| Revision as of 10:38, 17 May 2006 edit217.150.114.18 (talk)No edit summary← Previous edit | Latest revision as of 08:50, 21 December 2024 edit undoWhywhenwhohow (talk | contribs)Autopatrolled, Extended confirmed users, Pending changes reviewers49,018 edits rank | ||
| (827 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Antibiotic medication}} | |||
| {{drugbox | | |||
| {{Redirect|Eryc|the local authority of the East Riding of Yorkshire|East Riding of Yorkshire Council}} | |||
| |image=Erythromycin.png | |||
| {{Distinguish|Azithromycin}} | |||
| |IUPAC_name = <small>6-(4-dimethylamino-3-hydroxy-6-methyl-oxan-2-yl)oxy-14-ethyl-7,12,13-trihydroxy- | |||
| {{Use dmy dates|date=September 2024}} | |||
| 4-(5-hydroxy-4-methoxy-4,6-dimethyl-oxan-2-yl)oxy-3,5,7,9,11,13-hexamethyl- | |||
| {{cs1 config |name-list-style=vanc |display-authors=6}} | |||
| 1-oxacyclotetradecane-2,10-dione</small> | |||
| {{Infobox drug | |||
| |CAS_number = 114-07-8 | |||
| | Watchedfields = changed | |||
| | ATC_prefix=J01 | |||
| | verifiedrevid = 464189839 | |||
| | ATC_suffix=FA01 | |||
| | image = Erythromycin A skeletal.svg | |||
| | PubChem=3255 | |||
| | width = 200 | |||
| | DrugBank=APRD00953 | |||
| | alt = | |||
| |chemical_formula = {{Carbon}}<sub>37</sub>{{Hydrogen}}<sub>67</sub>{{Nitrogen}}{{Oxygen}}<sub>13</sub> |molecular_weight = 733.93]/] | |||
| | image2 = Erythromycin_3d_structure.png | |||
| |bioavailability = completely absorbed after oral administration | |||
| | width2 = | |||
| |metabolism = liver | |||
| | alt2 = | |||
| |elimination_half-life = | |||
| | caption = | |||
| |excretion = bile | |||
| |pregnancy_category = US: B; AU: A | |||
| <!-- Clinical data --> | |||
| |legal_status = ] | |||
| | pronounce = | |||
| |routes_of_administration = ], ], ] | |||
| | tradename = Eryc, Erythrocin, others<ref name=AHFS2015/> | |||
| | Drugs.com = {{drugs.com|monograph|erythromycin}} | |||
| | MedlinePlus = a682381 | |||
| | DailyMedID = Erythromycin | |||
| | pregnancy_AU = A | |||
| | pregnancy_AU_comment = <ref name=AG2015/> | |||
| | pregnancy_category = | |||
| | routes_of_administration = ], ], ], ], ] | |||
| | class = ] | |||
| | ATC_prefix = D10 | |||
| | ATC_suffix = AF02 | |||
| | ATC_supplemental = {{ATC|J01|FA01}} {{ATC|S01|AA17}} {{ATCvet|J51|FA01}} | |||
| <!-- Legal status --> | |||
| | legal_AU = S4 | |||
| | legal_AU_comment = | |||
| | legal_BR = <!-- OTC, A1, A2, A3, B1, B2, C1, C2, C3, C4, C5, D1, D2, E, F --> | |||
| | legal_BR_comment = | |||
| | legal_CA = <!-- OTC, Rx-only, Schedule I, II, III, IV, V, VI, VII, VIII --> | |||
| | legal_CA_comment = | |||
| | legal_DE = <!-- Anlage I, II, III or Unscheduled --> | |||
| | legal_DE_comment = | |||
| | legal_NZ = <!-- Class A, B, C --> | |||
| | legal_NZ_comment = | |||
| | legal_UK = POM | |||
| | legal_UK_comment = | |||
| | legal_US = Rx-only | |||
| | legal_US_comment = | |||
| | legal_EU = | |||
| | legal_EU_comment = | |||
| | legal_UN = <!-- N I, II, III, IV / P I, II, III, IV --> | |||
| | legal_UN_comment = | |||
| | legal_status = <!-- For countries not listed above --> | |||
| <!-- Pharmacokinetic data --> | |||
| | bioavailability = Depends on the ester type; between 30% and 65% | |||
| | protein_bound = 90% | |||
| | metabolism = Liver (under 5% excreted unchanged) | |||
| | metabolites = | |||
| | onset = | |||
| | elimination_half-life = 1.5 hours | |||
| | duration_of_action = | |||
| | excretion = Bile | |||
| <!-- Identifiers --> | |||
| | CAS_number_Ref = {{cascite|correct|??}} | |||
| | CAS_number = 114-07-8 | |||
| | CAS_supplemental = | |||
| | PubChem = 12560 | |||
| | IUPHAR_ligand = 1456 | |||
| | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| | DrugBank = DB00199 | |||
| | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| | ChemSpiderID = 12041 | |||
| | UNII_Ref = {{fdacite|correct|FDA}} | |||
| | UNII = 63937KV33D | |||
| | KEGG_Ref = {{keggcite|correct|kegg}} | |||
| | KEGG = D00140 | |||
| | ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| | ChEBI = 42355 | |||
| | ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| | ChEMBL = 532 | |||
| | NIAID_ChemDB = | |||
| | PDB_ligand = ERY | |||
| | synonyms = | |||
| <!-- Chemical and physical data --> | |||
| | IUPAC_name = (3''R'',4''S'',5''S'',6''R'',7''R'',9''R'',11''R'',12''R'',13''S'',14''R'')-6-{oxy}-14-ethyl-7,12,13-trihydroxy-4-{oxy}-3,5,7,9,11,13-hexamethyl-1-oxacyclotetradecane-2,10-dione | |||
| | C=37 | H=67 | N=1 | O=13 | |||
| | SMILES = CC1(((C(=O)(C(((((C(=O)O1)C)O2C(((O2)C)O)(C)OC)C)O3((C(O3)C)N(C)C)O)(C)O)C)C)O)(C)O | |||
| | Jmol = none <!-- SMILES renders as flat --> | |||
| | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | |||
| | StdInChI = 1S/C37H67NO13/c1-14-25-37(10,45)30(41)20(4)27(39)18(2)16-35(8,44)32(51-34-28(40)24(38(11)12)15-19(3)47-34)21(5)29(22(6)33(43)49-25)50-26-17-36(9,46-13)31(42)23(7)48-26/h18-26,28-32,34,40-42,44-45H,14-17H2,1-13H3/t18-,19-,20+,21+,22-,23+,24+,25-,26+,28-,29+,30-,31+,32-,34+,35-,36-,37-/m1/s1 | |||
| | StdInChI_comment = | |||
| | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | |||
| | StdInChIKey = ULGZDMOVFRHVEP-RWJQBGPGSA-N | |||
| | density = | |||
| | density_notes = | |||
| | melting_point = | |||
| | melting_high = | |||
| | melting_notes = | |||
| | boiling_point = | |||
| | boiling_notes = | |||
| | solubility = | |||
| | sol_units = | |||
| | specific_rotation = | |||
| }} | }} | ||
| '''Erythromycin''' is a ] ] which has an antimicrobial spectrum similar to or slightly wider than that of ], and is often used for people who have an ] to penicillins - this is not necessarily a good idea , as after all , erythromycin is '''itself''' a penicillin '''derivative'''. It is more likely that a medicine from a different family of anti-biotics would be prescribed, eg. metronidazole. Moving back onto Erythromycin now which is very useful in the treatment of respiratory tract infections, it has better coverage of atypical organisms, including ]. It is also used to treat outbreaks of ], ], and ]. Structurally, this macrocyclic compound contains a 14-membered ] ring with ten asymmetric centers and two sugars (L-cladinose and D-desoamine), making it a compound very difficult to produce via synthetic methods. | |||
| <!-- Definition and medical uses --> | |||
| Erythromycin is produced from a strain of the ] '']'', formerly known as ''Streptomyces erythraeus''. | |||
| '''Erythromycin''' is an ] used for the treatment of a number of ]s.<ref name=AHFS2015/> This includes ], ], ], ], and ].<ref name=AHFS2015/> It may also be used during ] to prevent ] in the newborn,<ref name=AHFS2015/> and to improve ].<ref>{{cite journal | vauthors = Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L | title = Clinical guideline: management of gastroparesis | journal = The American Journal of Gastroenterology | volume = 108 | issue = 1 | pages = 18–37; quiz 38 | date = January 2013 | pmid = 23147521 | pmc = 3722580 | doi = 10.1038/ajg.2012.373 }}</ref> It can be given ]ly and by mouth.<ref name=AHFS2015/> An eye ointment is routinely recommended after ] to prevent ].<ref>{{cite journal | vauthors = Matejcek A, Goldman RD | title = Treatment and prevention of ophthalmia neonatorum | journal = Canadian Family Physician | volume = 59 | issue = 11 | pages = 1187–90 | date = November 2013 | pmid = 24235191 | pmc = 3828094 }}</ref> | |||
| <!-- Side effects and mechanism --> | |||
| Common side effects include abdominal cramps, vomiting, and diarrhea.<ref name=AHFS2015/> More serious side effects may include ], liver problems, ], and ]s.<ref name=AHFS2015/> It is generally safe in those who are ].<ref name=AHFS2015>{{cite web |title=Erythromycin|url=https://www.drugs.com/monograph/erythromycin.html |publisher=The American Society of Health-System Pharmacists |access-date=1 August 2015 |url-status=live|archive-url=https://web.archive.org/web/20150906031153/http://www.drugs.com/monograph/erythromycin.html|archive-date=6 September 2015}}</ref> Erythromycin also appears to be safe to use during pregnancy.<ref name=AG2015>{{cite web |title=Prescribing medicines in pregnancy database|url=http://www.tga.gov.au/hp/medicines-pregnancy.htm |work=Australian Government |date=23 August 2015|url-status=live|archive-url=https://web.archive.org/web/20140408040902/http://www.tga.gov.au/hp/medicines-pregnancy.htm#.U1Yw8Bc3tqw|archive-date=8 April 2014}}</ref> While generally regarded as safe during ], its use by the mother during the first two weeks of life may increase the risk of ] in the baby.<ref name=Ric2013>{{cite book|vauthors=Hamilton RJ|title=Tarascon pocket pharmacopoeia|date=2013|publisher=Jones & Bartlett Learning|location=|isbn=9781449673611|page=72|edition=2013 delux lab-coat ed., 14th|url=https://books.google.com/books?id=zJay-fZCFGgC&pg=PA72|access-date=9 September 2017|archive-date=1 August 2020|archive-url=https://web.archive.org/web/20200801095144/https://books.google.com/books?id=zJay-fZCFGgC&pg=PA72|url-status=live}}</ref><ref name="Kong2013">{{cite journal | vauthors = Kong YL, Tey HL | title = Treatment of acne vulgaris during pregnancy and lactation | journal = Drugs | volume = 73 | issue = 8 | pages = 779–87 | date = June 2013 | pmid = 23657872 | doi = 10.1007/s40265-013-0060-0 | s2cid = 45531743 }}</ref> This risk also applies if taken directly by the baby during this age.<ref name=Erythromycin>{{cite journal | vauthors = Maheshwai N | title = Are young infants treated with erythromycin at risk for developing hypertrophic pyloric stenosis? | journal = Archives of Disease in Childhood | volume = 92 | issue = 3 | pages = 271–3 | date = March 2007 | pmid = 17337692 | pmc = 2083424 | doi = 10.1136/adc.2006.110007 | url = http://adc.bmj.com/content/92/3/271| archive-url = https://web.archive.org/web/20121107021907/http://adc.bmj.com/content/92/3/271 | url-status = live | archive-date = 7 November 2012 }}</ref> It is in the ] family of antibiotics and works by decreasing bacterial protein production.<ref name=AHFS2015/> | |||
| <!-- History, society and culture --> | |||
| Erythromycin was first isolated in 1952 from the bacteria '']''.<ref name=AHFS2015/><ref>{{cite book|vauthors=Vedas JC|title=Biosynthesis : polyketides and vitamins|date=2000|publisher=Springer|location=Berlin |isbn=9783540669692|page=52|url=https://books.google.com/books?id=XUuFPxvfWgAC&pg=PA52|access-date=9 September 2017|archive-date=1 August 2020|archive-url=https://web.archive.org/web/20200801110901/https://books.google.com/books?id=XUuFPxvfWgAC&pg=PA52|url-status=live}}</ref> It is on the ].<ref name="WHO22nd">{{cite book | vauthors = ((World Health Organization)) | title = World Health Organization model list of essential medicines: 22nd list (2021) | year = 2021 | hdl = 10665/345533 | author-link = World Health Organization | publisher = World Health Organization | location = Geneva | id = WHO/MHP/HPS/EML/2021.02 | hdl-access=free }}</ref> In 2022, it was the 271st most commonly prescribed medication in the United States, with more than 800,000 prescriptions.<ref>{{cite web | title=The Top 300 of 2022 | url=https://clincalc.com/DrugStats/Top300Drugs.aspx | website=ClinCalc | access-date=30 August 2024 | archive-date=30 August 2024 | archive-url=https://web.archive.org/web/20240830202410/https://clincalc.com/DrugStats/Top300Drugs.aspx | url-status=live }}</ref><ref>{{cite web | title = Erythromycin Drug Usage Statistics, United States, 2013 - 2022 | website = ClinCalc | url = https://clincalc.com/DrugStats/Drugs/Erythromycin | access-date = 30 August 2024 }}</ref> | |||
| {{TOC limit}} | |||
| == Medical uses == | |||
| Erythromycin can be used to treat bacteria responsible for causing infections of the skin and upper respiratory tract, including '']'', '']'', '']'' and ] genera. The following represents MIC susceptibility data for a few medically significant bacteria:<ref name = "www.toku-e.com">{{cite web | url = http://www.toku-e.com/Assets/MIC/Erythromycin.pdf | title = Erythromycin Susceptibility and Minimum Inhibitory Concentration (MIC) Data | publisher = TOKU-E | access-date = 26 February 2014 | archive-date = 9 May 2015 | archive-url = https://web.archive.org/web/20150509091111/http://www.toku-e.com/Assets/MIC/Erythromycin.pdf | url-status = live }}</ref> | |||
| * ''Haemophilus influenzae'': 0.015 to 256 μg/ml | |||
| * ''Staphylococcus aureus'': 0.023 to 1024 μg/ml | |||
| * ''Streptococcus pyogenes'': 0.004 to 256 μg/ml | |||
| * ''Corynebacterium minutissimum'': 0.015 to 64 μg/ml | |||
| It may be useful in treating ] due to this promotility effect. It has been shown to improve feeding intolerances in those who are critically ill.<ref>{{cite journal | vauthors = Lewis K, Alqahtani Z, Mcintyre L, Almenawer S, Alshamsi F, Rhodes A, Evans L, Angus DC, Alhazzani W | title = The efficacy and safety of prokinetic agents in critically ill patients receiving enteral nutrition: a systematic review and meta-analysis of randomized trials | journal = Critical Care | volume = 20 | issue = 1 | pages = 259 | date = August 2016 | pmid = 27527069 | pmc = 4986344 | doi = 10.1186/s13054-016-1441-z | doi-access = free }}</ref> Intravenous erythromycin may also be used in ] to help clear ] contents to enhance endoscopic visualization, potentially improving diagnostic accuracy and subsequent management.<ref>{{cite journal | vauthors = Laine L, Barkun AN, Saltzman JR, Martel M, Leontiadis GI | title = ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding | journal = The American Journal of Gastroenterology | volume = 116 | issue = 5 | pages = 899–917 | date = May 2021 | pmid = 33929377 | doi = 10.14309/ajg.0000000000001245 }}</ref> | |||
| === Available forms === | |||
| ] | |||
| Erythromycin is available in ] tablets, slow-release capsules, oral suspensions, ophthalmic solutions, ointments, gels, enteric-coated capsules, non enteric-coated tablets, non enteric-coated capsules, and injections. | |||
| The following erythromycin combinations are available for oral dosage:<ref name=drugs.com>{{cite web | url = https://www.drugs.com/cons/erythromycin-oral-parenteral.html | title = Erythromycin Oral, Parenteral Advanced Patient Information | work = Drugs.com | url-status = live | archive-url = https://web.archive.org/web/20091130183915/http://www.drugs.com/cons/erythromycin-oral-parenteral.html | archive-date = 30 November 2009 }}</ref> | |||
| * erythromycin base (capsules, tablets) | |||
| * erythromycin estolate (capsules, oral suspension, tablets), contraindicated during pregnancy<ref name="pmid16888612">{{cite journal | vauthors = Workowski KA, Berman SM | title = Sexually transmitted diseases treatment guidelines, 2006 | journal = MMWR: Recommendations and Reports | volume = 55 | issue = RR-11 | pages = 1–94 | date = August 2006 | pmid = 16888612 | doi = | url = https://www.cdc.gov/std/treatment/2006/toc.htm | archive-url = https://web.archive.org/web/20100211154655/http://www.cdc.gov/std/treatment/2006/toc.htm | archive-date=11 February 2010}}</ref> | |||
| * erythromycin ethylsuccinate (oral suspension, tablets) | |||
| * erythromycin stearate (oral suspension, tablets) | |||
| For injection, the available combinations are:<ref name=drugs.com/> | |||
| * erythromycin gluceptate | |||
| * erythromycin lactobionate | |||
| For ophthalmic use: | |||
| * erythromycin base (ointment) | |||
| == Adverse effects == | |||
| Gastrointestinal disturbances, such as ], ], ], and ], are very common because erythromycin is a ] agonist.<ref name="pmid8470625">{{cite journal | vauthors = Weber FH, Richards RD, McCallum RW | title = Erythromycin: a motilin agonist and gastrointestinal prokinetic agent | journal = The American Journal of Gastroenterology | volume = 88 | issue = 4 | pages = 485–90 | date = April 1993 | pmid = 8470625 }}</ref> | |||
| More serious side effects include ] with ]s, including '']'', and reversible ]. Allergic reactions range from ] to ]. ] and ] are some other rare side effects that may occur.<ref>{{cite book |title=Meyler's Side Effects of Drugs |publisher=Elsevier |year=2016 |pages=99–108 |url= | veditors = Aronson JK |chapter=Erythromycin |edition=Sixteenth |doi=10.1016/B978-0-444-53717-1.00698-3 |isbn=9780444537164 |chapter-url=https://www.sciencedirect.com/science/article/abs/pii/B9780444537171006983}}</ref> | |||
| Studies have shown evidence both for and against the association of ] and exposure to erythromycin prenatally and postnatally.<ref name = "Briggs_2011">{{cite book |vauthors=Briggs GG, Freeman RK, Yaffe SJ |title=Drugs in pregnancy and lactation : a reference guide to fetal and neonatal risk |date=2011 |publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins |location=Philadelphia |isbn=978-1-60831-708-0 |edition=9th |chapter=Erythromycin |chapter-url=https://books.google.com/books?id=OIgTE4aynrMC&q=erythromycin&pg=PA512 |access-date=20 October 2021 |archive-date=23 May 2022 |archive-url=https://web.archive.org/web/20220523131602/https://books.google.com/books?id=OIgTE4aynrMC&q=erythromycin&pg=PA512 |url-status=live }}</ref> Exposure to erythromycin (especially long courses at antimicrobial doses, and also through ]) has been linked to an increased probability of pyloric stenosis in young infants.<ref name="pmid17337692">{{cite journal | vauthors = Maheshwai N | title = Are young infants treated with erythromycin at risk for developing hypertrophic pyloric stenosis? | journal = Archives of Disease in Childhood | volume = 92 | issue = 3 | pages = 271–3 | date = March 2007 | pmid = 17337692 | pmc = 2083424 | doi = 10.1136/adc.2006.110007 }}</ref><ref name="pmid24618148">{{cite journal | vauthors = Lund M, Pasternak B, Davidsen RB, Feenstra B, Krogh C, Diaz LJ, Wohlfahrt J, Melbye M | title = Use of macrolides in mother and child and risk of infantile hypertrophic pyloric stenosis: nationwide cohort study | journal = BMJ | volume = 348 | pages = g1908 | date = March 2014 | pmid = 24618148 | pmc = 3949411 | doi = 10.1136/bmj.g1908 }}</ref> Erythromycin used for feeding intolerance in young infants has not been associated with hypertrophic pyloric stenosis.<ref name="pmid17337692"/> | |||
| Erythromycin estolate has been associated with reversible hepatotoxicity in pregnant women in the form of elevated serum glutamic-oxaloacetic transaminase and is not recommended during pregnancy. Some evidence suggests similar hepatotoxicity in other populations.<ref>{{cite journal | vauthors = McCormack WM, George H, Donner A, Kodgis LF, Alpert S, Lowe EW, Kass EH | title = Hepatotoxicity of erythromycin estolate during pregnancy | journal = Antimicrobial Agents and Chemotherapy | volume = 12 | issue = 5 | pages = 630–5 | date = November 1977 | pmid = 21610 | pmc = 429989 | doi = 10.1128/AAC.12.5.630 }}</ref> | |||
| It can also affect the ], causing ], nightmares, and night sweats.<ref name="BCFI"/> | |||
| == Interactions == | |||
| Erythromycin is metabolized by enzymes of the ] system, in particular, by ] of the ] superfamily.<ref name="pmid1732074">{{cite journal | vauthors = Hunt CM, Watkins PB, Saenger P, Stave GM, Barlascini N, Watlington CO, Wright JT, Guzelian PS | title = Heterogeneity of CYP3A isoforms metabolizing erythromycin and cortisol | journal = Clinical Pharmacology and Therapeutics | volume = 51 | issue = 1 | pages = 18–23 | date = January 1992 | pmid = 1732074 | doi = 10.1038/clpt.1992.3 | hdl = 2027.42/109905 | s2cid = 28056649 | url = https://deepblue.lib.umich.edu/bitstream/2027.42/109905/1/cptclpt19923.pdf | hdl-access = free | access-date = 29 August 2019 | archive-date = 28 August 2021 | archive-url = https://web.archive.org/web/20210828075533/https://deepblue.lib.umich.edu/bitstream/handle/2027.42/109905/cptclpt19923.pdf;jsessionid=E4EB0A4C0D1D5A07533C041190B23FA0?sequence=1 | url-status = live }}</ref> The activity of the CYP3A enzymes can be induced or inhibited by certain drugs (e.g., dexamethasone), which can cause it to affect the ] of many different drugs, including erythromycin. If other CYP3A substrates — drugs that are broken down by CYP3A — such as ] (Zocor), ] (Mevacor), or ] (Lipitor) — are taken concomitantly with erythromycin, levels of the substrates increase, often causing adverse effects. A noted drug interaction involves erythromycin and simvastatin, resulting in increased simvastatin levels and the potential for ]. Another group of CYP3A4 substrates are drugs used for ] such as ] and ]; their adverse effects may be more pronounced if erythromycin is associated.<ref name="BCFI">{{cite web | url = http://www.bcfi.be/GGR/MPG/MPG_KABA.cfm | title = Erythromycine | work = Belgisch Centrum voor Farmacotherapeutische Informatie | url-status = live | archive-url = https://web.archive.org/web/20151006100756/http://www.bcfi.be/GGR/MPG/MPG_KABA.cfm | archive-date = 6 October 2015 }}</ref> | |||
| Earlier case reports on sudden death prompted a study on a large cohort that confirmed a link between erythromycin, ], and sudden cardiac death in patients also taking drugs that prolong the metabolism of erythromycin (like ] or ]) by interfering with CYP3A4.<ref>{{cite journal | vauthors = Ray WA, Murray KT, Meredith S, Narasimhulu SS, Hall K, Stein CM | title = Oral erythromycin and the risk of sudden death from cardiac causes | journal = The New England Journal of Medicine | volume = 351 | issue = 11 | pages = 1089–96 | date = September 2004 | pmid = 15356306 | doi = 10.1056/NEJMoa040582 | doi-access = free }}</ref> Hence, erythromycin should not be administered to people using these drugs, or drugs that also prolong the ]. Other examples include ] (Seldane, Seldane-D),<ref>{{cite web |url=https://www.drugs.com/drug-interactions/erythromycin-with-terfenadine-1009-0-2164-0.html?professional=1 |title=Drug Interactions between erythromycin and terfenadine |access-date=21 December 2023 |website=Drugs.com}}</ref> ] (Hismanal),<ref>{{cite web |url=https://www.drugs.com/drug-interactions/astemizole-with-erythromycin-271-0-1009-0.html?professional=1 |title=Drug Interactions between astemizole and erythromycin |access-date=21 December 2023 |website=Drugs.com}}</ref> ]<ref>{{cite journal | vauthors = Michalets EL, Williams CR | title = Drug interactions with cisapride: clinical implications | journal = Clinical Pharmacokinetics | volume = 39 | issue = 1 | pages = 49–75 | date = July 2000 | pmid = 10926350 | doi = 10.2165/00003088-200039010-00004 | s2cid = 41704853 }}</ref> (Propulsid, withdrawn in many countries for prolonging the QT time) and ] (Orap).<ref>{{cite web |url=https://gpnotebook.com/pages/ear-nose-and-throat/erythromycin/interactions |title=Erythromycin Interactions |date=20 December 2020 |access-date=21 December 2023 |website=GPnotebook |archive-url=https://web.archive.org/web/20231221161502/https://gpnotebook.com/pages/ear-nose-and-throat/erythromycin/interactions |archive-date=21 December 2023 |url-status=live}}</ref> Interactions with ], which is used mostly in asthma, were also shown.<ref>{{cite web |url=https://www.drugs.com/drug-interactions/erythromycin-with-theophylline-1009-0-2177-0.html?professional=1 |title=Drug Interactions between erythromycin and theophylline |access-date=21 December 2023 |website=Drugs.com |archive-url=https://web.archive.org/web/20231221104101/https://www.drugs.com/drug-interactions/erythromycin-with-theophylline-1009-0-2177-0.html?professional=1 |archive-date=21 December 2023 |url-status=live}}</ref> | |||
| Erythromycin and ] can have a synergistic effect when combined and kill bacteria (''E. coli)'' with a higher potency than the sum of the two drugs together. This synergistic relationship is only temporary. After approximately 72 hours, the relationship shifts to become antagonistic, whereby a 50/50 combination of the two drugs kills less bacteria than if the two drugs were administered separately.<ref>{{cite journal | vauthors = Pena-Miller R, Laehnemann D, Jansen G, Fuentes-Hernandez A, Rosenstiel P, Schulenburg H, Beardmore R | title = When the most potent combination of antibiotics selects for the greatest bacterial load: the smile-frown transition | journal = PLOS Biology | volume = 11 | issue = 4 | pages = e1001540 | date = 23 April 2013 | pmid = 23630452 | pmc = 3635860 | doi = 10.1371/journal.pbio.1001540 | doi-access = free }}</ref> | |||
| It may alter the effectiveness of ]s because of its effect on the gut flora. A review found that when erythromycin was given with certain oral contraceptives, there was an increase in the maximum serum concentrations and ] of ] and ].<ref>{{cite journal | vauthors = Blode H, Zeun S, Parke S, Zimmermann T, Rohde B, Mellinger U, Kunz M | title = Evaluation of the effects of rifampicin, ketoconazole and erythromycin on the steady-state pharmacokinetics of the components of a novel oral contraceptive containing estradiol valerate and dienogest in healthy postmenopausal women | language = en | journal = Contraception | volume = 86 | issue = 4 | pages = 337–44 | date = October 2012 | pmid = 22445438 | doi = 10.1016/j.contraception.2012.01.010 | url = https://www.contraceptionjournal.org/article/S0010-7824(12)00041-8/abstract | access-date = 2 August 2019 | archive-date = 28 August 2021 | archive-url = https://web.archive.org/web/20210828075535/https://www.contraceptionjournal.org/article/S0010-7824%2812%2900041-8/fulltext | url-status = live }}</ref><ref>{{cite journal | vauthors = Simmons KB, Haddad LB, Nanda K, Curtis KM | title = Drug interactions between non-rifamycin antibiotics and hormonal contraception: a systematic review | language = en | journal = American Journal of Obstetrics and Gynecology | volume = 218 | issue = 1 | pages = 88–97.e14 | date = January 2018 | pmid = 28694152 | doi = 10.1016/j.ajog.2017.07.003 | s2cid = 36567820 | url = https://www.ajog.org/article/S0002-9378(17)30845-1/abstract | access-date = 2 August 2019 | archive-date = 28 August 2021 | archive-url = https://web.archive.org/web/20210828075543/https://www.ajog.org/article/S0002-9378%2817%2930845-1/fulltext | url-status = live }}</ref> | |||
| Erythromycin is an inhibitor of the cytochrome P450 system, which means it can have a rapid effect on levels of other drugs metabolised by this system, e.g., ].<ref>{{cite journal | vauthors = Westphal JF | title = Macrolide - induced clinically relevant drug interactions with cytochrome P-450A (CYP) 3A4: an update focused on clarithromycin, azithromycin and dirithromycin | journal = British Journal of Clinical Pharmacology | volume = 50 | issue = 4 | pages = 285–295 | date = October 2000 | pmid = 11012550 | pmc = 2015000 | doi = 10.1046/j.1365-2125.2000.00261.x }}</ref> | |||
| == Pharmacology == | |||
| === Mechanism of action === | |||
| Erythromycin displays ] activity or inhibits growth of bacteria, especially at higher concentrations.<ref name = "Trevor_2010">{{cite book | chapter = Section VIII: Chemotherapeutic Drugs; Chapter 44: Chloramphenicol, Tetracyclines, Macrolides, Clindamycin, & Streptogramins | pages = 389–396 | veditors = Trevor AJ, Katzung BG, Masters SB |title = Katzung & Trevor's Pharmacology: Examination & Board Review |date=2010 |publisher=McGraw-Hill Medical |location=New York |isbn=978-0-07-170155-6 |edition=9th}}</ref> By binding to the 50s subunit of the bacterial ] complex, protein synthesis and subsequent structure and function processes critical for life or replication are inhibited.<ref name="Trevor_2010"/> Erythromycin interferes with aminoacyl translocation, preventing the transfer of the ] bound at the ] of the rRNA complex to the ] of the rRNA complex.<ref>{{cite web |url=https://www.sigmaaldrich.com/SE/en/product/sial/e6376 |title=Erythromycin |access-date=21 December 2023 |website=Sigma-Aldrich}}</ref> Without this translocation, the A site remains occupied, thus the addition of an incoming tRNA and its attached ] to the nascent ] chain is inhibited.{{medical citation needed|date=December 2023}} This interferes with the production of functionally useful proteins, which is the basis of this antimicrobial action.{{medical citation needed|date=December 2023}} | |||
| Erythromycin increases gut motility by binding to ], thus it is a motilin receptor agonist in addition to its antimicrobial properties. It can be therefore administered intravenously as a stomach emptying stimulant.<ref>{{cite book |title=Gastroparesis: Pathophysiology, Clinical Presentation, Diagnosis and Treatment | vauthors = Parkman HP |publisher=Academic Press |year=2021 |pages=323–339 |chapter=Chapter 24 - Prokinetic agents for gastroparesis |doi=10.1016/B978-0-12-818586-5.00024-7 |isbn=9780128185865 |quote=Erythromycin has prokinetic effects because it is a motilin receptor agonist in addition to being an antibiotic. When given intravenously, erythromycin is a potent stimulant of gastric emptying among the available prokinetic drugs. |chapter-url=https://www.sciencedirect.com/science/article/abs/pii/B9780128185865000247}}</ref> | |||
| === Pharmacokinetics === | |||
| Erythromycin is easily inactivated by gastric acid; therefore, all orally administered formulations are given as either enteric-coated or more-stable salts or ]s, such as erythromycin ]. Erythromycin is very rapidly absorbed, and diffuses into most tissues and ]s. Due to the high concentration in phagocytes, erythromycin is actively transported to the site of infection, where, during active ], large concentrations of erythromycin are released.<ref>{{cite journal | vauthors = Lebel M | title = Pharmacokinetic properties of clarithromycin: A comparison with erythromycin and azithromycin | journal = The Canadian Journal of Infectious Diseases | volume = 4 | issue = 3 | pages = 148–152 | date = May 1993 | pmid = 22346438 | pmc = 3250788 | doi = 10.1155/1993/168061 | doi-access = free }}</ref> | |||
| === Metabolism === | |||
| Most of erythromycin is metabolised by ] in the ] by the hepatic enzyme CYP3A4. Its main elimination route is in the ] with little renal excretion, 2%–15% unchanged drug. Erythromycin's ] ranges between 1.5 and 2.0 hours and is between 5 and 6 hours in patients with end-stage renal disease. Erythromycin levels peak in the serum 4 hours after dosing; ethylsuccinate peaks 0.5–2.5 hours after dosing, but can be delayed if digested with food.<ref name = "Edmunds_2009">{{cite book |vauthors=Edmunds MW, Mayhew MS |title=Pharmacology for the primary care provider |date=2009 |location=Saint Louis, Missouri | publisher = Elsevier Health Sciences |isbn=978-0-323-06316-6 |edition=Third |chapter=Chapter 61: Macrolides |pages=658–662 (661) |chapter-url=https://books.google.com/books?id=9JtgGU0fkggC&pg=PA661 |access-date=3 March 2022 |archive-date=23 May 2022 |archive-url=https://web.archive.org/web/20220523131602/https://books.google.com/books?id=9JtgGU0fkggC&pg=PA661 |url-status=live }}; {{cite book | vauthors = Kirst HA, Sides GD | date = 1993 | chapter = Chapter 28: Erythromycin | veditors = Bryskier A, Butzler JP, Neu HC, Tulkens | title = The Macrolides | publisher = Arnette-Blackwell | location = Oxford UK }}</ref> | |||
| Erythromycin crosses the placenta and enters breast milk. The American Association of Pediatrics determined erythromycin is safe to take while breastfeeding.<ref name="urlwww.breastfeedingmadesimple.com">{{cite journal | title = Transfer of drugs and other chemicals into human milk | journal = Pediatrics | volume = 108 | issue = 3 | pages = 776–89 | date = September 2001 | pmid = 11533352 | doi = 10.1542/peds.108.3.776 | author1 = American Academy of Pediatrics Committee on Drugs | doi-access = free }}</ref> Absorption in pregnant patients has been shown to be variable, frequently resulting in levels lower than in nonpregnant patients.<ref name="Philipson_1976">{{cite journal | vauthors = Philipson A, Sabath LD, Charles D | title = Erythromycin and clindamycin absorption and elimination in pregnant women | journal = Clinical Pharmacology and Therapeutics | volume = 19 | issue = 1 | pages = 68–77 | date = January 1976 | pmid = 1245094 | doi = 10.1002/cpt197619168 | s2cid = 7573420 }}</ref><ref name = "Briggs_2011" /> | |||
| == Chemistry == | |||
| === Composition === | |||
| Standard-grade erythromycin is primarily composed of four related compounds known as erythromycins A, B, C, and D. Each of these compounds can be present in varying amounts and can differ by lot. Erythromycin A has been found to have the most antibacterial activity, followed by erythromycin B. Erythromycins C and D are about half as active as erythromycin A.<ref name = "www.toku-e.com"/><ref name="pmid4091529">{{cite journal | vauthors = Kibwage IO, Hoogmartens J, Roets E, Vanderhaeghe H, Verbist L, Dubost M, Pascal C, Petitjean P, Levol G | title = Antibacterial activities of erythromycins A, B, C, and D and some of their derivatives | journal = Antimicrobial Agents and Chemotherapy | volume = 28 | issue = 5 | pages = 630–3 | date = November 1985 | pmid = 4091529 | pmc = 176346 | doi = 10.1128/aac.28.5.630 }}</ref> Some of these related compounds have been purified and can be studied and researched individually. | |||
| === Synthesis === | |||
| Over the three decades after the discovery of erythromycin A and its activity as an antimicrobial, many attempts were made to synthesize it in the laboratory. The presence of 10 stereogenic carbons and several points of distinct substitution has made the total synthesis of erythromycin A a formidable task.<ref>{{cite journal | vauthors = Pal S | year = 2006 | title = A journey across the sequential development of macrolides and ketolides related to erythromycin | journal = Tetrahedron | volume = 62 | issue = 14| pages = 3171–3200 | doi = 10.1016/j.tet.2005.11.064 }}</ref> Complete syntheses of erythromycins’ related structures and precursors such as 6-deoxyerythronolide B have been accomplished, giving way to possible syntheses of different erythromycins and other macrolide antimicrobials.<ref>{{cite journal | vauthors = Evans DA, Kim AS | year = 1997 | title = Synthesis of 6-Deoxyerythronolide B. Implementation of a General Strategy for the Synthesis of Macrolide Antibiotics | journal = Tetrahedron Lett. | volume = 38 | pages = 53–56 | doi = 10.1016/S0040-4039(96)02258-7 }}</ref> ] successfully completed the synthesis of erythromycin A, which was published in 1981.<ref>{{cite journal | vauthors = Woodward RB, Logusch E, Nambiar KP, Sakan K, Ward DE, Au-Yeung BW, Balaram P, Browne LJ, Card PJ, Chen CH | date = June 1981 | title = Asymmetric Total Synthesis of Erythromycin. 1. Synthesis of an Erythronolide A Seco Acid Derivative via Asymmetric Induction | journal = Journal of the American Chemical Society | volume = 103 | issue = 11| pages = 3210–3213 | doi = 10.1021/ja00401a049 | bibcode = 1981JAChS.103.3210W }}</ref><ref>{{cite journal | vauthors = Woodward RB, Au-Yeung BW, Balaram P, Browne LJ, Ward DE, Au-Yeung BW, Balaram P, Browne LJ, Card PJ, Chen CH | year = 1981 | title = Asymmetric Total Synthesis of Erythromycin. 2. Synthesis of an Erythronolide A Lactone System | journal = Journal of the American Chemical Society | volume = 103 | issue = 11| pages = 3213–3215 | doi = 10.1021/ja00401a050 | bibcode = 1981JAChS.103.3213W }}</ref><ref>{{cite journal | vauthors = Woodward RB, Logusch E, Nambiar KP, Sakan K, Ward DE, Au-Yeung BW, Balaram P, Browne LJ, Card PJ, Chen CH | date = June 1981 | title = Asymmetric Total Synthesis of Erythromycin. 3. Total Synthesis of Erythromycin | journal =Journal of the American Chemical Society | volume = 103 | issue = 11| pages = 3215–3217 | doi = 10.1021/ja00401a051 | bibcode = 1981JAChS.103.3215W }}</ref> | |||
| == History == | == History == | ||
| Abelardo Aguilar, a Filipino scientist, sent some soil samples to his employer ] in ]. Eli Lilly’s research team, led by J. M. McGuire, managed to isolate Erythromycin from the metabolic products of a strain of ''Streptomyces erythreus'' found in the samples. The product was subsequently launched in ] under the brand name '''Ilosone®''' (after the ] region of ] where it was originally collected from). Erythromycin was formerly also called '''Ilotycin®'''. In 1981, Nobel laurate (1965 in chemistry) and Professor of Chemistry at ] (]) ] and a large team of researchers reported the first stereocontrolled asymmetric chemical synthesis of Erythromycin A. | |||
| In 1949 ], a Filipino scientist, sent some soil samples to his employer at ].<ref>{{cite news | vauthors = Tan ML |title=Drugs and rights |url=https://opinion.inquirer.net/123626/drugs-and-rights |access-date=4 November 2021 |newspaper=] |date=30 August 2019 |language=en |archive-date=28 February 2021 |archive-url=https://web.archive.org/web/20210228125609/https://opinion.inquirer.net/123626/drugs-and-rights |url-status=live }}</ref> Aguilar managed to isolate erythromycin from the metabolic products of a strain of ''Streptomyces erythreus'' (designation changed to '']'') found in the samples. Aguilar received no further credit or compensation for his discovery.<ref>{{cite news |url=https://opinion.inquirer.net/123626/drugs-and-rights |title=Drugs and rights |date=30 August 2019 |access-date=21 December 2023 |newspaper=] | vauthors = Tan ML }}</ref> | |||
| == Available forms == | |||
| Erythromycin is available in enteric-coated tablets, oral suspensions, ophthalmic solutions, ointments, gels and injections. | |||
| The scientist was allegedly promised a trip to the company's manufacturing plant in Indianapolis, but it was never fulfilled. In a letter to the company's president, Aguilar wrote: “A leave of absence is all I ask as I do not wish to sever my connection with a great company which has given me wonderful breaks in life.” The request was not granted.<ref name=the-news-today /> | |||
| Brand names include Robimycin, E-Mycin, E.E.S. Granules, E.E.S.-200, E.E.S.-400, E.E.S.-400 Filmtab, Ery-Tab, Eryc, EryPed, Eryped 200, Eryped 400, Erythrocin Stearate Filmtab, Erythrocot, E-Base, Ilosone, MY-E, Pediamycin, and PCE Dispertab. | |||
| Aguilar reached out to Eli Lilly again in 1993, requesting royalties from sales of the drug over the years, intending to use them to put up a foundation for poor and sickly Filipinos. This request was also denied. He died in September of the same year.<ref name=the-news-today>{{cite web | vauthors = Hibionada FF | title = Remembering the battle of Dr. Abelardo Aguilar: Cure for millions, deprived of millions. | work = The News Today | access-date = 22 September 2015 | url = https://www.thenewstoday.info/2005/05/03/iloilonews3.htm | archive-date = 18 September 2021 | archive-url = https://web.archive.org/web/20210918004325/https://www.thenewstoday.info/2005/05/03/iloilonews3.htm | url-status = live }}</ref> | |||
| == Mechanism of action == | |||
| Erythromycin prevents ] from growing, by interfering with their ]. Erythromycin binds to the 23s rRNA molecule in the 50S of the bacterial ], blocking the exit of the growing peptide chain thus inhibiting the translocation of ]s. | |||
| Lilly filed for patent protection on the compound which was granted in 1953.<ref>{{cite patent | country = US | number = 2653899 | title = Erythromycin, its salts, and method of preparation | inventor = Bunch RL, Mcguire JM | assign1 = Eli Lilly and Company | pubdate = 29 September 1953 | postscript = . }}</ref> The product was launched commercially in 1952 under the brand name Ilosone (after the ] region of ] where it was originally collected). Erythromycin was formerly also called Ilotycin. | |||
| == Pharmacokinetics == | |||
| Erythromycin is easily inactivated by gastric acids, therefore all orally administered formulations are given as either enteric coated or as more stable salts or ]s. Erythromycin is very rapidly absorbed, and diffused into most tissues and ]s. Due to the high concentration in phagocytes, erythromycin is actively transported to the site of infection, where during active phagocytosis, large concentrations of erythromycin are released. | |||
| The antibiotic ] was invented by scientists at the Japanese drug company ] in the 1970s as a result of their efforts to overcome the acid instability of erythromycin.<ref>{{cite book | vauthors = Greenwood D |url=https://books.google.com/books?id=i4_FZHmzjzwC&pg=PA239 |title=Antimicrobial drugs: chronicle of a twentieth century medical triumph |date=2008 |publisher=Oxford university press |isbn=978-0-19-953484-5 |location=New York |pages=239}}</ref> | |||
| == Metabolism == | |||
| Most of erythromycin is metabolised by demethylation in the liver. Its main elimination route is in the bile, and a small portion in the urine. Erythromycin's half-life is 1.5 hours. | |||
| == |
== Society and culture == | ||
| Gastrointestinal intestinal disturbances such as ], ], ] and ] are fairly common so it tends not to be prescribed as a first-line drug. However, erythromycin may be useful in treating ] due to this pro-motility effect. Erythromycin may also be used in ] as an adjunct to clear ] contents. | |||
| === Economics === | |||
| More serious side-effects, such as reversible ] are rare. Allergic reactions, while uncommon, may occur, ranging from ] to ]. ], ] and ] are some other rare side effects that may occur. | |||
| It is available as a ].<ref name=Ric2013 /> | |||
| Erythromycin has been shown to increase the probability of ] in children whose mothers took the drug during the late stages of pregnancy or while nursing. | |||
| In the United States, in 2014, the price increased to seven dollars per 500mg tablet.<ref name="increase">{{cite web | vauthors = Stahl S | date = 26 September 2014 | url = http://philadelphia.cbslocal.com/2014/09/26/health-generic-drugs-prices-increasing/ | title = Health: Generic Drugs Prices Increasing | archive-url = https://web.archive.org/web/20160409212651/http://philadelphia.cbslocal.com/2014/09/26/health-generic-drugs-prices-increasing/ | archive-date=9 April 2016 | work = CBS Philadelphia | access-date = 24 March 2016 }}</ref> | |||
| == Contraindications == | |||
| Earlier case reports on sudden death prompted a study on a large cohort that confirmed a link between erythromycin, ] and sudden cardiac death in patients also taking drugs that prolong the metabolism of erythromycin (like ] or ]) by interfering with ] (Ray ''et al'' 2004). Hence, erythromycin should not be administered in patients using these drugs, or drugs that also prolong the QT time. Other examples include ] (Seldane, Seldane-D), ] (Hismanal), ] (Propulsid, withdrawn in many countries for prolonging the QT time) and ] (Orap). | |||
| The US price of erythromycin rose three times between 2010 and 2015, from 24 cents per 500mg tablet in 2010 to $8.96 in 2015.<ref>{{cite web | vauthors = Terry K | date = 15 September 2016 | title = Some Generic Drugs See Huge Price Increases | url = https://www.medscape.com/viewarticle/868812 | website = www.medscape.com | access-date = 29 June 2018 | archive-date = 6 April 2017 | archive-url = https://web.archive.org/web/20170406005414/http://www.medscape.com/viewarticle/868812 | url-status = live }}</ref> In 2017, a Kaiser Health News study found that the per-unit cost of dozens of generics doubled or even tripled from 2015 to 2016, increasing spending by the Medicaid program. Due to price increases by drug manufacturers, Medicaid paid on average $2,685,330 more for Erythromycin in 2016 compared to 2015 (not including rebates).<ref>{{cite web | vauthors = Lupkin S | work = Kaiser Health News | date = 14 August 2017 | title = Climbing cost of decades-old drugs threatens to break Medicaid bank | url = http://www.philly.com/philly/health/health-cents/climbing-cost-of-decades-old-drugs-threatens-to-break-medicaid-bank-20170814.html | via = The Philadelphia Inquirer | access-date = 29 June 2018 | archive-date = 29 June 2018 | archive-url = https://web.archive.org/web/20180629050058/http://www.philly.com/philly/health/health-cents/climbing-cost-of-decades-old-drugs-threatens-to-break-medicaid-bank-20170814.html | url-status = live }}</ref> In the US by 2018, generic drug prices had climbed another 5% on average.<ref>{{cite news |vauthors=Marsh T |title=Are Drugs Really Getting More Expensive? Yes. |url=https://www.goodrx.com/blog/are-drugs-getting-more-expensive/ |website=The GoodRx Prescription Savings Blog |access-date=29 June 2018 |date=27 February 2018 |archive-date=23 March 2019 |archive-url=https://web.archive.org/web/20190323095306/https://www.goodrx.com/blog/are-drugs-getting-more-expensive/ |url-status=live }}</ref> | |||
| ==References== | |||
| * Ray WA, Murray KT, Meredith S, Narasimhulu SS, Hall K, Stein CM. Oral Erythromycin and the Risk of Sudden Death from Cardiac Causes. ] 2004;351:1089-96. | |||
| * British National Formulary "BNF 49" March 2005. | |||
| The UK price listed in the ] for erythromycin 500mg tablets was £36.40 for 100 tablets (36.4 pence each) {{asof|August 2024|lc=y}}. This price is not paid by NHS patients: there is no NHS prescription charge in Scotland, Wales, and Northern Ireland; while NHS patients in England without an exemption are liable for a flat rate ]. {{Asof|May 2024}}, that charge was £9.90 for each prescribed medicine.<ref>{{cite web | |||
| ] | |||
| | title = NHS prescription charges from 1 May 2024 | |||
| | website = gov.uk | |||
| | publisher = UK Government | |||
| | date = 5 April 2024 | |||
| | url = https://www.gov.uk/government/news/nhs-prescription-charges-from-1-may-2024 | |||
| | access-date = 25 August 2024 | |||
| |archive-url=https://web.archive.org/web/20240405105001/https://www.gov.uk/government/news/nhs-prescription-charges-from-1-may-2024 | |||
| |archive-date=5 April 2024}}</ref> | |||
| ===Brand names=== | |||
| ] | |||
| Brand names include Robimycin, E-Mycin, E.E.S. Granules, E.E.S.-200, E.E.S.-400, E.E.S.-400 Filmtab, Erymax, Ery-Tab, Eryc, Ranbaxy, Erypar, EryPed, Eryped 200, Eryped 400, Erythrocin Stearate Filmtab, Erythrocot, E-Base, Erythroped, Ilosone, MY-E, Pediamycin, Zineryt, Abboticin, Abboticin-ES, Erycin, PCE Dispertab, Stiemycine, Acnasol, and Tiloryth. | |||
| ] | |||
| ] | |||
| == Veterinary uses == | |||
| ] | |||
| Erythromycin is also used in fishcare for the "''broad spectrum treatment and control of bacterial disease''". Body slime, mouth fungus, furunculosis, bacterial gill illness, and hemorrhagic septicaemia are all examples of bacterial diseases in fish that may be treated and controlled with this therapy. The usage of Erythromycin in fishcare is mainly limited to therapies targeting gram-positive bacteria.<ref>{{cite web|url=https://edis.ifas.ufl.edu/publication/FA084 |title=CIR 84/FA084: Use of Antibiotics in Ornamental Fish Aquaculture|access-date=14 September 2021|archive-date=11 September 2021|archive-url=https://web.archive.org/web/20210911175940/https://edis.ifas.ufl.edu/publication/FA084|url-status=live}}</ref> | |||
| ] | |||
| ] | |||
| == References == | |||
| ] | |||
| {{Reflist}} | |||
| ] | |||
| ] | |||
| {{Acne agents}} | |||
| {{GlycopeptideAntiBio}} | |||
| {{Ion channel modulators}} | |||
| {{Xenobiotic-sensing receptor modulators}} | |||
| {{Portal bar|Medicine}} | |||
| {{Authority control}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 08:50, 21 December 2024
Antibiotic medication "Eryc" redirects here. For the local authority of the East Riding of Yorkshire, see East Riding of Yorkshire Council. Not to be confused with Azithromycin.Pharmaceutical compound
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Eryc, Erythrocin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682381 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous, intramuscular, topical, eye drops |
| Drug class | Macrolide antibiotic |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Depends on the ester type; between 30% and 65% |
| Protein binding | 90% |
| Metabolism | Liver (under 5% excreted unchanged) |
| Elimination half-life | 1.5 hours |
| Excretion | Bile |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.003.673 |
| Chemical and physical data | |
| Formula | C37H67NO13 |
| Molar mass | 733.937 g·mol |
SMILES
| |
InChI
| |
| (verify) | |
Erythromycin is an antibiotic used for the treatment of a number of bacterial infections. This includes respiratory tract infections, skin infections, chlamydia infections, pelvic inflammatory disease, and syphilis. It may also be used during pregnancy to prevent Group B streptococcal infection in the newborn, and to improve delayed stomach emptying. It can be given intravenously and by mouth. An eye ointment is routinely recommended after delivery to prevent eye infections in the newborn.
Common side effects include abdominal cramps, vomiting, and diarrhea. More serious side effects may include Clostridioides difficile colitis, liver problems, prolonged QT, and allergic reactions. It is generally safe in those who are allergic to penicillin. Erythromycin also appears to be safe to use during pregnancy. While generally regarded as safe during breastfeeding, its use by the mother during the first two weeks of life may increase the risk of pyloric stenosis in the baby. This risk also applies if taken directly by the baby during this age. It is in the macrolide family of antibiotics and works by decreasing bacterial protein production.
Erythromycin was first isolated in 1952 from the bacteria Saccharopolyspora erythraea. It is on the World Health Organization's List of Essential Medicines. In 2022, it was the 271st most commonly prescribed medication in the United States, with more than 800,000 prescriptions.
Medical uses
Erythromycin can be used to treat bacteria responsible for causing infections of the skin and upper respiratory tract, including Streptococcus, Staphylococcus, Haemophilus and Corynebacterium genera. The following represents MIC susceptibility data for a few medically significant bacteria:
- Haemophilus influenzae: 0.015 to 256 μg/ml
- Staphylococcus aureus: 0.023 to 1024 μg/ml
- Streptococcus pyogenes: 0.004 to 256 μg/ml
- Corynebacterium minutissimum: 0.015 to 64 μg/ml
It may be useful in treating gastroparesis due to this promotility effect. It has been shown to improve feeding intolerances in those who are critically ill. Intravenous erythromycin may also be used in endoscopy to help clear stomach contents to enhance endoscopic visualization, potentially improving diagnostic accuracy and subsequent management.
Available forms
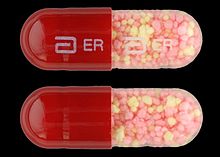
Erythromycin is available in enteric-coated tablets, slow-release capsules, oral suspensions, ophthalmic solutions, ointments, gels, enteric-coated capsules, non enteric-coated tablets, non enteric-coated capsules, and injections. The following erythromycin combinations are available for oral dosage:
- erythromycin base (capsules, tablets)
- erythromycin estolate (capsules, oral suspension, tablets), contraindicated during pregnancy
- erythromycin ethylsuccinate (oral suspension, tablets)
- erythromycin stearate (oral suspension, tablets)
For injection, the available combinations are:
- erythromycin gluceptate
- erythromycin lactobionate
For ophthalmic use:
- erythromycin base (ointment)
Adverse effects
Gastrointestinal disturbances, such as diarrhea, nausea, abdominal pain, and vomiting, are very common because erythromycin is a motilin agonist.
More serious side effects include arrhythmia with prolonged QT intervals, including torsades de pointes, and reversible deafness. Allergic reactions range from urticaria to anaphylaxis. Cholestasis and Stevens–Johnson syndrome are some other rare side effects that may occur.
Studies have shown evidence both for and against the association of pyloric stenosis and exposure to erythromycin prenatally and postnatally. Exposure to erythromycin (especially long courses at antimicrobial doses, and also through breastfeeding) has been linked to an increased probability of pyloric stenosis in young infants. Erythromycin used for feeding intolerance in young infants has not been associated with hypertrophic pyloric stenosis.
Erythromycin estolate has been associated with reversible hepatotoxicity in pregnant women in the form of elevated serum glutamic-oxaloacetic transaminase and is not recommended during pregnancy. Some evidence suggests similar hepatotoxicity in other populations.
It can also affect the central nervous system, causing psychotic reactions, nightmares, and night sweats.
Interactions
Erythromycin is metabolized by enzymes of the cytochrome P450 system, in particular, by isozymes of the CYP3A superfamily. The activity of the CYP3A enzymes can be induced or inhibited by certain drugs (e.g., dexamethasone), which can cause it to affect the metabolism of many different drugs, including erythromycin. If other CYP3A substrates — drugs that are broken down by CYP3A — such as simvastatin (Zocor), lovastatin (Mevacor), or atorvastatin (Lipitor) — are taken concomitantly with erythromycin, levels of the substrates increase, often causing adverse effects. A noted drug interaction involves erythromycin and simvastatin, resulting in increased simvastatin levels and the potential for rhabdomyolysis. Another group of CYP3A4 substrates are drugs used for migraine such as ergotamine and dihydroergotamine; their adverse effects may be more pronounced if erythromycin is associated.
Earlier case reports on sudden death prompted a study on a large cohort that confirmed a link between erythromycin, ventricular tachycardia, and sudden cardiac death in patients also taking drugs that prolong the metabolism of erythromycin (like verapamil or diltiazem) by interfering with CYP3A4. Hence, erythromycin should not be administered to people using these drugs, or drugs that also prolong the QT interval. Other examples include terfenadine (Seldane, Seldane-D), astemizole (Hismanal), cisapride (Propulsid, withdrawn in many countries for prolonging the QT time) and pimozide (Orap). Interactions with theophylline, which is used mostly in asthma, were also shown.
Erythromycin and doxycycline can have a synergistic effect when combined and kill bacteria (E. coli) with a higher potency than the sum of the two drugs together. This synergistic relationship is only temporary. After approximately 72 hours, the relationship shifts to become antagonistic, whereby a 50/50 combination of the two drugs kills less bacteria than if the two drugs were administered separately.
It may alter the effectiveness of combined oral contraceptive pills because of its effect on the gut flora. A review found that when erythromycin was given with certain oral contraceptives, there was an increase in the maximum serum concentrations and AUC of estradiol and dienogest.
Erythromycin is an inhibitor of the cytochrome P450 system, which means it can have a rapid effect on levels of other drugs metabolised by this system, e.g., warfarin.
Pharmacology
Mechanism of action
Erythromycin displays bacteriostatic activity or inhibits growth of bacteria, especially at higher concentrations. By binding to the 50s subunit of the bacterial rRNA complex, protein synthesis and subsequent structure and function processes critical for life or replication are inhibited. Erythromycin interferes with aminoacyl translocation, preventing the transfer of the tRNA bound at the A site of the rRNA complex to the P site of the rRNA complex. Without this translocation, the A site remains occupied, thus the addition of an incoming tRNA and its attached amino acid to the nascent polypeptide chain is inhibited. This interferes with the production of functionally useful proteins, which is the basis of this antimicrobial action.
Erythromycin increases gut motility by binding to motilin receptor, thus it is a motilin receptor agonist in addition to its antimicrobial properties. It can be therefore administered intravenously as a stomach emptying stimulant.
Pharmacokinetics
Erythromycin is easily inactivated by gastric acid; therefore, all orally administered formulations are given as either enteric-coated or more-stable salts or esters, such as erythromycin ethylsuccinate. Erythromycin is very rapidly absorbed, and diffuses into most tissues and phagocytes. Due to the high concentration in phagocytes, erythromycin is actively transported to the site of infection, where, during active phagocytosis, large concentrations of erythromycin are released.
Metabolism
Most of erythromycin is metabolised by demethylation in the liver by the hepatic enzyme CYP3A4. Its main elimination route is in the bile with little renal excretion, 2%–15% unchanged drug. Erythromycin's elimination half-life ranges between 1.5 and 2.0 hours and is between 5 and 6 hours in patients with end-stage renal disease. Erythromycin levels peak in the serum 4 hours after dosing; ethylsuccinate peaks 0.5–2.5 hours after dosing, but can be delayed if digested with food.
Erythromycin crosses the placenta and enters breast milk. The American Association of Pediatrics determined erythromycin is safe to take while breastfeeding. Absorption in pregnant patients has been shown to be variable, frequently resulting in levels lower than in nonpregnant patients.
Chemistry
Composition
Standard-grade erythromycin is primarily composed of four related compounds known as erythromycins A, B, C, and D. Each of these compounds can be present in varying amounts and can differ by lot. Erythromycin A has been found to have the most antibacterial activity, followed by erythromycin B. Erythromycins C and D are about half as active as erythromycin A. Some of these related compounds have been purified and can be studied and researched individually.
Synthesis
Over the three decades after the discovery of erythromycin A and its activity as an antimicrobial, many attempts were made to synthesize it in the laboratory. The presence of 10 stereogenic carbons and several points of distinct substitution has made the total synthesis of erythromycin A a formidable task. Complete syntheses of erythromycins’ related structures and precursors such as 6-deoxyerythronolide B have been accomplished, giving way to possible syntheses of different erythromycins and other macrolide antimicrobials. Woodward successfully completed the synthesis of erythromycin A, which was published in 1981.
History
In 1949 Abelardo B. Aguilar, a Filipino scientist, sent some soil samples to his employer at Eli Lilly. Aguilar managed to isolate erythromycin from the metabolic products of a strain of Streptomyces erythreus (designation changed to Saccharopolyspora erythraea) found in the samples. Aguilar received no further credit or compensation for his discovery.
The scientist was allegedly promised a trip to the company's manufacturing plant in Indianapolis, but it was never fulfilled. In a letter to the company's president, Aguilar wrote: “A leave of absence is all I ask as I do not wish to sever my connection with a great company which has given me wonderful breaks in life.” The request was not granted.
Aguilar reached out to Eli Lilly again in 1993, requesting royalties from sales of the drug over the years, intending to use them to put up a foundation for poor and sickly Filipinos. This request was also denied. He died in September of the same year.
Lilly filed for patent protection on the compound which was granted in 1953. The product was launched commercially in 1952 under the brand name Ilosone (after the Philippine region of Iloilo where it was originally collected). Erythromycin was formerly also called Ilotycin.
The antibiotic clarithromycin was invented by scientists at the Japanese drug company Taisho Pharmaceutical in the 1970s as a result of their efforts to overcome the acid instability of erythromycin.
Society and culture
Economics
It is available as a generic medication.
In the United States, in 2014, the price increased to seven dollars per 500mg tablet.
The US price of erythromycin rose three times between 2010 and 2015, from 24 cents per 500mg tablet in 2010 to $8.96 in 2015. In 2017, a Kaiser Health News study found that the per-unit cost of dozens of generics doubled or even tripled from 2015 to 2016, increasing spending by the Medicaid program. Due to price increases by drug manufacturers, Medicaid paid on average $2,685,330 more for Erythromycin in 2016 compared to 2015 (not including rebates). In the US by 2018, generic drug prices had climbed another 5% on average.
The UK price listed in the BNF for erythromycin 500mg tablets was £36.40 for 100 tablets (36.4 pence each) as of August 2024. This price is not paid by NHS patients: there is no NHS prescription charge in Scotland, Wales, and Northern Ireland; while NHS patients in England without an exemption are liable for a flat rate prescription charge. As of May 2024, that charge was £9.90 for each prescribed medicine.
Brand names
Brand names include Robimycin, E-Mycin, E.E.S. Granules, E.E.S.-200, E.E.S.-400, E.E.S.-400 Filmtab, Erymax, Ery-Tab, Eryc, Ranbaxy, Erypar, EryPed, Eryped 200, Eryped 400, Erythrocin Stearate Filmtab, Erythrocot, E-Base, Erythroped, Ilosone, MY-E, Pediamycin, Zineryt, Abboticin, Abboticin-ES, Erycin, PCE Dispertab, Stiemycine, Acnasol, and Tiloryth.
Veterinary uses
Erythromycin is also used in fishcare for the "broad spectrum treatment and control of bacterial disease". Body slime, mouth fungus, furunculosis, bacterial gill illness, and hemorrhagic septicaemia are all examples of bacterial diseases in fish that may be treated and controlled with this therapy. The usage of Erythromycin in fishcare is mainly limited to therapies targeting gram-positive bacteria.
References
- ^ "Erythromycin". The American Society of Health-System Pharmacists. Archived from the original on 6 September 2015. Retrieved 1 August 2015.
- ^ "Prescribing medicines in pregnancy database". Australian Government. 23 August 2015. Archived from the original on 8 April 2014.
- Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L (January 2013). "Clinical guideline: management of gastroparesis". The American Journal of Gastroenterology. 108 (1): 18–37, quiz 38. doi:10.1038/ajg.2012.373. PMC 3722580. PMID 23147521.
- Matejcek A, Goldman RD (November 2013). "Treatment and prevention of ophthalmia neonatorum". Canadian Family Physician. 59 (11): 1187–90. PMC 3828094. PMID 24235191.
- ^ Hamilton RJ (2013). Tarascon pocket pharmacopoeia (2013 delux lab-coat ed., 14th ed.). : Jones & Bartlett Learning. p. 72. ISBN 9781449673611. Archived from the original on 1 August 2020. Retrieved 9 September 2017.
- Kong YL, Tey HL (June 2013). "Treatment of acne vulgaris during pregnancy and lactation". Drugs. 73 (8): 779–87. doi:10.1007/s40265-013-0060-0. PMID 23657872. S2CID 45531743.
- Maheshwai N (March 2007). "Are young infants treated with erythromycin at risk for developing hypertrophic pyloric stenosis?". Archives of Disease in Childhood. 92 (3): 271–3. doi:10.1136/adc.2006.110007. PMC 2083424. PMID 17337692. Archived from the original on 7 November 2012.
- Vedas JC (2000). Biosynthesis : polyketides and vitamins. Berlin : Springer. p. 52. ISBN 9783540669692. Archived from the original on 1 August 2020. Retrieved 9 September 2017.
- World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- "Erythromycin Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ "Erythromycin Susceptibility and Minimum Inhibitory Concentration (MIC) Data" (PDF). TOKU-E. Archived (PDF) from the original on 9 May 2015. Retrieved 26 February 2014.
- Lewis K, Alqahtani Z, Mcintyre L, Almenawer S, Alshamsi F, Rhodes A, et al. (August 2016). "The efficacy and safety of prokinetic agents in critically ill patients receiving enteral nutrition: a systematic review and meta-analysis of randomized trials". Critical Care. 20 (1): 259. doi:10.1186/s13054-016-1441-z. PMC 4986344. PMID 27527069.
- Laine L, Barkun AN, Saltzman JR, Martel M, Leontiadis GI (May 2021). "ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding". The American Journal of Gastroenterology. 116 (5): 899–917. doi:10.14309/ajg.0000000000001245. PMID 33929377.
- ^ "Erythromycin Oral, Parenteral Advanced Patient Information". Drugs.com. Archived from the original on 30 November 2009.
- Workowski KA, Berman SM (August 2006). "Sexually transmitted diseases treatment guidelines, 2006". MMWR: Recommendations and Reports. 55 (RR-11): 1–94. PMID 16888612. Archived from the original on 11 February 2010.
- Weber FH, Richards RD, McCallum RW (April 1993). "Erythromycin: a motilin agonist and gastrointestinal prokinetic agent". The American Journal of Gastroenterology. 88 (4): 485–90. PMID 8470625.
- Aronson JK, ed. (2016). "Erythromycin". Meyler's Side Effects of Drugs (Sixteenth ed.). Elsevier. pp. 99–108. doi:10.1016/B978-0-444-53717-1.00698-3. ISBN 9780444537164.
- ^ Briggs GG, Freeman RK, Yaffe SJ (2011). "Erythromycin". Drugs in pregnancy and lactation : a reference guide to fetal and neonatal risk (9th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 978-1-60831-708-0. Archived from the original on 23 May 2022. Retrieved 20 October 2021.
- ^ Maheshwai N (March 2007). "Are young infants treated with erythromycin at risk for developing hypertrophic pyloric stenosis?". Archives of Disease in Childhood. 92 (3): 271–3. doi:10.1136/adc.2006.110007. PMC 2083424. PMID 17337692.
- Lund M, Pasternak B, Davidsen RB, Feenstra B, Krogh C, Diaz LJ, et al. (March 2014). "Use of macrolides in mother and child and risk of infantile hypertrophic pyloric stenosis: nationwide cohort study". BMJ. 348: g1908. doi:10.1136/bmj.g1908. PMC 3949411. PMID 24618148.
- McCormack WM, George H, Donner A, Kodgis LF, Alpert S, Lowe EW, et al. (November 1977). "Hepatotoxicity of erythromycin estolate during pregnancy". Antimicrobial Agents and Chemotherapy. 12 (5): 630–5. doi:10.1128/AAC.12.5.630. PMC 429989. PMID 21610.
- ^ "Erythromycine". Belgisch Centrum voor Farmacotherapeutische Informatie. Archived from the original on 6 October 2015.
- Hunt CM, Watkins PB, Saenger P, Stave GM, Barlascini N, Watlington CO, et al. (January 1992). "Heterogeneity of CYP3A isoforms metabolizing erythromycin and cortisol" (PDF). Clinical Pharmacology and Therapeutics. 51 (1): 18–23. doi:10.1038/clpt.1992.3. hdl:2027.42/109905. PMID 1732074. S2CID 28056649. Archived from the original on 28 August 2021. Retrieved 29 August 2019.
- Ray WA, Murray KT, Meredith S, Narasimhulu SS, Hall K, Stein CM (September 2004). "Oral erythromycin and the risk of sudden death from cardiac causes". The New England Journal of Medicine. 351 (11): 1089–96. doi:10.1056/NEJMoa040582. PMID 15356306.
- "Drug Interactions between erythromycin and terfenadine". Drugs.com. Retrieved 21 December 2023.
- "Drug Interactions between astemizole and erythromycin". Drugs.com. Retrieved 21 December 2023.
- Michalets EL, Williams CR (July 2000). "Drug interactions with cisapride: clinical implications". Clinical Pharmacokinetics. 39 (1): 49–75. doi:10.2165/00003088-200039010-00004. PMID 10926350. S2CID 41704853.
- "Erythromycin Interactions". GPnotebook. 20 December 2020. Archived from the original on 21 December 2023. Retrieved 21 December 2023.
- "Drug Interactions between erythromycin and theophylline". Drugs.com. Archived from the original on 21 December 2023. Retrieved 21 December 2023.
- Pena-Miller R, Laehnemann D, Jansen G, Fuentes-Hernandez A, Rosenstiel P, Schulenburg H, et al. (23 April 2013). "When the most potent combination of antibiotics selects for the greatest bacterial load: the smile-frown transition". PLOS Biology. 11 (4): e1001540. doi:10.1371/journal.pbio.1001540. PMC 3635860. PMID 23630452.
- Blode H, Zeun S, Parke S, Zimmermann T, Rohde B, Mellinger U, et al. (October 2012). "Evaluation of the effects of rifampicin, ketoconazole and erythromycin on the steady-state pharmacokinetics of the components of a novel oral contraceptive containing estradiol valerate and dienogest in healthy postmenopausal women". Contraception. 86 (4): 337–44. doi:10.1016/j.contraception.2012.01.010. PMID 22445438. Archived from the original on 28 August 2021. Retrieved 2 August 2019.
- Simmons KB, Haddad LB, Nanda K, Curtis KM (January 2018). "Drug interactions between non-rifamycin antibiotics and hormonal contraception: a systematic review". American Journal of Obstetrics and Gynecology. 218 (1): 88–97.e14. doi:10.1016/j.ajog.2017.07.003. PMID 28694152. S2CID 36567820. Archived from the original on 28 August 2021. Retrieved 2 August 2019.
- Westphal JF (October 2000). "Macrolide - induced clinically relevant drug interactions with cytochrome P-450A (CYP) 3A4: an update focused on clarithromycin, azithromycin and dirithromycin". British Journal of Clinical Pharmacology. 50 (4): 285–295. doi:10.1046/j.1365-2125.2000.00261.x. PMC 2015000. PMID 11012550.
- ^ Trevor AJ, Katzung BG, Masters SB, eds. (2010). "Section VIII: Chemotherapeutic Drugs; Chapter 44: Chloramphenicol, Tetracyclines, Macrolides, Clindamycin, & Streptogramins". Katzung & Trevor's Pharmacology: Examination & Board Review (9th ed.). New York: McGraw-Hill Medical. pp. 389–396. ISBN 978-0-07-170155-6.
- "Erythromycin". Sigma-Aldrich. Retrieved 21 December 2023.
- Parkman HP (2021). "Chapter 24 - Prokinetic agents for gastroparesis". Gastroparesis: Pathophysiology, Clinical Presentation, Diagnosis and Treatment. Academic Press. pp. 323–339. doi:10.1016/B978-0-12-818586-5.00024-7. ISBN 9780128185865.
Erythromycin has prokinetic effects because it is a motilin receptor agonist in addition to being an antibiotic. When given intravenously, erythromycin is a potent stimulant of gastric emptying among the available prokinetic drugs.
- Lebel M (May 1993). "Pharmacokinetic properties of clarithromycin: A comparison with erythromycin and azithromycin". The Canadian Journal of Infectious Diseases. 4 (3): 148–152. doi:10.1155/1993/168061. PMC 3250788. PMID 22346438.
- Edmunds MW, Mayhew MS (2009). "Chapter 61: Macrolides". Pharmacology for the primary care provider (Third ed.). Saint Louis, Missouri: Elsevier Health Sciences. pp. 658–662 (661). ISBN 978-0-323-06316-6. Archived from the original on 23 May 2022. Retrieved 3 March 2022.; Kirst HA, Sides GD (1993). "Chapter 28: Erythromycin". In Bryskier A, Butzler JP, Neu HC, Tulkens (eds.). The Macrolides. Oxford UK: Arnette-Blackwell.
- American Academy of Pediatrics Committee on Drugs (September 2001). "Transfer of drugs and other chemicals into human milk". Pediatrics. 108 (3): 776–89. doi:10.1542/peds.108.3.776. PMID 11533352.
- Philipson A, Sabath LD, Charles D (January 1976). "Erythromycin and clindamycin absorption and elimination in pregnant women". Clinical Pharmacology and Therapeutics. 19 (1): 68–77. doi:10.1002/cpt197619168. PMID 1245094. S2CID 7573420.
- Kibwage IO, Hoogmartens J, Roets E, Vanderhaeghe H, Verbist L, Dubost M, et al. (November 1985). "Antibacterial activities of erythromycins A, B, C, and D and some of their derivatives". Antimicrobial Agents and Chemotherapy. 28 (5): 630–3. doi:10.1128/aac.28.5.630. PMC 176346. PMID 4091529.
- Pal S (2006). "A journey across the sequential development of macrolides and ketolides related to erythromycin". Tetrahedron. 62 (14): 3171–3200. doi:10.1016/j.tet.2005.11.064.
- Evans DA, Kim AS (1997). "Synthesis of 6-Deoxyerythronolide B. Implementation of a General Strategy for the Synthesis of Macrolide Antibiotics". Tetrahedron Lett. 38: 53–56. doi:10.1016/S0040-4039(96)02258-7.
- Woodward RB, Logusch E, Nambiar KP, Sakan K, Ward DE, Au-Yeung BW, et al. (June 1981). "Asymmetric Total Synthesis of Erythromycin. 1. Synthesis of an Erythronolide A Seco Acid Derivative via Asymmetric Induction". Journal of the American Chemical Society. 103 (11): 3210–3213. Bibcode:1981JAChS.103.3210W. doi:10.1021/ja00401a049.
- Woodward RB, Au-Yeung BW, Balaram P, Browne LJ, Ward DE, Au-Yeung BW, et al. (1981). "Asymmetric Total Synthesis of Erythromycin. 2. Synthesis of an Erythronolide A Lactone System". Journal of the American Chemical Society. 103 (11): 3213–3215. Bibcode:1981JAChS.103.3213W. doi:10.1021/ja00401a050.
- Woodward RB, Logusch E, Nambiar KP, Sakan K, Ward DE, Au-Yeung BW, et al. (June 1981). "Asymmetric Total Synthesis of Erythromycin. 3. Total Synthesis of Erythromycin". Journal of the American Chemical Society. 103 (11): 3215–3217. Bibcode:1981JAChS.103.3215W. doi:10.1021/ja00401a051.
- Tan ML (30 August 2019). "Drugs and rights". Philippine Daily Inquirer. Archived from the original on 28 February 2021. Retrieved 4 November 2021.
- Tan ML (30 August 2019). "Drugs and rights". Philippine Daily Inquirer. Retrieved 21 December 2023.
- ^ Hibionada FF. "Remembering the battle of Dr. Abelardo Aguilar: Cure for millions, deprived of millions". The News Today. Archived from the original on 18 September 2021. Retrieved 22 September 2015.
- US 2653899, Bunch RL, Mcguire JM, "Erythromycin, its salts, and method of preparation", published 29 September 1953, assigned to Eli Lilly and Company.
- Greenwood D (2008). Antimicrobial drugs: chronicle of a twentieth century medical triumph. New York: Oxford university press. p. 239. ISBN 978-0-19-953484-5.
- Stahl S (26 September 2014). "Health: Generic Drugs Prices Increasing". CBS Philadelphia. Archived from the original on 9 April 2016. Retrieved 24 March 2016.
- Terry K (15 September 2016). "Some Generic Drugs See Huge Price Increases". www.medscape.com. Archived from the original on 6 April 2017. Retrieved 29 June 2018.
- Lupkin S (14 August 2017). "Climbing cost of decades-old drugs threatens to break Medicaid bank". Kaiser Health News. Archived from the original on 29 June 2018. Retrieved 29 June 2018 – via The Philadelphia Inquirer.
- Marsh T (27 February 2018). "Are Drugs Really Getting More Expensive? Yes". The GoodRx Prescription Savings Blog. Archived from the original on 23 March 2019. Retrieved 29 June 2018.
- "NHS prescription charges from 1 May 2024". gov.uk. UK Government. 5 April 2024. Archived from the original on 5 April 2024. Retrieved 25 August 2024.
- "CIR 84/FA084: Use of Antibiotics in Ornamental Fish Aquaculture". Archived from the original on 11 September 2021. Retrieved 14 September 2021.
| Acne-treating agents (D10) | |
|---|---|
| Antibacterial | |
| Keratolytic | |
| Anti-inflammatory | |
| Antibiotics | |
| Hormonal | |
| Retinoids | |
| Other | |
| Combinations | |
| |
| Antibacterials that inhibit protein synthesis (J01A, J01B, J01F, J01G, QJ01XQ) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30S |
| ||||||||||||||
| 50S | |||||||||||||||
| |||||||||||||||
| Ion channel modulators | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Calcium |
| ||||||||||||||||||||||||
| Potassium |
| ||||||||||||||||||||||||
| Sodium |
| ||||||||||||||||||||||||
| Chloride |
| ||||||||||||||||||||||||
| Others |
| ||||||||||||||||||||||||
| See also: Receptor/signaling modulators • Transient receptor potential channel modulators | |||||||||||||||||||||||||
| Xenobiotic-sensing receptor modulators | |
|---|---|
| CARTooltip Constitutive androstane receptor |
|
| PXRTooltip Pregnane X receptor |
|
| |