| Revision as of 13:30, 15 November 2011 editBeetstra (talk | contribs)Edit filter managers, Administrators172,031 edits Script assisted update of identifiers for the Chem/Drugbox validation project (updated: 'ChEMBL').← Previous edit | Latest revision as of 18:13, 18 October 2024 edit undoCitation bot (talk | contribs)Bots5,418,679 edits Added bibcode. | Use this bot. Report bugs. | Suggested by Spinixster | Category:Chemicals using indexlabels | #UCB_Category 243/831 | ||
| (208 intermediate revisions by 96 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Antiretroviral medication}} | |||
| {{Citation style|article|date=September 2011}} | |||
| {{Use dmy dates|date=March 2024}} | |||
| {{Drugbox | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| {{Infobox drug | |||
| | Verifiedfields = changed | | Verifiedfields = changed | ||
| | verifiedrevid = |
| verifiedrevid = 460773860 | ||
| | image = File:Darunavir structure.svg | |||
| | IUPAC_name = oct-6-yl] ''N''--3-hydroxy-1-phenyl- butan-2-yl] carbamate | |||
| | |
| width = 200 | ||
| | alt = | |||
| | width = 180 | |||
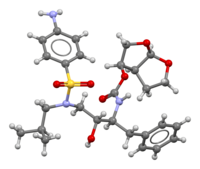
| | image2 = Darunavir-from-xtal-3D-bs-17.png | |||
| | width2 = | |||
| | alt2 = | |||
| | caption = | |||
| <!--Clinical data--> | <!-- Clinical data --> | ||
| | pronounce = | |||
| | tradename = Prezista | |||
| | tradename = Prezista, others<ref name=AHFS2016/> | |||
| | Drugs.com = {{drugs.com|monograph|darunavir}} | | Drugs.com = {{drugs.com|monograph|darunavir}} | ||
| | MedlinePlus = a607042 | | MedlinePlus = a607042 | ||
| | DailyMedID = Darunavir | |||
| | pregnancy_category = B | |||
| | |
| pregnancy_AU = B2 | ||
| | pregnancy_AU_comment = <ref name="Drugs.com pregnancy" /> | |||
| | routes_of_administration = oral | |||
| | pregnancy_category= | |||
| | routes_of_administration = ] | |||
| | class = ] | |||
| | ATC_prefix = J05 | |||
| | ATC_suffix = AE10 | |||
| | ATC_supplemental = | |||
| <!-- Legal status --> | |||
| | legal_AU = S4 | |||
| | legal_AU_comment = <ref>{{cite web | title=Prescription medicines: registration of new generic medicines and biosimilar medicines, 2017 | website=Therapeutic Goods Administration (TGA) | date=21 June 2022 | url=https://www.tga.gov.au/resources/publication/publications/prescription-medicines-registration-new-generic-medicines-and-biosimilar-medicines-2017 | access-date=30 March 2024 | archive-date=6 July 2023 | archive-url=https://web.archive.org/web/20230706023149/https://www.tga.gov.au/resources/publication/publications/prescription-medicines-registration-new-generic-medicines-and-biosimilar-medicines-2017 | url-status=live }}</ref> | |||
| | legal_BR = <!-- OTC, A1, A2, A3, B1, B2, C1, C2, C3, C4, C5, D1, D2, E, F--> | |||
| | legal_BR_comment = | |||
| | legal_CA = Rx-only | |||
| | legal_CA_comment = | |||
| | legal_DE = <!-- Anlage I, II, III or Unscheduled--> | |||
| | legal_DE_comment = | |||
| | legal_NZ = <!-- Class A, B, C --> | |||
| | legal_NZ_comment = | |||
| | legal_UK = POM | |||
| | legal_UK_comment = | |||
| | legal_US = Rx-only | |||
| | legal_US_comment = <ref name="Prezista FDA label" /> | |||
| | legal_EU = Rx-only | |||
| | legal_EU_comment = <ref name="Prezista EPAR" /> | |||
| | legal_UN = <!-- N I, II, III, IV / P I, II, III, IV--> | |||
| | legal_UN_comment = | |||
| | legal_status = Rx-only | |||
| <!--Pharmacokinetic data--> | <!-- Pharmacokinetic data --> | ||
| | bioavailability = | | bioavailability = 37% (without ]), 82% (with ]) | ||
| | protein_bound = 95% | | protein_bound = 95% | ||
| | metabolism = |
| metabolism = ] (]) | ||
| | metabolites = | |||
| | elimination_half-life = 15 hours | |||
| | onset = | |||
| | elimination_half-life = 15 hours (with ]) | |||
| | duration_of_action = | |||
| | excretion = Feces (80%), urine (14%) | |||
| <!--Identifiers--> | <!-- Identifiers --> | ||
| | index2_label = as salt | |||
| | CASNo_Ref = {{cascite|correct|CAS}} | |||
| | CAS_number_Ref = {{cascite|correct|??}} | | CAS_number_Ref = {{cascite|correct|??}} | ||
| | CAS_number = 206361-99-1 | | CAS_number = 206361-99-1 | ||
| | CAS_supplemental = | |||
| | ATC_prefix = J05 | |||
| | ATC_suffix = AE10 | |||
| | ATC_supplemental = | |||
| | PubChem = 213039 | | PubChem = 213039 | ||
| | IUPHAR_ligand = | |||
| | DrugBank_Ref = {{drugbankcite|changed|drugbank}} | |||
| | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| | DrugBank = DB01264 | | DrugBank = DB01264 | ||
| | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | ||
| Line 35: | Line 72: | ||
| | UNII_Ref = {{fdacite|correct|FDA}} | | UNII_Ref = {{fdacite|correct|FDA}} | ||
| | UNII = YO603Y8113 | | UNII = YO603Y8113 | ||
| | KEGG_Ref = {{keggcite| |
| KEGG_Ref = {{keggcite|correct|kegg}} | ||
| | KEGG = D03656 | | KEGG = D03656 | ||
| | |
| KEGG2_Ref = {{keggcite|correct|kegg}} | ||
| | KEGG2 = D06478 | |||
| | ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| | ChEBI = 367163 | | ChEBI = 367163 | ||
| | ChEMBL_Ref = {{ebicite|changed|EBI}} | | ChEMBL_Ref = {{ebicite|changed|EBI}} | ||
| | ChEMBL = |
| ChEMBL = 1323 | ||
| | NIAID_ChemDB = 073035 | |||
| | C=27 | H=37 | N=3 | O=7 | S=1 | |||
| | PDB_ligand = 017 | |||
| | molecular_weight = 547.665 g/mol | |||
| | synonyms = TMC114, DRV, darunavir ethanolate | |||
| | smiles = O=S(=O)(c1ccc(N)cc1)N(CC(C)C)C(O)(NC(=O)O2CO3OCC23)Cc4ccccc4 | |||
| | InChI = 1/C27H37N3O7S/c1-18(2)15-30(38(33,34)21-10-8-20(28)9-11-21)16-24(31)23(14-19-6-4-3-5-7-19)29-27(32)37-25-17-36-26-22(25)12-13-35-26/h3-11,18,22-26,31H,12-17,28H2,1-2H3,(H,29,32)/t22-,23-,24+,25-,26+/m0/s1 | |||
| <!-- Chemical and physical data --> | |||
| | InChIKey = CJBJHOAVZSMMDJ-HEXNFIEUBK | |||
| | IUPAC_name = oct-6-yl] ''N''--3-hydroxy-1-phenyl- butan-2-yl] carbamate | |||
| | C=27 | H=37 | N=3 | O=7 | S=1 | |||
| | SMILES = O=S(=O)(c1ccc(N)cc1)N(CC(C)C)C(O)(NC(=O)O2CO3OCC23)Cc4ccccc4 | |||
| | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChI = 1S/C27H37N3O7S/c1-18(2)15-30(38(33,34)21-10-8-20(28)9-11-21)16-24(31)23(14-19-6-4-3-5-7-19)29-27(32)37-25-17-36-26-22(25)12-13-35-26/h3-11,18,22-26,31H,12-17,28H2,1-2H3,(H,29,32)/t22-,23-,24+,25-,26+/m0/s1 | | StdInChI = 1S/C27H37N3O7S/c1-18(2)15-30(38(33,34)21-10-8-20(28)9-11-21)16-24(31)23(14-19-6-4-3-5-7-19)29-27(32)37-25-17-36-26-22(25)12-13-35-26/h3-11,18,22-26,31H,12-17,28H2,1-2H3,(H,29,32)/t22-,23-,24+,25-,26+/m0/s1 | ||
| | StdInChI_comment = | |||
| | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChIKey = CJBJHOAVZSMMDJ-HEXNFIEUSA-N | | StdInChIKey = CJBJHOAVZSMMDJ-HEXNFIEUSA-N | ||
| | density = | |||
| | density_notes = | |||
| | melting_point = | |||
| | melting_high = | |||
| | melting_notes = | |||
| | boiling_point = | |||
| | boiling_notes = | |||
| | solubility = | |||
| | sol_units = | |||
| | specific_rotation = | |||
| }} | }} | ||
| '''Darunavir''' (brand name '''Prezista''', formerly known as TMC114) is a ] used to treat ] infection. It is in the ] class. Prezista is an ] recommended treatment option for treatment-naïve and treatment-experienced adults and adolescents<ref name="oarac">Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents, November 3, 2008, Developed by the DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents – A Working Group of the Office of AIDS Research Advisory Council (OARAC). .</ref>. Developed by pharmaceutical company ], darunavir is named after Arun K. Ghosh, the chemist who discovered the molecule at the ]. It was approved by the ] (FDA) on June 23, 2006.<ref>Rodger D MacArthura, Darunavir: promising initial results, doi:10.1016/S0140-6736(07)60499-1</ref> | |||
| <!-- Definition and symptoms --> | |||
| Darunavir is a second-generation protease inhibitor (PIs), designed specifically to overcome problems with the older agents in this class, such as ]. Early PIs often have severe side effects and drug toxicities, require a high therapeutic dose, are costly to manufacture, and show a disturbing susceptibility to drug resistant mutations. Such mutations can develop in as little as a year of use, and effectively render the drugs useless. | |||
| '''Darunavir''' ('''DRV'''), sold under the brand name '''Prezista''' among others, is an ] used to treat and prevent ].<ref name=AHFS2016/> It is generally recommended for use with other antiretrovirals.<ref name=AHFS2016/><ref name="Prezista FDA label">{{cite web | title=Prezista- darunavir tablet, film coated Prezista- darunavir suspension | website=DailyMed | date=6 June 2019 | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=814301f9-c990-46a5-b481-2879a521a16f | access-date=21 April 2020 | archive-date=6 February 2019 | archive-url=https://web.archive.org/web/20190206184548/https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=814301f9-c990-46a5-b481-2879a521a16f | url-status=live }}</ref> It is often used with low doses of ] or ] to increase darunavir levels.<ref name=AHFS2016/> It may be used for prevention after a ] or other potential exposure.<ref name=AHFS2016/> It is taken ] once to twice a day.<ref name=AHFS2016>{{cite web|title=Darunavir|url=https://www.drugs.com/monograph/darunavir.html|publisher=The American Society of Health-System Pharmacists|access-date=28 November 2016|url-status=live|archive-url=https://web.archive.org/web/20161110112612/https://www.drugs.com/monograph/darunavir.html|archive-date=10 November 2016}}</ref> | |||
| <!-- Side effects and mechanism --> | |||
| Darunavir was designed to form robust interactions with the ] enzyme from many strains of HIV, including strains from treatment-experienced patients with multiple resistance mutations to PIs.<ref name="pmid17900913">{{cite journal | |||
| Common side effects include ], ], ], ], ] and ].<ref name=AHFS2016/><ref name="Prezista FDA label" /> Severe side effects include ], ], and skin rashes such as ].<ref name=AHFS2016/> While poorly studied in ] it appears to be safe for the baby.<ref name="Drugs.com pregnancy">{{cite web | title=Darunavir (Prezista) Use During Pregnancy | website=Drugs.com | date=23 October 2018 | url=https://www.drugs.com/pregnancy/darunavir.html | access-date=21 April 2020 | archive-date=20 December 2016 | archive-url=https://web.archive.org/web/20161220115210/https://www.drugs.com/pregnancy/darunavir.html | url-status=live }}</ref> It is of the ] (PI) class and works by blocking ].<ref name=AHFS2016/> | |||
| | author = Ghosh AK, Dawson ZL, Mitsuya H | |||
| | title = Darunavir, a conceptually new HIV-1 protease inhibitor for the treatment of drug-resistant HIV | |||
| | journal = Bioorg. Med. Chem. | |||
| | volume = 15 | |||
| | issue = 24 | |||
| | pages = 7576–80 | |||
| | year = 2007 | |||
| | pmid = 17900913 | |||
| | doi = 10.1016/j.bmc.2007.09.010 | |||
| | url = http://linkinghub.elsevier.com/retrieve/pii/S0968-0896(07)00783-3 | |||
| | accessdate = 2007-12-22 | |||
| | pmc = 2112938 | |||
| }}</ref><ref>''Darunavir-ritonavir more effective than Lopinavir-ritonavir in HIV infected, treatment-experienced patients'', The Lancet, '''2007''', 370, </ref> | |||
| <!-- History and culture --> | |||
| Darunavir received much attention at the time of its release, as it represents an important treatment option for patients with drug-resistant HIV. Patient advocacy groups pressured developer Tibotec not to follow the previous trend of releasing new drugs at prices higher than existing drugs in the same class. Darunavir was priced to match other common PIs already in use, such as the ] drug ]. The drug costs around $9,000 for a one year supply.<ref>Liz Highleyman, Patient Advocates Commend Pricing of New PI Darunavir, </ref><ref>Darunavir - first molecule to treat drug-resistant HIV, </ref><ref>Retaining Efficacy Against Evasive HIV, </ref> | |||
| Darunavir was approved by the US ] (FDA) in June 2006.<ref name="Drug Approval Package: Prezista">{{cite web | title=Drug Approval Package: Prezista (Darumavir) NDA #021976 | website=U.S. ] (FDA) | url=https://www.accessdata.fda.gov/drugsatfda_docs/nda/2006/021976s000_SprycelTOC.cfm | access-date=26 May 2024 | archive-date=1 July 2016 | archive-url=https://web.archive.org/web/20160701210501/http://www.accessdata.fda.gov/drugsatfda_docs/nda/2006/021976s000_SprycelTOC.cfm | url-status=live }}</ref><ref>{{cite journal | vauthors = MacArthur RD | title = Darunavir: promising initial results | journal = Lancet | volume = 369 | issue = 9568 | pages = 1143–1144 | date = April 2007 | pmid = 17416241 | doi = 10.1016/S0140-6736(07)60499-1 | s2cid = 31175809 }}</ref> It is on the ].<ref name="WHO21st">{{cite book | vauthors = ((World Health Organization)) | title = World Health Organization model list of essential medicines: 21st list 2019 | year = 2019 | hdl = 10665/325771 | author-link = World Health Organization | publisher = World Health Organization | location = Geneva | id = WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO | hdl-access=free }}</ref> It is available as a ].<ref>{{cite web | title=2022 First Generic Drug Approvals | website=U.S. ] (FDA) | date=3 March 2023 | url=https://www.fda.gov/drugs/drug-and-biologic-approval-and-ind-activity-reports/2022-first-generic-drug-approvals | archive-url=https://web.archive.org/web/20230630003602/https://www.fda.gov/drugs/drug-and-biologic-approval-and-ind-activity-reports/2022-first-generic-drug-approvals | archive-date=30 June 2023 | url-status=live | access-date=30 June 2023}}</ref> | |||
| It is available in the ] medication ] (Prezcobix, Rezolsta),<ref>{{cite web | title=Prezcobix - darunavir ethanolate and cobicistat tablet, film coated | website=DailyMed | date=2 January 2024 | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=16ca460a-3c89-4697-8f45-972615a2a518 | access-date=26 May 2024 | archive-date=28 November 2023 | archive-url=https://web.archive.org/web/20231128095338/https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=16ca460a-3c89-4697-8f45-972615a2a518 | url-status=live }}</ref><ref>{{cite web | title=Darunavir / Cobicistat | website=Clinicalinfo | date=27 November 2023 | url=https://clinicalinfo.hiv.gov/en/drugs/darunavir-cobicistat/patient | access-date=26 May 2024 | archive-date=25 February 2024 | archive-url=https://web.archive.org/web/20240225050339/https://clinicalinfo.hiv.gov/en/drugs/darunavir-cobicistat/patient | url-status=live }}</ref> and in the fixed-dose combination medication ] (Symtuza).<ref>{{cite web | title=Symtuza - darunavir, cobicistat, emtricitabine, and tenofovir alafenamide tablet, film coated | website=DailyMed | date=18 August 2023 | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=85a17d00-6b7c-41ea-a6b3-5ad924820dab#section-10 | access-date=26 May 2024 | archive-date=9 July 2021 | archive-url=https://web.archive.org/web/20210709182242/https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=85a17d00-6b7c-41ea-a6b3-5ad924820dab#section-10 | url-status=live }}</ref><ref>{{cite web | title=Darunavir / Cobicistat / Emtricitabine / Tenofovir Alafenamide | website=Clinicalinfo | date=20 June 2023 | url=https://clinicalinfo.hiv.gov/en/drugs/darunavir-cobicistat-emtricitabine-tenofovir-alafenamide/patient | access-date=26 May 2024 | archive-date=23 January 2024 | archive-url=https://web.archive.org/web/20240123223300/https://clinicalinfo.hiv.gov/en/drugs/darunavir-cobicistat-emtricitabine-tenofovir-alafenamide/patient | url-status=live }}</ref> | |||
| ==Efficacy== | |||
| ==Medical uses== | |||
| Prezista is an ] (DHHS) recommended treatment option for treatment-naïve and treatment-experienced adults and adolescents<ref name="oarac" />. | |||
| Darunavir is ] for the treatment of human immunodeficiency virus (HIV-1) infection in adults and children three years of age and older when co-administered with ritonavir, in combination with other antiretroviral agents.<ref name="Prezista FDA label" /><ref name="Prezista EPAR">{{cite web | title=Prezista EPAR | website=] (EMA) | url=https://www.ema.europa.eu/en/medicines/human/EPAR/prezista | access-date=21 April 2020 | archive-date=25 June 2019 | archive-url=https://web.archive.org/web/20190625095402/https://www.ema.europa.eu/en/medicines/human/EPAR/prezista | url-status=live }} Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.</ref> | |||
| Darunavir is an ] (DHHS) recommended treatment option for adults and adolescents, regardless of whether they have received HIV treatment in the past.<ref>{{cite web | title=What's New: Adult and Adolescent ARV Guidelines | website=Clinicalinfo | date=27 February 2024 | url=https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv/whats-new | access-date=26 May 2024 | archive-date=26 November 2023 | archive-url=https://web.archive.org/web/20231126215220/https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv/whats-new | url-status=live }}</ref><ref name="AIDSinfo 2018">{{cite web | title=What's New in the Guidelines? Adult and Adolescent ARV | website=AIDSinfo | date=26 June 2018 | url=https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv/37/whats-new-in-the-guidelines- | archive-url=https://web.archive.org/web/20200914185419/https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv/37/whats-new-in-the-guidelines- | archive-date=14 September 2020 | url-status=dead | access-date=22 April 2023}}</ref> In a study of people that had never received HIV treatment, darunavir was as effective as ]/] at 96 weeks with a once-daily dosing.<ref>{{cite journal | vauthors = Antinori A, Lazzarin A, Uglietti A, Palma M, Mancusi D, Termini R | title = Efficacy and safety of boosted darunavir-based antiretroviral therapy in HIV-1-positive patients: results from a meta-analysis of clinical trials | journal = Scientific Reports | volume = 8 | issue = 1 | pages = 5288 | date = March 2018 | pmid = 29588457 | pmc = 5869729 | doi = 10.1038/s41598-018-23375-6 | bibcode = 2018NatSR...8.5288A }}</ref> It was approved by the FDA in October 2008, for people not previously treated for HIV.<ref>{{cite web | title=U.S. Food and Drug Administration (FDA) Approves Prezista Once-Daily as Part of Combination Therapy for Treatment-Naive Adults with HIV-1 | website=Drugs.com | date=22 October 2008 | url=https://www.drugs.com/newdrugs/u-s-food-administration-fda-approves-prezista-once-daily-part-combination-therapy-naive-adults-hiv-1-1159.html | access-date=26 May 2024 | archive-date=23 September 2013 | archive-url=https://web.archive.org/web/20130923024546/http://www.drugs.com/newdrugs/u-s-food-administration-fda-approves-prezista-once-daily-part-combination-therapy-naive-adults-hiv-1-1159.html | url-status=live }}</ref> Darunavir does not cure HIV/AIDS.<ref name="Prezista FDA label" /> | |||
| Darunavir showed comparable efficacy to lopinavir/ritonavir at 96 weeks with a once-daily dosing in treatment-naïve patients<ref>, Efficacy and Safety of Boosted Darunavir (Prezista) Are Superior to Lopinavir/ritonavir (Kaletra) at 96 Weeks: ARTEMIS Trial, 2008-10-28, .</ref>. It was approved by the ] for '''treatment-naive patients''' on October the 21st 2008.<ref>, Darunavir (Prezista) Receives Full Traditional Approval, Dose Set for Treatment-naive Patients, Caution Urged for Pregnant Women, 2008-10-24, .</ref> | |||
| == Adverse effects == | |||
| Darunavir showed superiority to ] and other ] in the POWER trials. The POWER 1 and POWER 2 were designed for '''treatment-experienced patients''', together with supportive data from the POWER 3 analysis. <ref>Bonaventura Clotet, Nicholas Bellos, Jean-Michel Molina, David Cooper, Jean-Christophe Goffard, Adriano Lazzarin, Andrej Wöhrmann, Christine Katlama, Timothy Wilkin, Richard Haubrich, et al., Efficacy and safety of darunavir-ritonavir at week 48 in treatment-experienced patients with HIV-1 infection in POWER 1 and 2: a pooled subgroup analysis of data from two randomised trials, The Lancet, Volume 369, Issue 9568, 7 April 2007-13 April 2007, Pages 1169-1178.</ref> The patients eligible for these studies had experience with at least one protease inhibitor, one non-nucleoside reverse transcriptase inhibitor (]) and two nucleoside reverse transcriptase inhibitors (]), and had one or more primary protease inhibitor mutations. | |||
| Darunavir is generally well tolerated by people. Rash is the most common side effect (7% of patients).<ref name="Prezista FDA label" /> Other common side effects are diarrhea (2.3%), headache (3.8%), abdominal pain (2.3%), constipation (2.3%), and vomiting (1.5%).<ref name="Prezista FDA label" /> Darunavir can also cause allergic reactions, and people allergic to ritonavir can also have a reaction to darunavir.<ref name="Prezista FDA label" /> | |||
| ], ] or worsening of diabetes, ], tenderness or weakness, and increased bleeding in people with ] have been reported in patients taking protease inhibitor medicines like darunavir.<ref name="Prezista FDA label" /> Changes in body fat have been seen in some patients taking medicines for HIV, including loss of fat from legs, arms and face, increased fat in the abdomen and other internal organs, breast enlargement, and fatty lumps on the back of the neck. The cause and long-term health effects of these conditions are not known.<ref name="Prezista FDA label" /> | |||
| Darunavir also showed superior results to ] in the TITAN trials (pre-planned, secondary endpoint, week 48), which was designed for patients with '''less advanced ] disease''' compared to the POWER trials.<ref>José Valdez Madruga, Daniel Berger, Marilyn McMurchie, Fredy Suter, Denes Banhegyi, Kiat Ruxrungtham, Dorece Norris, Eric Lefebvre, Marie-Pierre de Béthune, Frank Tomaka, et al., Efficacy and safety of darunavir-ritonavir compared with that of lopinavir-ritonavir at 48 weeks in treatment-experienced, HIV-infected patients in TITAN: a randomised controlled phase III trial, Pages 49-58. DOI 10.1016/S0140-6736(07)61049-6</ref> | |||
| === |
=== Drug interactions === | ||
| Darunavir may interact with medications commonly taken by people with ] such as other antiretrovirals, and antacids such as ] and ].<ref name="Prezista FDA label" /> ] may reduce the effectiveness of darunavir by increasing the breakdown of darunavir by the metabolic enzyme '']''.<ref name="Prezista FDA label" /> | |||
| ARTEMIS includes 689 treatment-naive participants with a baseline viral load of at least 5000 copies/mL who were randomly assigned to receive 800/100 mg once-daily darunavir/ritonavir or 800/200 mg lopinavir/ritonavir given once- or twice-daily. | |||
| At 96 weeks, darunavir/ritonavir remained non-inferior to lopinavir/ritonavir. | |||
| ==Mechanism of action== | |||
| * In an intent-to-treat analysis, significantly more patients in the darunavir/ritonavir arm achieved HIV RNA below 50 copies/mL compared with the lopinavir/ritonavir arm (79% vs. 71%; p = 0.012). | |||
| Darunavir is a nonpeptidic inhibitor of protease (PR) that lodges itself in the active site of PR through a number of hydrogen bonds.<ref name="Leonis, G. 2012">{{cite journal | vauthors = Leonis G, Czyżnikowska Ż, Megariotis G, Reis H, Papadopoulos MG | title = Computational studies of darunavir into HIV-1 protease and DMPC bilayer: necessary conditions for effective binding and the role of the flaps | journal = Journal of Chemical Information and Modeling | volume = 52 | issue = 6 | pages = 1542–1558 | date = June 2012 | pmid = 22587384 | doi = 10.1021/ci300014z }}</ref> It was developed to increase interactions with HIV-1 protease and to be more resistant against HIV-1 protease mutations. With a K<sub>d</sub> (]) of 4.5 x 10<sup>−12</sup> M, darunavir has a much stronger interaction with PR and its dissociation constant is 1/100 to 1/1000 of other protease inhibitors.<ref name="King, N. M. 2004">{{cite journal | vauthors = King NM, Prabu-Jeyabalan M, Nalivaika EA, Wigerinck P, de Béthune MP, Schiffer CA | title = Structural and thermodynamic basis for the binding of TMC114, a next-generation human immunodeficiency virus type 1 protease inhibitor | journal = Journal of Virology | volume = 78 | issue = 21 | pages = 12012–12021 | date = November 2004 | pmid = 15479840 | pmc = 523255 | doi = 10.1128/JVI.78.21.12012-12021.2004 | s2cid = 828919 | doi-access = free }}</ref> This strong interaction comes from increased hydrogen bonds between darunavir and the backbone of the PR active site (Figure 2). Darunavir's structure allows it to create more hydrogen bonds with the PR active site than most PIs that have been developed and approved by the FDA.<ref name="ReferenceB">{{cite journal | vauthors = Lefebvre E, Schiffer CA | title = Resilience to resistance of HIV-1 protease inhibitors: profile of darunavir | journal = AIDS Reviews | volume = 10 | issue = 3 | pages = 131–142 | year = 2008 | pmid = 18820715 | pmc = 2699666 }}</ref> Furthermore, the backbone of HIV-1 protease maintains its spatial conformation in the presence of mutations.<ref>{{cite journal | vauthors = Lascar RM, Benn P | title = Role of darunavir in the management of HIV infection | journal = HIV/AIDS: Research and Palliative Care| volume = 1 | pages = 31–39 | year = 2009 | pmid = 22096377 | pmc = 3218677 | doi = 10.2147/hiv.s5397 | doi-access = free }}</ref> Because darunavir interacts with this stable portion of the protease, the PR-PI interaction is less likely to be disrupted by a mutation.<ref name="ReferenceB"/> | |||
| * Response rates in the darunavir/ritonavir arm were statistically superior to those in the lopinavir/ritonavir arm for patients with high baseline viral load and low baseline CD4 count. | |||
| ** Among patients with baseline viral load below 100,000 copies/mL, 76% of patients in the darunavir/ritonavir arm and 63% in the lopinavir/ritonavir arm achieved HIV RNA below 50 copies/mL (p = 0.023). | |||
| * Once-daily darunavir/ritonavir was generally safe and well tolerated. | |||
| * Fewer patients in the darunavir/ritonavir arm discontinued treatment due to adverse events (4% vs. 9%). | |||
| * Patients taking darunavir/ritonavir were less likely to have moderate to severe (grade 2-4) treatment-related diarrhea (4% vs. 11%; p < 0.001). | |||
| * Grade 2-4 treatment-related rash occurred infrequently in both arms (3% with darunavir/ritonavir vs. 1% with lopinavir/ritonavir; p = 0.273). | |||
| * Patients taking darunavir/ritonavir had smaller average increases in triglycerides (0.1 vs. 0.8 mmol/L, or 12% vs. 50%) and total cholesterol (0.6 vs. 0.9 mmol/L, or 15% vs. 23%) (both p < 0.0001). | |||
| ] | |||
| ===TITAN trial=== | |||
| Analysis of 595 treatment-experienced patients being ]/]-naïve, HIV-1 infected adults with a viral load of greater than 1000 HIV-1 ] copies/mL. | |||
| Pre-planned secondary endpoint findings include: | |||
| * 71 percent of patients in the darunavir/r arm reached an undetectable viral load (less than 50 copies/mL) vs. 60 percent of patients in the lopinavir/r arm, a statistically significant difference (] = 0.005) | |||
| * 77 percent of patients in the darunavir/r arm achieved at least a 1 log10 reduction in HIV RNA vs. 69 percent in the lopinavir/r arm, a statistically significant difference (p = 0.028) | |||
| * The median increase from baseline in CD4 cell count was similar between the darunavir/r and lopinavir/r arms (88 cells per cubic millimeter vs. 81 cells per cubic millimeter) | |||
| ===Catalytic site=== | |||
| Development of resistance also was studied. Findings include: | |||
| * 10 percent of patients in the darunavir/r arm experienced virological failure vs. 22 percent of patients in the lopinavir/r arm | |||
| * Among patients experiencing virologic failure who had baseline and endpoint genotype data, 21 percent of patients in the darunavir/r arm developed primary PI resistance mutations vs. 36 percent of patients in the lopinavir/r arm, and 14 percent of patients in the darunavir/r arm developed primary NRTI resistance mutations vs. 27 percent of patients in the lopinavir/r arm | |||
| The chemical activity of the HIV-1 protease depends on two residues in the active site, Asp25 and Asp25', one from each copy of the homodimer.<ref name="Zhang, Y. 2014">{{cite journal | vauthors = Li D, Zhang Y, Zhao RN, Fan S, Han JG | title = Investigation on the mechanism for the binding and drug resistance of wild type and mutations of G86 residue in HIV-1 protease complexed with Darunavir by molecular dynamic simulation and free energy calculation | journal = Journal of Molecular Modeling | volume = 20 | issue = 2 | pages = 2122 | date = February 2014 | pmid = 24526384 | doi = 10.1007/s00894-014-2122-y | s2cid = 23262721 }}</ref> Darunavir interacts with these catalytic aspartates and the backbone of the active site through hydrogen bonds, specifically binding to residues Asp25, Asp25', Asp 29, Asp 30, Asp 30', and Gly 27 (Figure 3). This interaction prevents viral replication, as it competitively inhibits the viral polypeptides from gaining access to the active site and strongly binds to the enzymatic portions of this protein.<ref name="Leonis, G. 2012"/> | |||
| ===POWER 1 and POWER 2 trials=== | |||
| A pooled analysis of results from POWER 1 and POWER 2 demonstrated that after 24 weeks: | |||
| * Significantly more treatment-experienced patients achieved a reduction in viral load at the 24-week primary endpoint with darunavir, compared with the investigator-selected PI (70% vs. 21%, respectively). | |||
| * Almost four times as many treatment-experienced patients (45%) have achieved an undetectable viral load with the darunavir containing regimen, compared with the investigator-selected PI arm (12%). | |||
| * In treatment-experienced patients, the darunavir containing regimen increases CD4 cell counts five times more than the investigator-selected PI arm (92 cells/mm<sup>3</sup> vs. 17 cells/mm<sup>3</sup>, respectively) (Johnson & Johnson Press Release, 2006; Lazzarin, 2005) | |||
| ==History== | |||
| The efficacy results of POWER 1 and POWER 2 are confirmed by data from a large, non-randomized, open-label analysis known as POWER 3. | |||
| ] | |||
| After 24 weeks: | |||
| * 65 percent of patients achieved a reduction in viral load of 1 log10 or more, versus baseline. | |||
| * 40 percent of patients reached undetectable virus levels (less than 50 HIV RNA copies/mL). (Molina, 2005) | |||
| Darunavir was approved for use in the United States in June 2006 and for use in the European Union in February 2007.<ref>{{cite journal | vauthors = MacArthur RD | title = Darunavir: promising initial results | journal = Lancet | volume = 369 | issue = 9568 | pages = 1143–1144 | date = April 2007 | pmid = 17416241 | doi = 10.1016/S0140-6736(07)60499-1 | s2cid = 31175809 }}</ref><ref>{{cite press release|url=https://www.fda.gov/newsEvents/Newsroom/PressAnnouncements/2006/ucm108676.htm|title=FDA Approves New HIV Treatment for Patients Who Do Not Respond to Existing Drugs |website=U.S. ] (FDA) |access-date=10 November 2016|url-status=dead|archive-url=https://web.archive.org/web/20161113210634/https://www.fda.gov/newsEvents/Newsroom/PressAnnouncements/2006/ucm108676.htm|archive-date=13 November 2016}}</ref><ref name="FDA 2011"/><ref name="FDA approval">{{cite web | title=Drug Approval Package: Prezista (Darumavir) NDA #021976 | website=U.S. ] (FDA) | date=6 September 2006 | url=https://www.accessdata.fda.gov/drugsatfda_docs/nda/2006/021976s000_SprycelTOC.cfm | access-date=21 April 2020 | archive-date=1 July 2016 | archive-url=https://web.archive.org/web/20160701210501/http://www.accessdata.fda.gov/drugsatfda_docs/nda/2006/021976s000_SprycelTOC.cfm | url-status=live }}</ref><ref name="Prezista EPAR" />{{citation overkill|date=November 2022}} | |||
| ==Pharmacoeconomic considerations== | |||
| In the US and UK, healthcare costs were estimated to be lower with boosted darunavir than with investigator-selected control protease inhibitors in treatment-experienced patients.<ref name="darunavir">McKeage K, Perry CM, Keam SJ.. Drugs 2009;69(4):477-503.doi: 10.2165/00003495-200969040-00007.</ref> | |||
| The development of first-generation clinical inhibitors was founded on creating more protease-ligand interactions through hydrogen bonding and hydrophobic interactions.<ref name="Leonis, G. 2012"/> The first HIV protease inhibitor approved by the FDA was saquinavir, which was designed to target wild-type HIV-1 protease.<ref>{{cite journal | vauthors = Liu F, Kovalevsky AY, Tie Y, Ghosh AK, Harrison RW, Weber IT | title = Effect of flap mutations on structure of HIV-1 protease and inhibition by saquinavir and darunavir | journal = Journal of Molecular Biology | volume = 381 | issue = 1 | pages = 102–115 | date = August 2008 | pmid = 18597780 | pmc = 2754059 | doi = 10.1016/j.jmb.2008.05.062 }}</ref> However, this inhibitor is no longer effective due to resistance-causing mutations on the HIV-1 protease structure. The HIV genome has high plasticity, so has been able to become resistant to multiple HIV-1 protease inhibitors.<ref>{{cite journal | vauthors = Eron JJ | title = HIV-1 protease inhibitors | journal = Clinical Infectious Diseases | volume = 30 | issue = Suppl 2 | pages = S160–S170 | date = June 2000 | pmid = 10860901 | doi = 10.1086/313853 | doi-access = free }}</ref> Since saquinavir, the FDA has approved several PIs, including darunavir.<ref name="FDA 2011">{{cite web | title=HIV/AIDS Historical Time Line 2000 - 2010 | website=U.S. ] (FDA) | date=5 January 2018 | url=https://www.fda.gov/patients/hiv-timeline-and-history-approvals/hivaids-historical-time-line-2000-2010 | archive-url=https://web.archive.org/web/20190701174234/https://www.fda.gov/patients/hiv-timeline-and-history-approvals/hivaids-historical-time-line-2000-2010 | archive-date= 1 July 2019 | url-status=dead | access-date=21 April 2020}}</ref> | |||
| == Safety == | |||
| {{Unreferenced section|date=July 2009}} | |||
| As other ], darunavir does not cure HIV infection or ], and does not prevent passing HIV to others. | |||
| == Society and culture == | |||
| In studies, darunavir was generally well tolerated. Mild to moderate rash was seen in 7% of patients. Some patients developed severe rash. In clinical studies, 0.3% of patients discontinued due to rash. The most common moderate to severe side effects associated with darunavir include diarrhea (2.3%), headache (3.8%), abdominal pain (2.3%), constipation (2.3%), and vomiting (1.5%). Four percent of patients discontinued treatment due to adverse events. People who are allergic to darunavir or any of its ingredients, or ritonavir (Norvir) should not take darunavir. | |||
| === Economics === | |||
| In the US and UK, healthcare costs were estimated to be lower with boosted darunavir than with investigator-selected control protease inhibitors in treatment-experienced patients.<ref name="darunavir">{{cite journal | vauthors = McKeage K, Perry CM, Keam SJ | title = Darunavir: a review of its use in the management of HIV infection in adults | journal = Drugs | volume = 69 | issue = 4 | pages = 477–503 | year = 2009 | pmid = 19323590 | doi = 10.2165/00003495-200969040-00007 | s2cid = 195690027 }}</ref> | |||
| {{clear}} | |||
| There were few relevant drug-drug interactions with other medications commonly used in HIV patient populations, such as other antiretroviral medications, proton pump inhibitors, and H2 receptor antagonists. ] may reduce its effectiveness by interaction with ]. Patients should talk to their healthcare provider about all the medicines they are taking or plan to take, including prescription and nonprescription medicines, vitamins, and herbal supplements. | |||
| == References == | |||
| Before taking darunavir, patients should tell their healthcare provider if they have any medical conditions, including diabetes, liver problems, hemophilia, or allergy to sulfa medicines and should tell their doctor if they are pregnant or planning to become pregnant, or are nursing. Darunavir should be used with caution in patients with hepatic impairment. | |||
| High blood sugar, diabetes or worsening of diabetes, muscle pain, tenderness or weakness, and increased bleeding in people with hemophilia have been reported in patients taking protease inhibitor medicines like darunavir. Changes in body fat have been seen in some patients taking anti-HIV medicines, including loss of fat from legs, arms and face, increased fat in the abdomen and other internal organs, breast enlargement and fatty lumps on the back of the neck. The cause and long-term health effects of these conditions are not known at this time. | |||
| Clinical laboratory safety observed in the darunavir group was comparable to the control group. (Product Monograph, Darunavir) | |||
| == Dosing and administration == | |||
| The recommended oral dose of darunavir tablets is 600 mg (two 300 mg tablets) twice daily (BID) taken with ritonavir 100 mg BID and with food. The drug can be taken with any type of food. | |||
| Additional Studies Involving Darunavir | |||
| * TMC114-C211: Investigating a dose of 800 mg of the drug boosted with 100 mg of ritonavir once daily in treatment-naïve patients. | |||
| * TMC114-C214: Investigating a dose of 600 mg of the drug boosted with 100 mg of ritonavir twice daily in moderately treatment-experienced patients. | |||
| * DUET trial: The drug is being studied with TMC125, an investigational non-nucleoside reverse transcriptase inhibitor, in one of the few HIV clinical trials to involve two investigational HIV treatments in treatment-experienced patients. (Tibotec 2006) | |||
| ==See also== | |||
| * ] | |||
| ==Notes== | |||
| {{Reflist}} | {{Reflist}} | ||
| {{Antiretroviral drug}} | |||
| == References == | |||
| {{Portal bar | Medicine | Viruses }} | |||
| {{More footnotes|date=October 2009}} | |||
| {{Authority control}} | |||
| * Lazzarin A, Queiroz-Telles F, Frank I, Rockstroh J, Walmsley S, De Paepe E, Vangeneugden T, Spinosa-Guzman S and Lefebvre E Lazzarin A, et al. XVI IAC 2006. | |||
| * Johnson & Johnson FDA Approval Press Release, June 23 2006, http://www.jnj.com/news/jnj_news/20060623_191250.htm;jsessionid=NT1BC4RC4RHKYCQPCAOWU3YKB2IIWTT | |||
| * Molina JM, Cohen C, Katlama C et al. TMC114/r in treatment-experienced HIV patients in power 3: 24-week efficacy and safety analysis. Poster abstract TUPE0060. | |||
| * Janssen-Ortho, Darunavir Mongraph information. Updated 2006. http://www.janssen-ortho.com/JOI/pdf_files/Darunavir_E.pdf | |||
| * TMC114, Tibotec, http://www.tibotec.com/bgdisplay.jhtml?itemname=HIV_tmc114 | |||
| * Ghosh, A. K., et al. Bioorg. Med. Chem. Lett. 1998, 8, 687-90; | |||
| * Mitsuya, H. Ghosh, A. K., et al. J. Virology 2002, 76, 1349; | |||
| * Ghosh, A. K. Duzguiness, N., et al. Antiviral Res. 2002, 54, 29; | |||
| * Koh, Y., Ghosh, A. K., Mitsuya, H., et al. Antimicrobial Agents and Chemotherapy, 2003, 47, 3123 | |||
| * Ghosh, A. K., Mitsuya, H., et al. ChemMedChem 2006, 1, 937 | |||
| * A. K. Ghosh, B. D. Chapsal, I. T. Weber, H. Mitsuya. '' Acc. Chem. Res.'' 2007, ASAP. | |||
| * A. K. Ghosh, Z. L. Dawson, H. Mitsuya. '' Bioorg. Med. Chem.'' 2007, 15, 7576. | |||
| ] | |||
| ==External links== | |||
| ] | |||
| * ] at AIDSmeds.com | |||
| ] | |||
| * in ] | |||
| ], | |||
| * | |||
| ] | |||
| * | |||
| ] | |||
| ] | |||
| {{HIVpharm}} | |||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
Latest revision as of 18:13, 18 October 2024
Antiretroviral medicationPharmaceutical compound
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Prezista, others |
| Other names | TMC114, DRV, darunavir ethanolate |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a607042 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | HIV protease inhibitor |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 37% (without ritonavir), 82% (with ritonavir) |
| Protein binding | 95% |
| Metabolism | Liver (CYP3A4) |
| Elimination half-life | 15 hours (with ritonavir) |
| Excretion | Feces (80%), urine (14%) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.111.730 |
| Chemical and physical data | |
| Formula | C27H37N3O7S |
| Molar mass | 547.67 g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (what is this?) (verify) | |
Darunavir (DRV), sold under the brand name Prezista among others, is an antiretroviral medication used to treat and prevent HIV/AIDS. It is generally recommended for use with other antiretrovirals. It is often used with low doses of ritonavir or cobicistat to increase darunavir levels. It may be used for prevention after a needlestick injury or other potential exposure. It is taken by mouth once to twice a day.
Common side effects include diarrhea, nausea, abdominal pain, headache, rash and vomiting. Severe side effects include allergic reactions, liver problems, and skin rashes such as toxic epidermal necrolysis. While poorly studied in pregnancy it appears to be safe for the baby. It is of the protease inhibitor (PI) class and works by blocking HIV protease.
Darunavir was approved by the US Food and Drug Administration (FDA) in June 2006. It is on the World Health Organization's List of Essential Medicines. It is available as a generic medication.
It is available in the fixed-dose combination medication darunavir/cobicistat (Prezcobix, Rezolsta), and in the fixed-dose combination medication darunavir/cobicistat/emtricitabine/tenofovir alafenamide (Symtuza).
Medical uses
Darunavir is indicated for the treatment of human immunodeficiency virus (HIV-1) infection in adults and children three years of age and older when co-administered with ritonavir, in combination with other antiretroviral agents.
Darunavir is an Office of AIDS Research Advisory Council (DHHS) recommended treatment option for adults and adolescents, regardless of whether they have received HIV treatment in the past. In a study of people that had never received HIV treatment, darunavir was as effective as lopinavir/ritonavir at 96 weeks with a once-daily dosing. It was approved by the FDA in October 2008, for people not previously treated for HIV. Darunavir does not cure HIV/AIDS.
Adverse effects
Darunavir is generally well tolerated by people. Rash is the most common side effect (7% of patients). Other common side effects are diarrhea (2.3%), headache (3.8%), abdominal pain (2.3%), constipation (2.3%), and vomiting (1.5%). Darunavir can also cause allergic reactions, and people allergic to ritonavir can also have a reaction to darunavir.
High blood sugar, diabetes or worsening of diabetes, muscle pain, tenderness or weakness, and increased bleeding in people with hemophilia have been reported in patients taking protease inhibitor medicines like darunavir. Changes in body fat have been seen in some patients taking medicines for HIV, including loss of fat from legs, arms and face, increased fat in the abdomen and other internal organs, breast enlargement, and fatty lumps on the back of the neck. The cause and long-term health effects of these conditions are not known.
Drug interactions
Darunavir may interact with medications commonly taken by people with HIV/AIDS such as other antiretrovirals, and antacids such as proton pump inhibitors and H2 receptor antagonists. St. John's wort may reduce the effectiveness of darunavir by increasing the breakdown of darunavir by the metabolic enzyme CYP3A.
Mechanism of action
Darunavir is a nonpeptidic inhibitor of protease (PR) that lodges itself in the active site of PR through a number of hydrogen bonds. It was developed to increase interactions with HIV-1 protease and to be more resistant against HIV-1 protease mutations. With a Kd (dissociation constant) of 4.5 x 10 M, darunavir has a much stronger interaction with PR and its dissociation constant is 1/100 to 1/1000 of other protease inhibitors. This strong interaction comes from increased hydrogen bonds between darunavir and the backbone of the PR active site (Figure 2). Darunavir's structure allows it to create more hydrogen bonds with the PR active site than most PIs that have been developed and approved by the FDA. Furthermore, the backbone of HIV-1 protease maintains its spatial conformation in the presence of mutations. Because darunavir interacts with this stable portion of the protease, the PR-PI interaction is less likely to be disrupted by a mutation.

Catalytic site
The chemical activity of the HIV-1 protease depends on two residues in the active site, Asp25 and Asp25', one from each copy of the homodimer. Darunavir interacts with these catalytic aspartates and the backbone of the active site through hydrogen bonds, specifically binding to residues Asp25, Asp25', Asp 29, Asp 30, Asp 30', and Gly 27 (Figure 3). This interaction prevents viral replication, as it competitively inhibits the viral polypeptides from gaining access to the active site and strongly binds to the enzymatic portions of this protein.
History

Darunavir was approved for use in the United States in June 2006 and for use in the European Union in February 2007.
The development of first-generation clinical inhibitors was founded on creating more protease-ligand interactions through hydrogen bonding and hydrophobic interactions. The first HIV protease inhibitor approved by the FDA was saquinavir, which was designed to target wild-type HIV-1 protease. However, this inhibitor is no longer effective due to resistance-causing mutations on the HIV-1 protease structure. The HIV genome has high plasticity, so has been able to become resistant to multiple HIV-1 protease inhibitors. Since saquinavir, the FDA has approved several PIs, including darunavir.
Society and culture
Economics
In the US and UK, healthcare costs were estimated to be lower with boosted darunavir than with investigator-selected control protease inhibitors in treatment-experienced patients.
References
- ^ "Darunavir". The American Society of Health-System Pharmacists. Archived from the original on 10 November 2016. Retrieved 28 November 2016.
- ^ "Darunavir (Prezista) Use During Pregnancy". Drugs.com. 23 October 2018. Archived from the original on 20 December 2016. Retrieved 21 April 2020.
- "Prescription medicines: registration of new generic medicines and biosimilar medicines, 2017". Therapeutic Goods Administration (TGA). 21 June 2022. Archived from the original on 6 July 2023. Retrieved 30 March 2024.
- ^ "Prezista- darunavir tablet, film coated Prezista- darunavir suspension". DailyMed. 6 June 2019. Archived from the original on 6 February 2019. Retrieved 21 April 2020.
- ^ "Prezista EPAR". European Medicines Agency (EMA). Archived from the original on 25 June 2019. Retrieved 21 April 2020. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- "Drug Approval Package: Prezista (Darumavir) NDA #021976". U.S. Food and Drug Administration (FDA). Archived from the original on 1 July 2016. Retrieved 26 May 2024.
- MacArthur RD (April 2007). "Darunavir: promising initial results". Lancet. 369 (9568): 1143–1144. doi:10.1016/S0140-6736(07)60499-1. PMID 17416241. S2CID 31175809.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "2022 First Generic Drug Approvals". U.S. Food and Drug Administration (FDA). 3 March 2023. Archived from the original on 30 June 2023. Retrieved 30 June 2023.
- "Prezcobix - darunavir ethanolate and cobicistat tablet, film coated". DailyMed. 2 January 2024. Archived from the original on 28 November 2023. Retrieved 26 May 2024.
- "Darunavir / Cobicistat". Clinicalinfo. 27 November 2023. Archived from the original on 25 February 2024. Retrieved 26 May 2024.
- "Symtuza - darunavir, cobicistat, emtricitabine, and tenofovir alafenamide tablet, film coated". DailyMed. 18 August 2023. Archived from the original on 9 July 2021. Retrieved 26 May 2024.
- "Darunavir / Cobicistat / Emtricitabine / Tenofovir Alafenamide". Clinicalinfo. 20 June 2023. Archived from the original on 23 January 2024. Retrieved 26 May 2024.
- "What's New: Adult and Adolescent ARV Guidelines". Clinicalinfo. 27 February 2024. Archived from the original on 26 November 2023. Retrieved 26 May 2024.
- "What's New in the Guidelines? Adult and Adolescent ARV". AIDSinfo. 26 June 2018. Archived from the original on 14 September 2020. Retrieved 22 April 2023.
- Antinori A, Lazzarin A, Uglietti A, Palma M, Mancusi D, Termini R (March 2018). "Efficacy and safety of boosted darunavir-based antiretroviral therapy in HIV-1-positive patients: results from a meta-analysis of clinical trials". Scientific Reports. 8 (1): 5288. Bibcode:2018NatSR...8.5288A. doi:10.1038/s41598-018-23375-6. PMC 5869729. PMID 29588457.
- "U.S. Food and Drug Administration (FDA) Approves Prezista Once-Daily as Part of Combination Therapy for Treatment-Naive Adults with HIV-1". Drugs.com. 22 October 2008. Archived from the original on 23 September 2013. Retrieved 26 May 2024.
- ^ Leonis G, Czyżnikowska Ż, Megariotis G, Reis H, Papadopoulos MG (June 2012). "Computational studies of darunavir into HIV-1 protease and DMPC bilayer: necessary conditions for effective binding and the role of the flaps". Journal of Chemical Information and Modeling. 52 (6): 1542–1558. doi:10.1021/ci300014z. PMID 22587384.
- King NM, Prabu-Jeyabalan M, Nalivaika EA, Wigerinck P, de Béthune MP, Schiffer CA (November 2004). "Structural and thermodynamic basis for the binding of TMC114, a next-generation human immunodeficiency virus type 1 protease inhibitor". Journal of Virology. 78 (21): 12012–12021. doi:10.1128/JVI.78.21.12012-12021.2004. PMC 523255. PMID 15479840. S2CID 828919.
- ^ Lefebvre E, Schiffer CA (2008). "Resilience to resistance of HIV-1 protease inhibitors: profile of darunavir". AIDS Reviews. 10 (3): 131–142. PMC 2699666. PMID 18820715.
- Lascar RM, Benn P (2009). "Role of darunavir in the management of HIV infection". HIV/AIDS: Research and Palliative Care. 1: 31–39. doi:10.2147/hiv.s5397. PMC 3218677. PMID 22096377.
- Li D, Zhang Y, Zhao RN, Fan S, Han JG (February 2014). "Investigation on the mechanism for the binding and drug resistance of wild type and mutations of G86 residue in HIV-1 protease complexed with Darunavir by molecular dynamic simulation and free energy calculation". Journal of Molecular Modeling. 20 (2): 2122. doi:10.1007/s00894-014-2122-y. PMID 24526384. S2CID 23262721.
- MacArthur RD (April 2007). "Darunavir: promising initial results". Lancet. 369 (9568): 1143–1144. doi:10.1016/S0140-6736(07)60499-1. PMID 17416241. S2CID 31175809.
- "FDA Approves New HIV Treatment for Patients Who Do Not Respond to Existing Drugs". U.S. Food and Drug Administration (FDA) (Press release). Archived from the original on 13 November 2016. Retrieved 10 November 2016.
- ^ "HIV/AIDS Historical Time Line 2000 - 2010". U.S. Food and Drug Administration (FDA). 5 January 2018. Archived from the original on 1 July 2019. Retrieved 21 April 2020.
- "Drug Approval Package: Prezista (Darumavir) NDA #021976". U.S. Food and Drug Administration (FDA). 6 September 2006. Archived from the original on 1 July 2016. Retrieved 21 April 2020.
- Liu F, Kovalevsky AY, Tie Y, Ghosh AK, Harrison RW, Weber IT (August 2008). "Effect of flap mutations on structure of HIV-1 protease and inhibition by saquinavir and darunavir". Journal of Molecular Biology. 381 (1): 102–115. doi:10.1016/j.jmb.2008.05.062. PMC 2754059. PMID 18597780.
- Eron JJ (June 2000). "HIV-1 protease inhibitors". Clinical Infectious Diseases. 30 (Suppl 2): S160 – S170. doi:10.1086/313853. PMID 10860901.
- McKeage K, Perry CM, Keam SJ (2009). "Darunavir: a review of its use in the management of HIV infection in adults". Drugs. 69 (4): 477–503. doi:10.2165/00003495-200969040-00007. PMID 19323590. S2CID 195690027.
,
Categories: