ||||||||||||||||||||||||||||||||||||
| Sexually transmitted infections (STI) | |
|---|---|
| Bacterial | |
| Protozoal | |
| Parasitic | |
| Viral | |
| General inflammation |
|
